Neurology
↓consciousness occurs in many diseases requiring admission to intensive care, and is often a cause for admission in its own right. Changes in neurological state may be related to intracranial pathology, or may occur in response to respiratory, circulatory, or metabolic disorders.
The immediate management of ↓consciousness should aim to protect the airway, ensure adequate respiration, prevent BP fluctuations, and maintain adequate oxygen delivery to the brain.
Causes
Physiological derangement
Hypoxia.
Hypercapnia.
Hypotension.
Hypothermia/hyperthermia.
Hypoglycaemia/hyperglycaemia.
Other metabolic derangement (e.g. hyponatraemia/hypernatraemia, hypocalcaemia, hypermagnesaemia, hyper-osmolar states).
Endocrine disease (e.g. hypothyroidism/hyperthyroidism, Addison’s disease).
Hepatic failure, renal failure.
Intracranial damage
Diffuse brain injury.
Extradural haemorrhage, subdural haemorrhage, intracerebral bleed.
Stroke/ischaemia.
Tumour/other intracerebral mass.
Cerebral oedema.
Seizures
Status epilepticus, post-ictal states.
Infections
Meningitis, encephalitis, intracranial abscess.
Systemic sepsis.
Drugs and toxins
Alcohol, sedatives, illicit drugs.
Presentation and assessment
Level of consciousness should be quantified using the Glasgow coma score (GCS) or AVPU systems (rather than poorly defined terms such as unconscious, semi-conscious, obtunded, comatose).
GCS assesses eye, verbal and motor responses and has a maximum score of 15 (fully conscious) and a minimum score of 3 (deeply unconscious/comatose). A GCS <8 equates to ‘unconsciousness’ (in the AVPU scale P is taken as the cut-off).
Glasgow coma score1
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Painful stimuli should not result in skin damage or marking, alternatives include supraorbital pressure, jaw thrust manoeuvre, nail bed pressure, and sternal rub.
Record each individual component of the GCS or why they might not be possible (e.g. patient intubated).
AVPU scale
An alternative to the GCS, which is particularly useful in children, in which there are 4 levels of alertness:
A—alert
V—responds to voice
P—responds to pain
U—unresponsive.
Transient loss of consciousness, or changes in consciousness are also important, particularly following head injuries.
Obtain a contemporaneous history if possible (e.g. from patient, relatives or ambulance crew):
Mechanism of injury (particularly in trauma cases, p.178)
p.178)
Any history of headaches, amnesia, limb weakness, seizures, vomiting, slurred speech
Any past or current medical history
Any medications (especially anticoagulants) or illicit drug use
Previous neurosurgery
Other indicators of altered neurological state may include:
Drowsiness, agitation, incoherence.
Incontinence.
Headache, amnesia.
Vomiting.
Seizures.
Evidence of meningism (painful neck flexion or straight-leg raising—often lost if GCS ≤5) may indicate meningitis or encephalitis.
Evidence of head or neck trauma, especially evidence of vault or base-of-skull fracture (see p.179).
p.179).
Focal neurological signs and symptoms including:
Loss or change in sensation (anaesthesia or paraesthesia) or power
Gait or balance problems
Problems speaking or understanding speech
Problems reading or writing
Abnormal peripheral or central reflexes (including lack of gag/cough reflex)
Abnormal plantar responses
Visual changes (e.g. blurred or double vision, or loss of visual field)
Eye examination may reveal:
Pupil signs: abnormal size, difference in size, reactivity, accommodation, deviation, or movements
Fundoscopy (if possible): haemorrhages, papilloedema
Raised ICP (>20 mmHg) where monitored.
Other signs and symptoms may include:
Airway: grunting, snoring, or complete obstruction may occur (airway obstruction may cause, or be caused by, loss of consciousness).
Respiratory:
Hypoventilation is a late sign unless associated with narcotic/drug overdose
Hyperventilation and/or Kussmaul’s breathing may indicate a metabolic acidosis (e.g. DKA)
Cheyne-Stokes is associated with brainstem events or raised ICP
Tachypnoea causing a respiratory alkalosis may sometimes occur
Neurogenic pulmonary oedema
Cardiovascular changes:
Tachycardia or hypotension may occur if there is associated trauma (especially spinal)
Bradycardia is often a late or pre-terminal sign
Hypertension may be associated with pain or agitation, or may be associated with severe neurological injury (more likely in patients who are deeply unconscious)
Cushing’s response of hypertension combined with bradycardia is a late sign indicative of severe intracranial hypertension
Renal: incontinence, polyuria.
