Fig. 7.1
Skin incision for a right inguinal hernia starting halfway along the line between the superior anterior iliac spine and the pubic tubercle over 3 cm to the medial side
7.2.5 7.2.5 Superficial Dissection
The skin, subcutaneous fat, and Scarpa’s fascia are opened down to the aponeurosis of the external oblique muscle and the external orifice can be visualized. The external oblique aponeurosis is then opened, taking caution not to harm the ilioinguinal nerve, and the inguinal canal is exposed (Fig. 7.2).
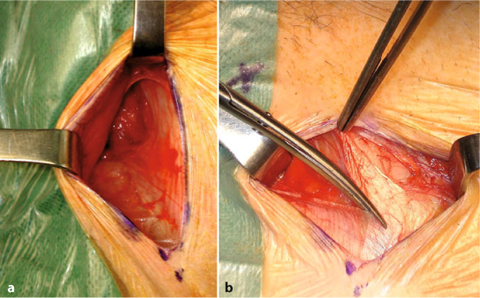
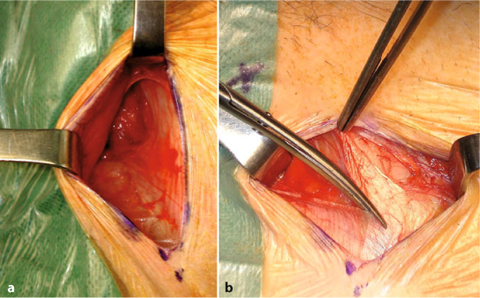
Fig. 7.2
a Superficial dissection of the subcutaneous fat and Scarpa’s fascia. b Incision of the aponeurosis of the external oblique muscle
An important modification compared to the former description of this technique [7] is not to perform extensive dissection to locate the hernia defect, but, if possible, to let the patient strain or cough and in that way visualize the defect. There is absolutely no reason to completely section the cremasteric muscle and to skeletonise the cord structures. This may only increase the harm done to the inguinal nerves.
7.2.6 7.2.6 Approach for Indirect Hernias (Fig. 7.3)
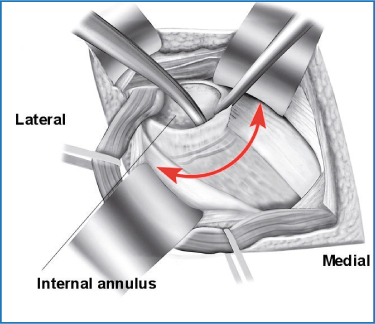
Fig. 7.3
The approach for entering the preperitoneal space in case of an indirect hernia
In the case of an indirect hernia, the sac is completely dissected until its entrance through the internal orifice. At the level of the orifice, the preperitoneal fat can now be seen. It is important at this time to visualize the epigastric vessels before entering the preperitoneal space. The posterior sheet of the transversalis fascia should be opened at the level of the dilated deep internal ring to enter the space of Bogros. From that moment on, the epigastric vessels will be retracted softly upwards. After palpation of both Cooper’s ligament and the pubic bone to ensure the dissection will be done in the right avascular preperitoneal plane, gauze can be introduced into the preperitoneal space towards the space of Retzius. By doing so, most of the dissection medially will be performed bluntly. The index finger can now be introduced medially performing further dissection, first cranially, leaving the preperitoneal fat attached to the peritoneum. The fatty tissue is then swept off from the iliopubic branch of the iliac bone, the pubic symphysis, the rectus muscle and the transverse muscle in succession, thus enlarging the preperitoneal space to accommodate the mesh.
The next step, crucial for a good accommodation of the mesh in the preperitoneal pocket, is to parietalize the peritoneum off the cord structures as far as possible, even inside the abdominal cavity where the spermatic cord separates from the spermatic vessels (Fig. 7.4). In very obese patients this can be difficult to achieve through a 3 cm incision. However, especially for larger indirect hernias this is essential for preventing later recurrences. By doing this there is no need to create a new internal orifice.
