Fig. 12.1
Operating room set-up
12.7 12.7 Surgical Technique
12.7.1 12.7.1 Entering and creating the Preperitoneal Space
There are few techniques to enter and create the preperitoneal space. A 10-mm vertical infraumbilical incision is first made. Subcutaneous tissue is bluntly dissected to expose the anterior rectus sheath using (2) S-retractors (Fig. 12.2). The anterior rectus sheath is then incised, lateral from the midline, on the ipsilateral side of the hernia. This will avoid the linea alba and accidentally entering the peritoneal cavity. Then the rectus muscle is retracted laterally to expose the posterior rectus sheath (Fig. 12.3).

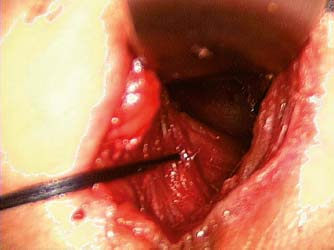

Fig. 12.2
Anterior rectus sheath exposed using S-retractors
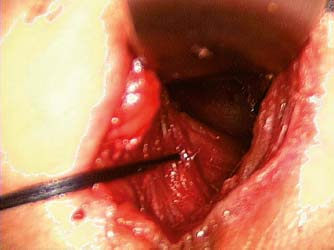
Fig. 12.3
Rectus muscle retracted laterally
Once the preperitoneal plane is entered, there are a few techniques to create the space: 1. the optical ballon dissector; 2. the Veress’ needle technique; 3. the most common blunt dissection. Using the trocar with an optical ballon dissector, the space is created by inflating the balloon under vision (Fig. 12.4). This is the plane one should maintain and create up to the symphysis pubis using a gauze, finger or a dissecting balloon, depending on the preference and expertise of the surgeon. A Hasson’s trocar is then inserted and the plane is confirmed by inserting a 30-degree trocar. The rectus muscle should be visualized in the anterior area to be in the right plane. Insufflation is done with carbon dioxide at 8–12 mmHg.
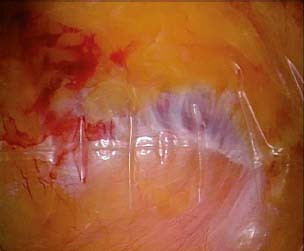
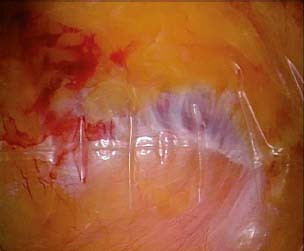
Fig. 12.4
Balloon dissector
Two 5-mm trocars are then inserted at the midline under direct vision to prevent any injury to the bladder, peritoneum, or bowels. The first 5-mm trocar is placed 3 finger breadths above the symphysis pubis. The second 5-mm trocar is then placed in between the Hasson’s trocar and the first 5-mm trocar (Fig 12.5).
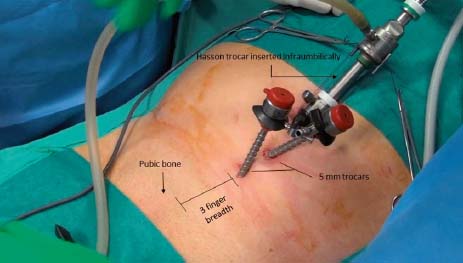
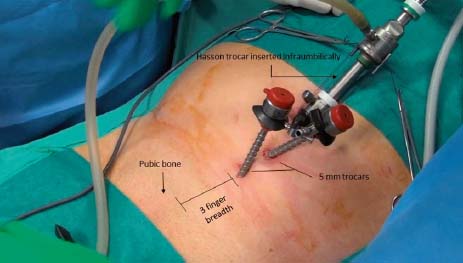
Fig. 12.5
Trocar placement
12.7.2 12.7.2 Medial Dissection (Space of Retzius or Prevesical Space)
Once all the working ports are inserted, using two atraumatic graspers, the dissection is conducted along the midline, below the rectus muscle and towards the pubis arch. The dissection should go 2 cm beyond the symphysis pubis to the obturator fossa to avoid missing any obturator hernia and to allow the medial lower corner of the mesh to be fixated once the space is deflated (Fig. 12.6). The limits of the dissection are: medially, 1–2 cm beyond the midline and below the pubis arch; inferiorly until the peritoneal refection is identified at the border with the retroperitoneal space.