Investigations
ABGs (for hypoxia, hypercapnia, acidaemia and anion gap).
FBC, coagulation screen (particularly in anticoagulated patients, or where acute liver failure is possible).
Serum glucose, with urinalysis for ketones if indicated (may identify hypo-, hyperglycaemia, or HHS/HONK).
Plasma osmolality (may help identify ethanol, methanol, or ethylene glycol poisoning).
Crossmatch blood (if there is trauma or risk of bleeding).
Blood alcohol levels and/or urine toxicology (for illicit drugs).
Blood, urine, and sputum cultures where infection is a possible cause.
ECG (tachyarrhythmia or bradyarrhythmia).
CXR (malignancy or pneumonia may be present).
CT head (and possible also neck, see Criteria for the request for CT scan of the head and also p.182).
Criteria for the request for CT scan of the head and also p.182).
MRI head (investigation of choice for suspected brainstem lesions).
In patients with associated trauma also consider: C-spine X-rays, other trauma X-rays (e.g. pelvis or long bones), skull or facial X-rays.
CFAM/EEG may be indicated if status epilepticus is suspected.
Criteria for the request for CT scan of the head
Immediate CT head scan for a head injury with any of the following:
GCS <13 on initial assessment in the emergency department.
GCS <15 at 2 hours after the injury on assessment in the emergency department.
Suspected open or depressed skull fracture.
Any sign of basal skull fracture (haemotympanum, ‘panda’ eyes, cerebrospinal fluid leakage from the ear or nose, Battle’s sign).
Post-traumatic seizure.
Focal neurological deficit.
>1 episode of vomiting.
Coagulopathy and any amnesia/loss of consciousness.
Other possible head trauma indications
Amnesia for events >30 minutes before a head injury.
Amnesia or loss of consciousness in the elderly or those with a coagulopathy (e.g. patients on warfarin).
Any injury with a suspicious mechanism (e.g. fall from height or ejection from a car).
Other indications
Any prolonged, unexplained episode of ↓consciousness or focal neurology.
History suggestive of subarachnoid haemorrhage, meningitis, encephalitis, or intracranial abscess.
Suspected stroke or other central neurological deficit.
Status epilepticus.
Raised ICP (if measured) resistant to treatment.
Immediate management
Give 100% O2, supporting airway/breathing/circulation as required.
Use cervical spine precautions if trauma is suspected/possible.
Obtain a contemporaneous history if possible (e.g. from relatives or ambulance crew):
An ‘AMPLE’ history should be obtained as a minimum ( p.2)
p.2)
Roughly assess neurological state (e.g. conscious and talking, or unconscious):
Simultaneously treat neurological complications which may interfere with ABC (e.g. seizures)
Airway
The airway may be compromised due to impaired conscious level:
Intubate the trachea as appropriate
If this is impossible (i.e. in a remote location) the patient may be placed in the recovery position (depending on the risk posed by other injuries)
If endotracheal intubation is required a rapid sequence intubation will be required to minimize the risk of aspiration.
The stress response to endotracheal intubation should be avoided if possible, by using induction agents/short-acting opiates.
Rapid sequence endotracheal intubation should be considered if:
GCS ≤8, or rapidly deteriorating
There is risk of aspiration of vomit or blood
There is a lack of gag reflex
There is facial or neck trauma putting the airway at risk
There is hypoxia (SaO2 <94%, PaO2 <9 kPa on air, <13 kPa on oxygen), hypercapnia (PaCO2 >6 kPa) or marked tachypnoea
Short-term deliberate hyperventilation is required
There is ongoing seizure activity
The patient is unlikely to remain still for investigations (e.g. CT)
The patient is agitated and combative but requiring treatment
Breathing
Ensure breathing/ventilation is adequate:
Circulation
Neurology
Formally assess neurological status, including:
Eye examination; including pupil size and reactivity and fundoscopy if possible
Evidence of trauma, especially evidence of vault or base-of-skull fracture
Plantar reflexes
Re-assess GCS after stabilizing airway, breathing, and circulation, and continue to re-assess consciousness and neurological state at regular intervals.
Other
Exclude and treat hypoglycaemia.
Exclude blockage of V-P shunt (if present).
Urgent CT scan may be required for diagnosis and appropriate management (prevent hypoxia, hypercapnia, hypotension, and hypertension throughout).
Raised ICP may be treated with hypertonic saline or mannitol until more definitive measures are employed (see p.186).
p.186).
Treat seizures as per protocol ( p.160).
p.160).
Check electrolytes.
