![]() Emergency venous access for fluid resuscitation and drug infusion
Emergency venous access for fluid resuscitation and drug infusion
![]() Infusions requiring central venous administration (vasopressors, hyperosmolar solutions, hyperalimentation)
Infusions requiring central venous administration (vasopressors, hyperosmolar solutions, hyperalimentation)
![]() Central venous pressure and oxygen monitoring
Central venous pressure and oxygen monitoring
![]() Routine venous access due to inadequate peripheral IV sites
Routine venous access due to inadequate peripheral IV sites
![]() Introduction of pulmonary artery catheter
Introduction of pulmonary artery catheter
![]() Introduction of transvenous pacing wire
Introduction of transvenous pacing wire
CONTRAINDICATIONS
![]() No absolute contraindications
No absolute contraindications
![]() Relative Contraindications
Relative Contraindications
![]() Coagulopathic patients (femoral approach preferred)
Coagulopathic patients (femoral approach preferred)
![]() Combative or uncooperative patients
Combative or uncooperative patients
![]() Overlying infection, burn, or skin damage at puncture site
Overlying infection, burn, or skin damage at puncture site
![]() Trauma at the cannulation site
Trauma at the cannulation site
![]() Penetrating trauma with suspected proximal vascular injury
Penetrating trauma with suspected proximal vascular injury
![]() Suspected cervical spine fracture
Suspected cervical spine fracture
RISKS/CONSENT ISSUES
![]() Pain (local anesthesia will be given)
Pain (local anesthesia will be given)
![]() Local bleeding and hematoma
Local bleeding and hematoma
![]() Infection (sterile technique will be utilized)
Infection (sterile technique will be utilized)
![]() Pneumothorax or hemothorax and the need for thoracostomy tube
Pneumothorax or hemothorax and the need for thoracostomy tube
![]() General Basic Steps
General Basic Steps
![]() Preprocedure ultrasound (if using ultrasound guidance)
Preprocedure ultrasound (if using ultrasound guidance)
![]() Vessel localization
Vessel localization
![]() Analgesia
Analgesia
![]() Insertion
Insertion
![]() Seldinger technique
Seldinger technique
![]() Dilation
Dilation
![]() Catheter insertion
Catheter insertion
![]() Confirmation
Confirmation
![]() Flush and secure
Flush and secure
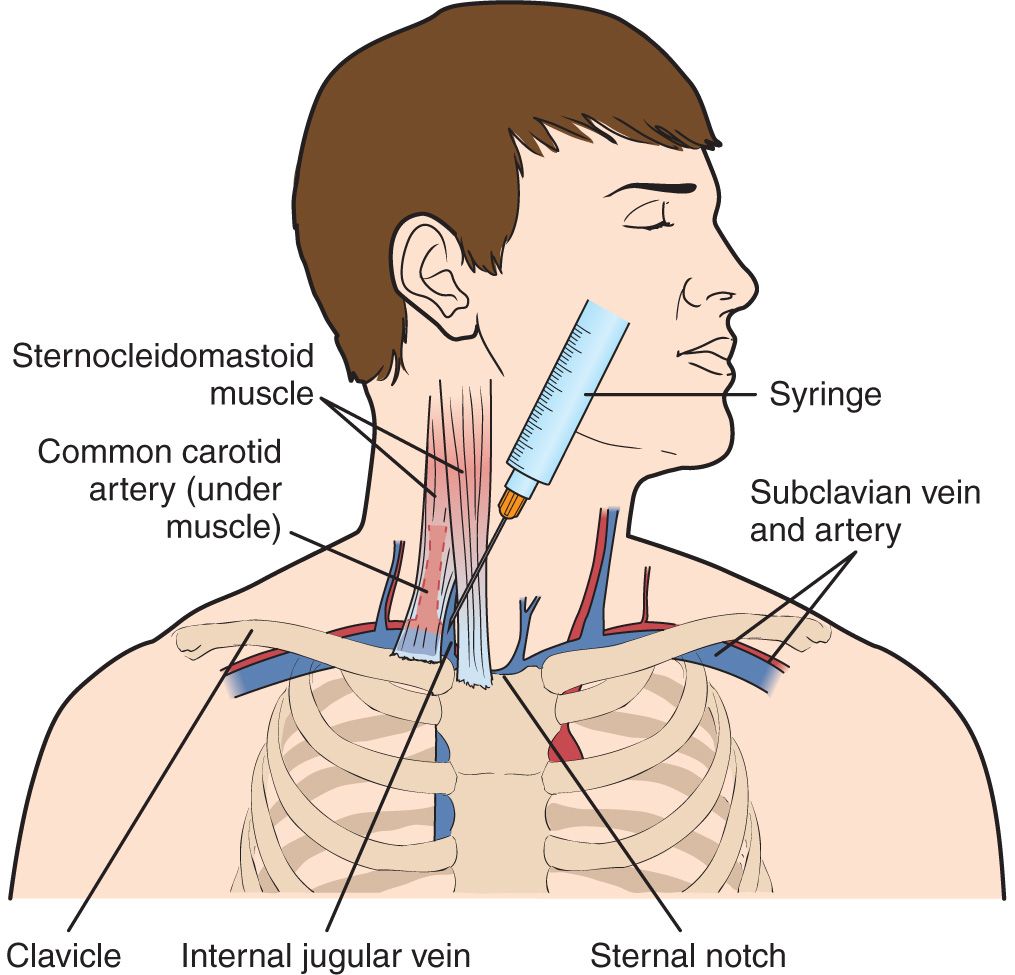
LANDMARK TECHNIQUE
Site of insertion is the apex of the triangle formed by the sternal and clavicular heads of the sternocleidomastoid muscle and the clavicle. This point is lateral to the carotid pulse. The needle is pointed toward the ipsilateral nipple (FIGURE 23.1).