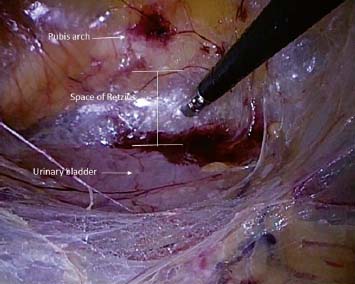
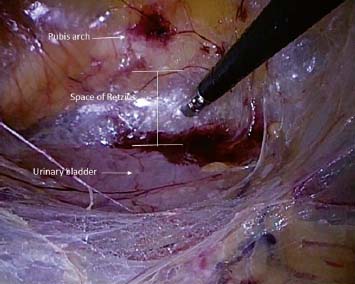
Fig. 12.6
Space of Retzius
12.7.3 12.7.3 Lateral Dissection (Lateral Space of Bogros)
Moving towards the anterior superior iliac spine (ASIS), in a surgical plane that is below the inferior epigastric vessels (IEV) and above the peritoneum, the lateral dissection is made. This plane is confined by the two layers of the fascia transversalis. The dissection is continued by pushing down the peritoneum until the psoas muscle can be seen. The lateral space of Bogros is delineated and cleaned all the way up to the anterior superior iliac spine. Attention should be made to avoid dissecting further laterally, beyond the lumbar fascia in the so-called “lateral triangle of pain”. This will prevent injury to the latero-cutaneous and genitofemoral nerves. The thin layer of fat covering the lateral fascia should be preserved and not skeletonized; similarly, energy and diathermy should not be used at this level. (Figs. 12.7 and 12.8). The limits of the lateral dissection are inferiorly the psoas muscle, superiorly the ASIS and cranially the arcuate line.
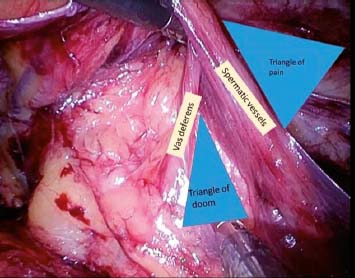
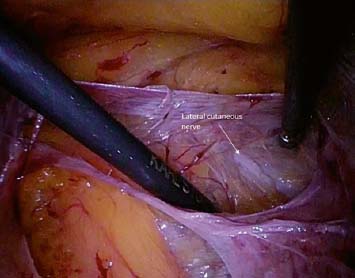
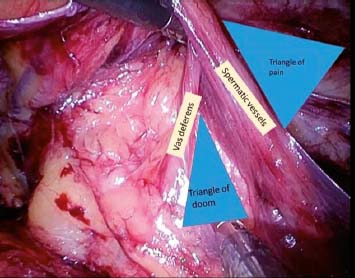
Fig. 12.7
Triangle of pain and triangle of doom
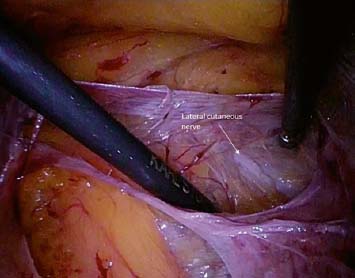
Fig. 12.8
Lateral cutaneous nerve at the space of Bogros
12.7.4 12.7.4 Hernia Sac Identification and Reduction
Once the medial and lateral dissection is completed (Fig. 12.9), we should be able to identify the entire hernia defect, followed by a proper hernia sac reduction and repair. This will allow the surgeon to visualize all the anatomical landmarks, to lessen the risk of injuries, to have a wider space for placing the prosthesis and, in case of inadvertent tear of the peritoneum, to continue to work safely without being affected by the pneumoperitoneum.
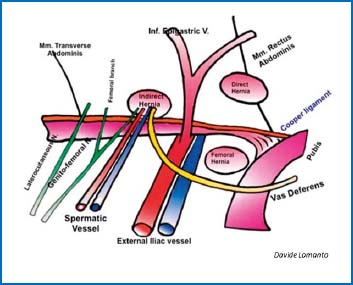
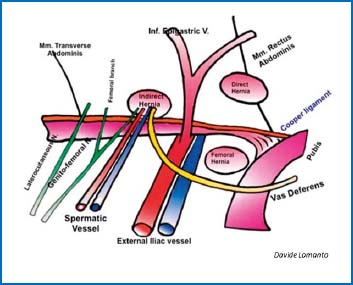
Fig. 12.9
Anatomic landmarks in endo-laparoscopic inguinal hernia repair
Exposure of the whole myopectineal orifice should be made after a complete medial and lateral dissection followed by the hernia sac reduction (Fig. 12.10).