Consider the possibility of unexpected overdose (see pp. 448 and 472); trials of naloxone or flumazenil may be appropriate.
pp. 448 and 472); trials of naloxone or flumazenil may be appropriate.
Further management
Worsening neurological state due to respiratory, cardiac, or metabolic disorders will often respond to successful management of the 1° precipitating disorder.
Neurosurgical referral
Where ↓level of consciousness is suspected, or proven, to be neurosurgically treatable then referral is indicated.
Indications for neurosurgical referral
Fractured skull with impaired consciousness, focal neurology, fits or other neurology.
Compound skull fractures, depressed skull fractures, or fracture to the base of skull.
Head injury with coma (GCS <9), deteriorating consciousness, neurological disturbance, which continue after resuscitation.
Head injury with confusion or neurological disturbance lasting >8 hours.
Evidence of intracranial haemorrhage (subarachnoid, subdural, extradural, or intracerebral) or mass lesion seen on CT.
Ventilation
Hypoxia should be avoided, as should hypo- or hypercapnia; an SaO2 >94%, PaO2 >13 kPa, and PaCO2 4.0-4.5 kPa should be maintained.
Pulmonary oedema may require the addition of PEEP (although caution may be required as high levels of PEEP may increase ICP).
Aspiration and chest infections are common in patients with ↓consciousness and should be actively sought/treated.
Head-up positioning may decrease the risk of aspiration and improve cerebral venous drainage.
Cardiovascular
Hypotension should be avoided; a MAP >90 mmHg should be sufficient initially:
Fluid resuscitation (avoiding hypotonic fluids) is often sufficient, although inotropes may be needed.
Sedation
Sedation will be required in most cases where patients are intubated and ventilated.
Sedatives with rapid offset (e.g. propofol) are useful initially as they can be discontinued and the level of consciousness rapidly reassessed.
Muscle relaxants may be required initially for endotracheal intubation, or for short periods during transfer or CT scanning; however, they run the risk of masking seizure activity:
Where neuromuscular blockade is used consider concurrent sedative infusions with anticonvulsive prophylaxis (e.g. propofol or midazolam), or CFAM/EEG monitoring.
Metabolic
Hyper- or hypoglycaemia should be avoided.
Hyper- or hyponatraemia should be corrected (see pp. 208 and 210).
pp. 208 and 210).
Pyrexia should be avoided; the place of mild/moderate hypothermia for severe neurological injuries is unclear, but is practised by some hospitals (mild/moderate hypothermia following cardiac arrest is indicated, see guidelines, p. 103).
p. 103).
Pitfalls/difficult situations
Hypoglycaemia is a common treatable cause; every patient with ↓consciousness should have a finger-prick blood sugar test.
Drug or alcohol use is frequently associated with other causes of diminished consciousness; a high suspicion of metabolic derangement or head injury/intracranial haemorrhage is essential in these patients.
Diminished consciousness is common in patients sedated in intensive care for prolonged periods, or where there has been renal or hepatic dysfunction leading to a prolonged washout period of sedative medications; a low threshold for suspecting metabolic derangement, intracranial haemorrhage/ischaemia is advisable.
Alcoholic and coagulopathic patients are at ↑ risk of intracranial haemorrhage even after relatively minor trauma.
Transfer to CT or MRI is hazardous (particularly MRI where monitoring and ventilators need to be ‘magnet compatible’); scans should only be attempted once patients are stable.
In some cases general surgical interventions (e.g. for major internal haemorrhage) may take precedence over investigating or treating neurological problems.
1Reprinted from The Lancet, 304, 7872, Teasdale and Jennett, ‘Assessment of coma and impaired consciousness: a practical scale’, pp. 81-84, Copyright 1974, with permission from Elsevier.
Further reading
Bateman DE. Neurological assessment of coma. J Neurol Neurosurg Psychiatry 2001; 71(SI): i13-i17.
Holzer M. Targeted temperature management for comatose survivors of cardiac arrest. N Engl J Med 2010; 363: 1256-64.
Mayer S, et al. Critical care management of increased intracranial pressure. J Intensive Care Med 2002; 17: 55-1767.
Moppett IK. Traumatic brain injury: assessment, resuscitation and early management. Br J Anaesth 2007; 99(1): 18-31.
NICE. Head injury. Triage, assessment, investigation and early management of head injury in infants, children and adults. London: NICE, 2007.
Sanap MN, et al. Neurologic complications of critical illness: Part I. Altered states of consciousness and metabolic encephalopathies. Crit Care Resusc 2002; 4(2): 119-32.
