CHAPTER 34 Transversus abdominis plane block
Clinical anatomy
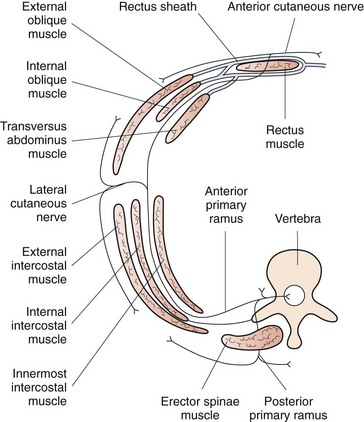
The sensory innervation of the abdominal wall is derived from the sixth thoracic nerve to the first lumbar nerve (Fig. 34.1). The nerves arise from the ventral rami of their respective nerve roots and travel anteriorly in a groove beneath the respective ribs to lie between the internal intercostal muscle and the innermost intercostal muscle. The intercostal nerve gives a sensory branch at the mid-axillary line, which provides variable innervation from the posterior axillary line anteriorly. The nerve continues forward as the anterior cutaneous branch, which enters the transversus abdominis plane of the anterior abdominal wall and supplies the skin, muscles and parietal peritoneum in the abdomen (Fig. 34.2). The transversus abdominis plane (TAP) lies between the internal oblique and transversus abdominis muscles, and forms a connective tissue conduit through which the ventral rami of T6 to L1 travel. Deposition of local anesthetic solution in the TAP permits abdominal wall sensory blockade.
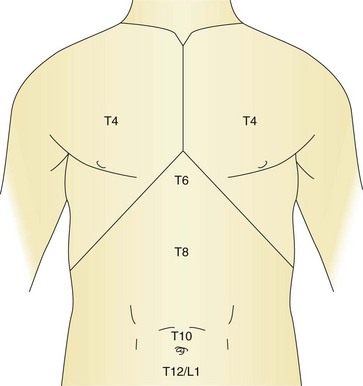
Figure 34.1 The dermatomal levels and corresponding relevant anatomical surface landmarks are illustrated.
From Harmon D, et al. Perioperative diagnostic and interventional ultrasound with DVD. Elsevier, Saunders; 2008.
Surface anatomy
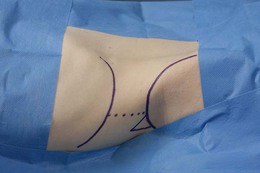
The surface anatomical landmarks for this block are: the iliac crest, the mid-axillary line and the costal margin. The needle insertion point is at the apex of the Lumbar Triangle of Petit, which is formed by the external oblique muscle anteriorly, the latissimus dorsi muscle posteriorly, and the iliac crest inferiorly (Fig. 34.3).
Sonoanatomy
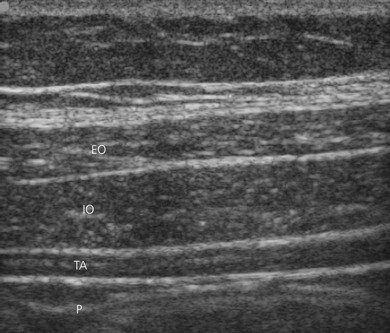
The muscles of the anterior abdominal wall are readily visible as three distinct layers (external oblique, internal oblique, transversus abdominis) (Fig. 34.4). The muscle layers are seen as marbled transverse structures surrounded by bright hyperechoic fascial coverings. The target for this block is the space between the internal oblique muscle and the transversus abdominis muscle at the level of the apex of the Lumbar Triangle of Petit.
Landmark-based approach
The block tray is set up with antibacterial solution and swabs, block needle and local anesthetic injectate. With the patient in a supine position, the operator stands opposite the side to be blocked and the iliac crest is palpated from anterior to posterior. The needle insertion point is at the apex of the Lumbar Triangle of Petit cephalad to the iliac crest, behind the mid-axillary line. The skin is disinfected with antiseptic solution and draped. The skin is pierced by the regional anesthesia needle (18-G Tuohy needle connected to sterile extension tubing). The needle is advanced at right angles to the skin, and a ’pop’ sensation is appreciated as the external oblique muscle is traversed (Fig. 34.5). Further advancement results in a second ‘pop,’ which signals entry to the transversus abdominis fascial plane. After aspiration to exclude vascular puncture, 0.3 mL/kg of local anesthetic (usually 0.25% levobupivacaine to a maximum dose of 2 mg/kg) is injected into the space (repeated on the other side, if indicated).
< div class='tao-gold-member'>

Full access? Get Clinical Tree