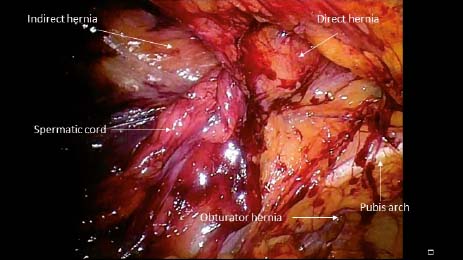
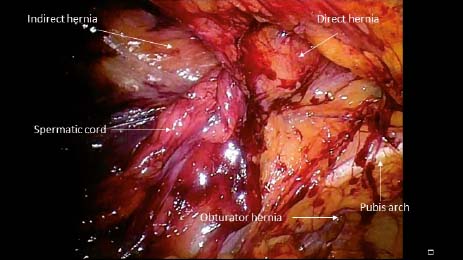
Fig. 12.10
Myopectineal orifice
12.7.5 12.7.5 Hernia Reduction
Medial or Direct Hernia In the endolaparoscopic approach, a defect medial to the inferior epigastric hernia and at the level of the Hesselbach’s triangle is a direct hernia. Reduction can be easily achieved by identifying and holding the hernia “pseudosac” and dividing it from the preperitoneal lipoma and peritoneum. Special care should be taken once the pubis arch is reached because of the risk of injury to the “corona mortis” and laterally to the iliac vessels and vas deferens. The “pseudosac” is grabbed and the hernia contents are then reduced.
Femoral Hernia Reduction of the hernia sac and content is achieved by gentle traction keeping in mind that the vessels hide behind the content (Fig. 12.11). If the content is not reducible by traction due to the small size of the defect, it may be necessary to widen the femoral defect by using a hook diathermy ONLY on the medial-upper side (Fig. 12.12). This will facilitate the hernia sac reduction.
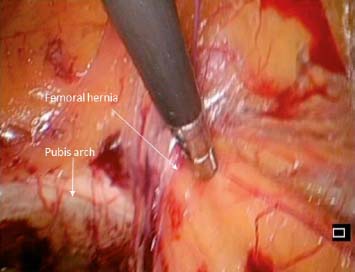
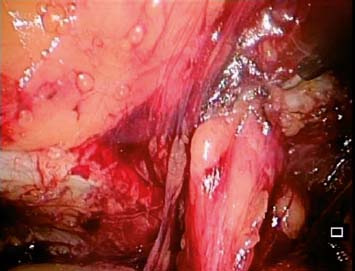
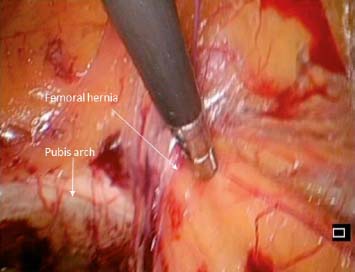
Fig. 12.11
Femoral hernia
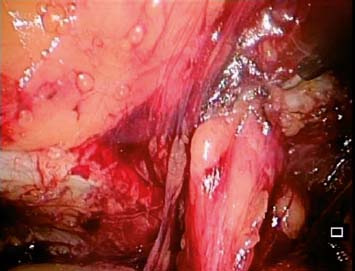
Fig. 12.12
Widening of the femoral ring at the medial-upper side
Obturator Hernia In the same canal where the obturator vessels are, it is possible that a preperitoneal fat and/or hernia sac is within. As in femoral hernia, a gentle traction will allow the reduction of the hernia sac (Fig. 12.13).
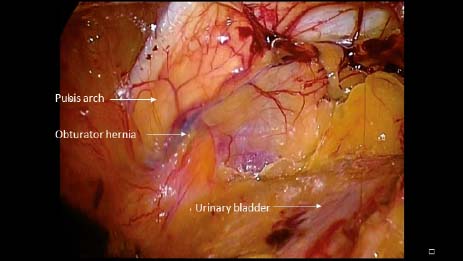
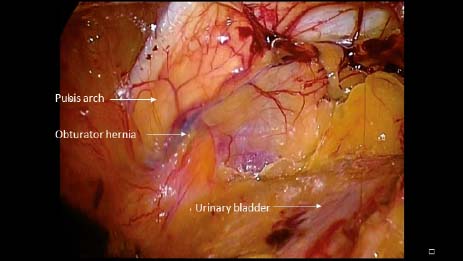
Fig. 12.13
Obturator hernia
Indirect Hernia Lateral to the IEV lies the deep ring and indirect hernia. The standard approach to indirect hernia repair requires the spermatic structures to be separated from the hernia sac. This can be achieved using the medial approach and four simple steps: 1. Separating the whole sac and spermatic cord from the iliac vessels; 2. Slimming the sac at the level of the deep ring with a partial reduction of both cord structures and sac; 3. Separating the cord structures from the sac on the inferior edge of the sac; 4. Reducing the sac by simple traction or transection. This can be necessary in cases of long or complete sac in order to minimize injury to the testis by overtraction. It is suggested to divide the sac using diathermy to reduce the risk of hematoma and to ligate the proximal part using pre-made suture loops. Lipoma of the cord should be fully reduced.

Full access? Get Clinical Tree