Scottish Intercollegiate Guidelines Network. Early management of patients with a head injury: a national clinical guideline. Edinburgh: Scottish Intercollegiate Guidelines Network, 2009.
Sydenham E, et al. Hypothermia for traumatic head injury (review). Cochrane Database Syst Rev 2009; 2: CD001048. DOI: 10.1002/14651858.CD001048.pub4
Varon J, et al. Therapeutic hypothermia: past, present, and future. Chest 2008; 133: 1267-74.
Seizures require intensive care management if they are prolonged, are associated with underlying disease, or cause severe physiological disturbance. Prolonged seizure activity carries a significant mortality. Any seizure lasting >5 minutes should be treated as an emergency.
A working definition of status epilepticus is: a seizure lasting >10 minutes, or repeated seizure activity without full consciousness between seizures, or failure to respond to 2 first-line treatments.
Causes
Hypoxia.
Brain injury (e.g. traumatic brain injury, intracranial tumour, haemorrhagic or ischaemic stroke, TTP).
Metabolic/electrolyte abnormalities (e.g. hypoglycaemia, hyperglycaemia, uraemia; sodium, calcium, or magnesium derangement).
Eclampsia ( p. 432).
p. 432).
Infection (e.g. meningitis, encephalitis, brain abscess).
Drug associated: drug withdrawal (especially alcohol), drug overdose, or illicit drug use (particularly cocaine).
In patients known to have epilepsy, seizures may be triggered by:
Head trauma, alcohol, intercurrent infection
Subtherapeutic blood levels of antiepileptic medications
Presentation and assessment
Seizures are most commonly generalized convulsive, with:
Loss of consciousness.
Tonic-clonic muscle movements (these may become very subtle when prolonged seizure activity leads to exhaustion).
Subtle eye movements (sometimes the only sign).
Teeth clenching, tongue biting, and/or urinary incontinence.
Physiological response to seizure:
Sweating and/or hyperthermia
Tachypnoea (airway obstruction may occur; hypoxia is associated airway obstruction and with prolonged fits)
Tachycardia and hypertension
Non-convulsive episodes are difficult to characterize, but may involve:
Impaired consciousness (defined as absence or complex seizures, and can range from lack of awareness to stupor).
Partial seizures: features may include focal twitching, facial tics, autonomic symptoms, and/or hallucinations (gustatory, acoustic, sensory, or visual), automatic behaviour (e.g. chewing, lip-smacking).
Investigations
ABGs (hypoxia, metabolic acidosis, raised lactate).
Serum glucose.
CK (raised after prolonged fits).
Urine/blood βHCG (to exclude pregnancy/eclampsia).
Blood and/or urine toxicology screen (for alcohol or illicit drugs).
Serum anticonvulsant drug levels (in patients with known epilepsy).
CXR (to exclude malignancy, infection, or aspiration).
Head CT/MRI (if seizures are prolonged, or have no obvious precipitant; or if focal neurology, papilloedema, or head injury are present).
Lumbar puncture (if infection is possible/likely).
Blood, urine, and sputum cultures (if infection is likely).
EEG as advised by neurologists.
Differential diagnoses
Any disease causing spasms (e.g. rigors, myoclonic jerks, dystonia).
Any disease causing syncope or agitation (see pp.152 and 192).
pp.152 and 192).
Immediate management
Give 100% O2, monitor SpO2.
Airway may be compromised due to seizure activity:
Maintain airway until fit is terminated, adjuncts may be required (consider nasal airways where there is marked jaw clenching)
Consider placing the patient in recovery position
Ensure breathing/ventilation is adequate (in some cases bag and mask support of ventilation may be needed).
Assess/monitor circulation and obtain IV access:
Fluid resuscitation may be needed to restore BP
Rapidly assess consciousness level and confirm presence of seizure.
Obtain a brief history.
Administer first-line antiseizure therapy: lorazepam IV 4 mg bolus:
Use diazepam IV (or rectally) 10 mg if lorazepam unavailable
Alternatively: midazolam 10 mg to buccal mucosa, or 200 mcg/kg intranasally (unlicensed alternative to lorazepam)
Within ICU a 2-4-mg bolus of midazolam may be used as first-line therapy if an infusion is already running
If there is no response after 5 minutes dose can be repeated (with monitoring of pulse oximetry and respiration).
Further seizure assessment and control:
Perform finger-prick blood sugar test, if hypoglycaemic, give 50 ml of 50% glucose IV or 500 ml 10% glucose (the need for hypoglycaemia correction outweighs the risk of exacerbating cerebral ischaemia).