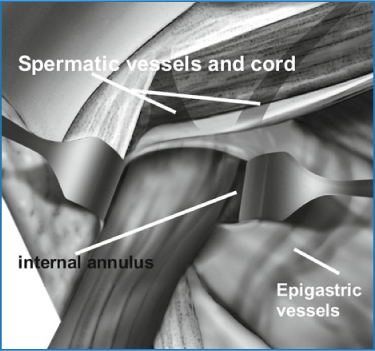
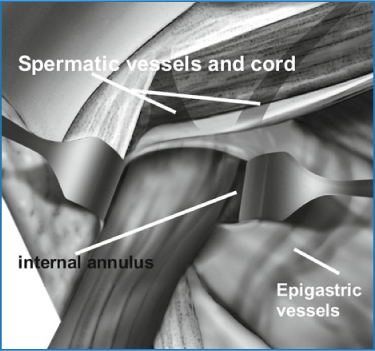
Fig. 7.4
Complete parietalization of the cord structures
A last critical point in using this technique is to obtain a sufficient pocket at the lateral side of the internal orifice. To facilitate this part of the dissection, it can sometimes be helpful to introduce gauze laterally. One should only be satisfied with the created pocket once the index finger can reach the superior anterior iliac spine easily.
7.2.7 7.2.7 Approach for Direct or Femoral Hernias (Fig. 7.5)
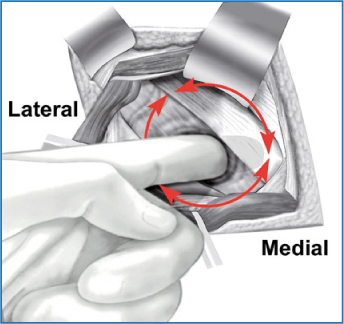
Fig. 7.5
The approach for entering the preperitoneal space in the case of a direct hernia defect
In case the surgeon feels more comfortable to completely dissect the direct hernia sac, in the absence of an indirect component, he can incise the direct hernia sac (both layers of the transversalis fascia have to be incised) at its base circumferentially. The preperitoneal fat will then immediately be visualized and you can enter the preperitoneal space. Again, the epigastric vessels should be identified, on the lateral side of the defect in this situation, and protected by a retractor upwards. The preperitoneal space is created in the same manner as in the indirect hernia. In cases of a femoral or obturator hernia, the transversalis fascia has to be incised from the internal ring.
In our experience, we prefer handling all types of hernia through the deep internal ring as it is very easy to reduce direct hernias by approaching these from the lateral side, while reduction and dissection of an indirect hernia sac might be more difficult. In the case of a combination of an indirect and direct hernia, or when the direct component is difficult to reduce, one could also prefer to open the transversalis fascia over a few centimetres through the deep inguinal ring.
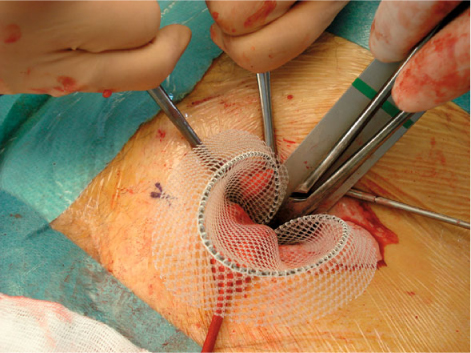
7.2.8 7.2.8 Introduction of the Mesh and Adequate Mesh Placement
After creation of the appropriate pocket, a malleable flat retractor is introduced medially to recline peritoneum, preperitoneal fat and the lateral aspect of the bladder. Introduction of the mesh can now be performed, by sliding the mesh over the malleable retractor.
The use of a mesh with a memory facilitates the introduction and fast placement. Different meshes are available. The Polysoft mesh consists of a polypropylene mesh with a resorbable memory ring. It has an oval shape and exists in two sizes: medium (14 × 7.5 cm) and large (16 × 9.5 cm). Laterally, a notch has been manufactured in the mesh to allow proper deployment over the iliac vessels. The main disadvantage of this mesh is the interrupted memory at the lateral side, which limits the complete deployment of the mesh in some cases, which might lead to pain or long-term recurrences.
Another possible mesh frame is the Rebound HRD shield, which consists of a large polypropylene mesh with a non-resorbable nitinol frame. It is also available in two sizes: small (14.93 × 10.31 cm) and large (16 × 11 cm). This mesh has a continuous memory ring that facilitates lateral flat mesh placement.
The medial side of the mesh is grasped with a blunt clamp, and the mesh is introduced in the direction of the pubis, up to the tendon of the rectus muscle, keeping the malleable retractor still in place (Fig 7.6). The clamp can then be removed from the mesh as well as the malleable retractor. Although the created pocket is medially large enough to do so, it is important not to introduce the mesh too medially. Especially for indirect hernias, an adequate overlap of the mesh lateral to the deep internal ring is necessary.