If alcoholism, or malnourishment, is suspected give thiamine 250 mg (Pabrinex® 2 ampoules) IV over 10 minutes.
In women of child-bearing age perform a pregnancy test: if eclampsia is suspected follow protocol ( p.432, magnesium sulphate, loading dose: 20 mmol/4g IV over 3-5 minutes, followed by maintenance infusion of 5-10 mmol/hour).
p.432, magnesium sulphate, loading dose: 20 mmol/4g IV over 3-5 minutes, followed by maintenance infusion of 5-10 mmol/hour).
If seizure activity persists despite initial therapy commence second-line therapy: phenytoin (in 0.9% saline) 18 mg/kg IV infusion at a rate not exceeding 50 mg/minute; ECG monitoring is required:
If seizure activity persists 20 minutes from first presentation (or if the patient is severely hypoxic, acidotic or hypotensive at any time):
Induce general anaesthesia using thiopental or propofol, as a rapid sequence intubation with suxamethonium (or rocuronium if serum potassium is high).
Sedate with propofol or midazolam infusions (both may be required).
Avoid further muscle relaxant infusions unless absolutely necessary (may mask further seizures).
EEG monitoring must be used if muscle relaxant infusions are used (e.g. atracurium infusions).
If seizures persist discuss diagnosis and treatment with neurology:
Possible treatments include: levetiracetam (500-1000 mg IV), sodium valproate (800 mg IV over 3-5 minutes), lacosamide (50 mg IV BD over 15-60 minutes), or the addition of thiopental 1-5 mg/kg/hour IV or phenobarbital 5-12 mg/kg IV (maximum rate 100 mg/minute); follow-up doses of antiepileptics should be discussed with a neurologist
EEG/CFAM monitoring should be organized, aiming for a burst suppression pattern
Further management
Ensure that a full neurological assessment has been carried out and discuss the case with a neurologist.
Maintain PaCO2 4.5-5 kPa, PaO2 ≥10 kPa, temperature ≤37°C, Hb ≥10 g/dl, glucose 6-10 mmol/L, serum Na 135-140 mmol/L, where possible.
Where there is evidence of hypotension commence fluid resuscitation with inotropic support if required.
Pitfalls/difficult situations
If seizure control is achieved reassess airway as the sedative effects of treatment may require endotracheal intubation/ventilation.
Many drugs lower the fit threshold (e.g. flumazenil and antipsychotics).
Status epilepticus is not common in epileptics; always consider other causes of seizures such as infections.
Psychogenic seizures may be superficially similar to convulsive status epilepticus; the diagnosis is supported by the absence of hypoxia or acidosis, and if suspected a neurology opinion should be sought.
Where tumour or vasculitis are present consider dexamethasone.
Valproate may be preferred as second-line therapy for absence states.
1Phenytoin equivalents (P.E.) are used for fosphenytoin: fosphenytoin 1.5 mg = phenytoin 1 mg.
Further reading
Costello DJ, et al. Treatment of acute seizures and status epilepticus. J Intensive Care Med 2007; 22: 319-47.
Meierkord H, et al. EFNS guideline on the management of status epilepticus in adults. Eur J Neurol 2010; 17: 348-55.
Maganti R, et al. Nonconvulsive status epilepticus. Epilepsy Behav 2008; 12: 572-86.
NICE. The epilepsies: the diagnosis and management of the epilepsies in adults and children in primary and secondary care. London: NICE, 2012.
Rossetti AO, et al. Management of refractory status epilepticus in adults: still more questions than answers. Lancet Neurol 2011; 10: 922-30.
Scottish Intercollegiate Guidelines Network. Diagnosis and management of epilepsy in adults. A national clinical guideline. Edinburgh: SIGN, 2003.
A stroke (sometimes called a cerebrovascular accident, CVA, or occasionally a ‘brain attack’) is defined as an acute focal neurological deficit caused by cerebrovascular disease that lasts >24 hours or causes death. If the focal neurological deficit lasts <24 hours the diagnosis is a transient ischaemic attack (TIA).
Cerebral infarction is caused either by thromboembolic disorders (85%) or by haemorrhage (10% intracerebral haemorrhage, see  p.172; 5% subarachnoid haemorrhage,
p.172; 5% subarachnoid haemorrhage,  p.174; subarachnoid and intracerebral haemorrhages may also be caused by head injury, see
p.174; subarachnoid and intracerebral haemorrhages may also be caused by head injury, see  p.178).
p.178).
 p.172; 5% subarachnoid haemorrhage,
p.172; 5% subarachnoid haemorrhage,  p.174; subarachnoid and intracerebral haemorrhages may also be caused by head injury, see
p.174; subarachnoid and intracerebral haemorrhages may also be caused by head injury, see  p.178).
p.178).Causes
The incidence of stroke increases with age. Causes include: Emboli:
Platelet aggregates from ruptured atherosclerotic plaques.
Left atrial or ventricular thrombus 2° to atrial fibrillation, poor ventricular function, or myocardial infarction.
Paradoxical emboli (venous emboli entering the arterial circulation via patent foramen ovale, ASD, or VSD).
Prosthetic heart valves; indwelling lines/prosthesis.
Infective endocarditis.
Following carotid or cardiac surgery.
Thrombosis:
Rupture of atherosclerotic lesions (risk factors for atherosclerosis include age, male sex, family history, smoking, diabetes, hypertension, and hyperlipidaemia).
Vasculitis.
Cerebral venous thrombosis (caused by hypercoagulable states like dehydration, polycythaemia, thrombocythaemia, OCP medication, protein S/C deficiency, factor V Leiden deficiency).
Other:
Vertebral or carotid dissection (spontaneous or post traumatic).
Vessel occlusion by tumour/abscess.
Carotid occlusion (post strangulation).
Systemic hypotension (e.g. post cardiac arrest).
Patients who have had TIAs are at high risk of stroke, especially if:
They have had 2 or more TIAs within 1 week.
They have an ‘ABCD’ (Age, Blood pressure, Clinical features, Duration) score of ≥4.
Presentation and assessment
Strokes are atraumatic, but may result in associated trauma (e.g. by causing falls). They result in rapid focal or global neurological deterioration. Other signs and symptoms may include
Airway: grunting, snoring or complete obstruction.
Respiratory: Cheyne-Stokes breathing, tachypnoea, bradypnoea (hypoventilation is a late sign):
Neurogenic pulmonary oedema may sometimes occur
Cardiovascular changes: tachycardia and/or hypertension (hypertension associated with bradycardia is a late or pre-terminal sign):
Renal: incontinence.
Neurological: agitation, diminished consciousness:
Common presentations: a commonly used system combining anatomical and clinical systems for classifying strokes is the Oxford acute stroke classification system ( p.169)
p.169)
Atypical presentations: seizures, falls, or personality change
Thrombotic stroke often presents with evolving neurology, whilst embolic stroke presents with sudden onset, rapidly developing neurology
Investigations
ABGs (in case of hypoxia or metabolic acidosis).
FBC.
Coagulation screen (in case of coagulopathy).
Serum glucose (hypo/hyperglycaemia).
Serum lipids.
Head CT scan (to clarify diagnosis, extent of cerebral damage, differentiate infarct from haemorrhage and exclude hydrocephalus).
Carotid Doppler studies (to identify carotid stenosis of >70%).
ECHO (the source of any emboli may be cardiac).
Other investigation that may be of benefit include:
Thrombophilia screen
Auto-antibody screen
Plasma electrophoresis
Blood cultures
Syphilis screen
Differential diagnoses
Migraine.
Hypoglycaemia.
Partial epileptic seizures, or following seizures (post-ictal states).
Space-occupying lesions (e.g. tumour, abscess or subdural haematoma).
Demyelinating disease.
Cerebral venous thrombosis.
Immediate management
Airway may be compromised due to impaired conscious level, place patient in recovery position or intubate trachea as appropriate.
Few stroke patients benefit from invasive ventilatory support but some might if gag reflex is absent, the GCS is <8, and the diagnosis is unclear before further investigation is undertaken (or there is evidence of other illness, e.g. pneumonia)
Ensure breathing/ventilation is adequate.
Assess circulation and obtain IV access; commence fluid resuscitation where hypotension is present.
Hypertension is common and should not be corrected unless:
Thrombolysis is required and BP is ≥185/110 mmHg
Hypertensive encephalopathy, nephropathy, or cardiac failure/MI are suspected
Aortic dissection is present
Pre-eclampsia/eclampsia is present
Assess and monitor consciousness level.
Perform a rapid, detailed neurological assessment (with fundoscopy).
An urgent CT is required if:
There are indications for thrombolysis or early anticoagulation
There is evidence of trauma
The patient is anticoagulated or has a known bleeding tendency
There is rapidly progressive, inconsistent, poorly localized, or fluctuating neurology; or brainstem symptoms
The patient has a ↓level of consciousness (GCS <13)
Papilloedema, fever, or meningism are present
The patient had a severe headache at onset of neurology
Aspirin 300 mg (oral, or if dysphagic rectally or via NGT) should be given once a diagnosis of haemorrhage has been excluded (unless thrombolysis is used, then it should be withheld for 24 hours):
Aspirin should also be given to patients with >1 TIA in a week, or an ‘ABCD’ score ≥4
Thrombolysis with t-PA of ischaemic strokes must be considered.
Neurosurgical intervention may be needed in patients with hydrocephalus or a large infarcted area of the middle cerebral artery (MCA) territory causing oedema (a ‘malignant’ stroke):
Decompressive craniectomy for ‘malignant’ stroke is indicated in patients aged ≤60 years with: clinical deficits suggestive of infarction in the territory of the MCA with a National Institutes of Health Stroke Scale (NIHSS) score above 15; a decrease in the level of consciousness to give a score of 1 or more on item 1a of the NIHSS; signs on CT scan of an infarct of at least 50% of MCA territory, with or without additional infarction in the territory of the anterior or posterior cerebral artery on the same side, or infarct volume greater than 145 cm3 as shown on diffusion-weighted MRI
Further management
If not already performed, brain imaging should be undertaken within 24 hours where possible.
Ensure adequate hydration and nutrition (often NG feeding is required until a swallowing assessment can be performed).
Aspirin (50-300 mg) should be continued until an alternative antiplatelet therapy is started.
Prior statin therapy should be continued.
Anticoagulation is controversial; heart lesions are the only definite indication for full anticoagulation.
Lowering BP may extend the infarct; it is unclear at what point a high BP requires may benefit from treatment:
Consider using short-acting agents to reduce BP slowly if ≥220/110 mmHg
Ensure adequate analgesia and DVT prophylaxis.
Maintain blood glucose 4-10 mmol/L.
Investigate and treat fever aggressively (aspiration is a common cause of infection).
Aggressive physiotherapy and transfer to a specialist stroke unit are associated with better outcomes.
Consider initiating treatment aimed at modifying cardiovascular risk factors.
Pitfalls/difficult situations
Strokes in young patients should always raise the suspicion of ‘atypical’ causes (e.g. procoagulant disorders such as vasculitis).
Up to 5% of patients presenting with stroke have underlying space-occupying lesions (e.g. tumour, abscess, or subdural haematoma)
Where there is any history of scalp tenderness always consider temporal arteritis and measure ESR.
Careful BP monitoring is important following carotid endarterectomy as strokes are associated with hyper-/hypotension.
Haemorrhagic transformation of ischaemic strokes may occur (with or without thrombolysis).
Strokes after cardiac surgery or cardiac bypass present diagnostic and therapeutic challenges, especially as these patients are often extensively anticoagulated.
Cerebral oedema caused by a ‘malignant’ MCA territory infarct commonly occurs on day 2-5.
The Oxford acute stroke classification system1
Hemiparesis with/without hemisensory loss.
Homonymous hemianopia and higher cerebral dysfunction (e.g. dysphasia, visuospatial dysfunction neglect).
Any two TACS features (see earlier list).
Higher cerebral dysfunction.
Isolated motor and/or sensory deficit in one limb or in the face.
Pure motor or sensory stroke (involving two of face, arm, or leg).
Ataxic hemiparesis.
Dysarthria or ‘clumsy hand’ syndrome.
Bilateral motor sensory and sensory signs.
Cerebellar signs, unless accompanied by ipsilateral motor deficit.
Disorder of conjugate eye movement.
Ipsilateral cranial nerve palsy with contralateral motor and/or sensory deficit.
Isolated homonymous visual field deficit.
Thrombolysis with alteplase1
Consider giving alteplase for treatment of acute ischaemic stroke if indicated by exclusion of intracranial haemorrhage. Alteplase must be used in full accordance with its marketing authorization, which states:
Use within 3 hours of symptom onset.
Treatment must be by a physician specialized in neurological care.
Alteplase should be administered only within in a stroke service with:
Staff trained in delivering thrombolysis and in monitoring for any associated complications, including level 1 and level 2 nursing care staff trained in acute stroke and thrombolysis.
Immediate access to imaging and re-imaging, and staff trained to interpret the images.
Staff in A&E who are trained and supported can administer thrombolysis (in accordance with its marketing authorization) if patients are managed within a specialist acute stroke service.
Consider BP reduction to 185/110 mmHg or lower in people who are candidates for thrombolysis.
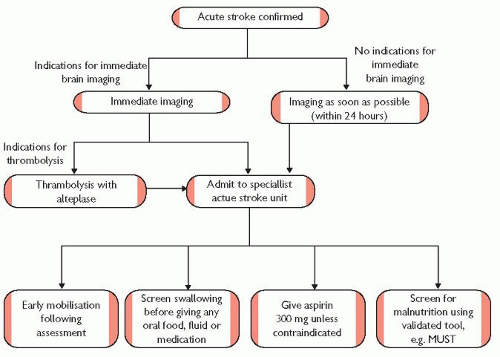 Fig. 5.2 Emergency management of patients with acute stroke. Adapted from NICE. Stroke: diagnosis and initial management of acute stroke and transient ischaemic attack (TIA). London: NICE, 2008. |
1Reprinted from The Lancet, 337, 8756, J. Bamford et al., ‘Classification and natural history of clinically identifiable subtypes of cerebral infarction’, pp. 1521-1526.
2The final letter may be changed to denote the type of stroke: S for syndrome, I for infarct, H for haemorrhage (i.e. TACS, TACI, or TACH).
Further reading
AHA. Adult stroke. Circulation 2005; 112: 111-20.
Lukovits TG, et al. Critical care of patients with acute ischemic and hemorrhagic stroke: update on recent evidence and international guidelines. Chest 2011; 139: 694-700.
NICE. Stroke: diagnosis and initial management of acute stroke and transient ischaemic attack (TIA). London: NICE, 2008.
Sandset EC, et al. The angiotensin-receptor blocker candesartan for treatment of acute stroke (SCAST): a randomised, placebo-controlled, double-blind trial. Lancet 2011; 377: 741-50.
SIGN. Management of patients with stroke or TIA: assessment, investigation, immediate management and secondary prevention: a national clinical guideline. Edinburgh: SIGN, 2008.
Wardlow JM, et al. Thrombolysis for acute ischaemic stroke (review). Cochrane Database Syst Rev 2009; 4: CD000213. DOI: 10.1002/14651858.CD000213.pub2.
Vahedi K, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol 2007; 6: 215-22.
van der Worp B, et al. Acute ischaemic stroke. N Engl J Med 2007; 357: 572-9.
Spontaneous intracerebral haemorrhage (SICH) is bleeding into the parenchyma of the brain (possibly extending to the subarachnoid space). Intracerebral haemorrhage may be supratentorial or infratentorial. The associated mortality is higher than that of either thromboembolic stroke or subarachnoid haemorrhage (30-day mortality ranges from 35-52%.).
Causes
Chronic hypertension (commonest overall cause)
Amyloid angiopathy
2° intracerebral haemorrhage:
Acute hypertension
Eclampsia/pre-eclampsia ( p.432)
p.432)
Drugs: sympathomimetics and recreational drugs such as cocaine
Coagulopathies, especially following thrombolysis and warfarin use
Aneurysms and arteriovenous malformations
Tumours; following neurosurgery
Complicating CNS infections or venous sinus thrombosis
Haemorrhagic transformation of thromboembolic stroke.
Presentation and assessment
The presentation of intracerebral haemorrhage overlaps with that of ischaemic/thromboembolic stroke ( p.166):
p.166):
 p.166):
p.166):
Supratentorial haemorrhages cause sensory/motor deficits, aphasia, neglect, gaze deviation, and hemianopia.
Infratentorial haemorrhages cause brainstem dysfunction, cranial nerve defects, ataxia, and nystagmus.
The following are also common:
Headache, nausea, and vomiting
Elevated BP (up to 90% of patients)
Seizures (up to 10% of patients)
 p.574
p.574 p.86
p.86 p.153
p.153 p.186
p.186
 p.155
p.155 p.186
p.186 p.86
p.86 p.66
p.66 p.204
p.204 p.268
p.268 p.306
p.306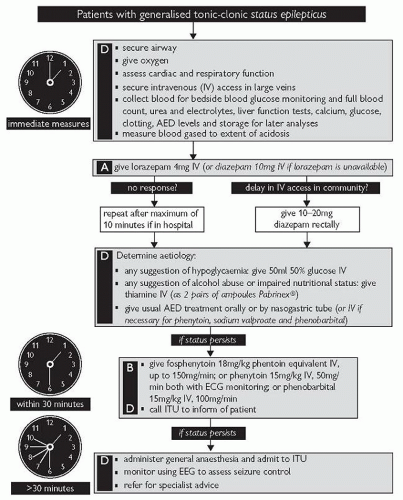
 p.174
p.174
 p.186
p.186 p.167
p.167