ULTRASOUND-GUIDED TECHNIQUE
Real-time ultrasound-guided internal jugular vein (IJV) catheterization has been shown to:
![]() Increase success rates
Increase success rates
![]() Decrease the number of attempts
Decrease the number of attempts
![]() Decrease skin to blood flash time
Decrease skin to blood flash time
![]() Decrease complications
Decrease complications
![]() Help achieve successful cannulation when landmark attempts have failed
Help achieve successful cannulation when landmark attempts have failed
The use of ultrasound to guide the procedure also allows detection of anatomical variants:
![]() Carotid artery (CA) directly below the IJV instead of lateral
Carotid artery (CA) directly below the IJV instead of lateral
![]() Small IJV diameter
Small IJV diameter
![]() Noncompressible IJV, indicating the presence of thrombus
Noncompressible IJV, indicating the presence of thrombus
If ultrasound is available for use, placement of the IJV catheter using ultrasound guidance is highly recommended.
SUPPLIES
![]() Central Venous Catheter (CVC) Kit
Central Venous Catheter (CVC) Kit
![]() Drapes, chlorhexidine prep (2), gauze
Drapes, chlorhexidine prep (2), gauze
![]() Catheter (multiport, cordis, or hemodialysis)
Catheter (multiport, cordis, or hemodialysis)
![]() Guidewire within plastic sheath
Guidewire within plastic sheath
![]() Lidocaine, anesthesia syringe, and a small-gauge needle
Lidocaine, anesthesia syringe, and a small-gauge needle
![]() Three-inch introducer needle and syringe
Three-inch introducer needle and syringe
![]() Dilator
Dilator
![]() Scalpel
Scalpel
![]() Suture
Suture
![]() Sterile gloves, sterile gown, sterile cap, eye protection, and mask
Sterile gloves, sterile gown, sterile cap, eye protection, and mask
![]() Sterile drapes
Sterile drapes
![]() Sterile saline flushes
Sterile saline flushes
![]() Sterile port caps
Sterile port caps
![]() Ultrasound machine (optional)
Ultrasound machine (optional)
![]() Sterile ultrasound probe cover with sterile ultrasound gel (optional)
Sterile ultrasound probe cover with sterile ultrasound gel (optional)
TECHNIQUE
![]() Patient Preparation
Patient Preparation
![]() Cardiac monitoring to detect dysrhythmias triggered by the wire being advanced into the right ventricle
Cardiac monitoring to detect dysrhythmias triggered by the wire being advanced into the right ventricle
![]() Supplemental oxygen and continuous pulse oximetry monitoring
Supplemental oxygen and continuous pulse oximetry monitoring
![]() Rotate the patient’s head 30 to 45 degrees away from the side of cannulation
Rotate the patient’s head 30 to 45 degrees away from the side of cannulation
![]() Lower the head of the bed to 15 to 30 degrees in Trendelenburg position
Lower the head of the bed to 15 to 30 degrees in Trendelenburg position
![]() If using ultrasound guidance, evaluate the right and left IJVs for ideal size and position
If using ultrasound guidance, evaluate the right and left IJVs for ideal size and position
![]() Sterilize the neck and clavicle area with chlorhexidine or povidone–iodine solution
Sterilize the neck and clavicle area with chlorhexidine or povidone–iodine solution
![]() Wear surgical cap, eye protection, mask, sterile gown and gloves
Wear surgical cap, eye protection, mask, sterile gown and gloves
![]() Drape with sterile sheets to cover the patient’s head and legs
Drape with sterile sheets to cover the patient’s head and legs
![]() If using ultrasound guidance, have an assistant place the probe (with gel applied) inside the sterile probe sheath
If using ultrasound guidance, have an assistant place the probe (with gel applied) inside the sterile probe sheath
Note: Unless immediate emergent access is warranted, the physicians attempting the procedure must wear cap, eye shields, and mask, along with sterile gown and gloves.
![]() Vessel Localization
Vessel Localization
![]() If attempting localization of right IJV, use the right hand to hold the syringe and introducer needle. With the left hand, palpate the CA to avoid arterial puncture while guiding needle insertion. If attempting the left IJV, reverse hands.
If attempting localization of right IJV, use the right hand to hold the syringe and introducer needle. With the left hand, palpate the CA to avoid arterial puncture while guiding needle insertion. If attempting the left IJV, reverse hands.
![]() Analgesia
Analgesia
![]() Use a small-gauge needle to anesthetize skin and subcutaneous tissue with 1% lidocaine
Use a small-gauge needle to anesthetize skin and subcutaneous tissue with 1% lidocaine
![]() Insertion
Insertion
![]() Using the above landmarks, insert the introducer needle at 30- to 60-degree angle to the skin just lateral to the apex of the triangle just lateral to the carotid pulse (Figure 23.1)
Using the above landmarks, insert the introducer needle at 30- to 60-degree angle to the skin just lateral to the apex of the triangle just lateral to the carotid pulse (Figure 23.1)
![]() Apply negative pressure to the syringe plunger while advancing the needle 3 to 5 cm or until a flash of blood is seen in the syringe
Apply negative pressure to the syringe plunger while advancing the needle 3 to 5 cm or until a flash of blood is seen in the syringe
![]() If no flash is obtained, withdraw the needle slowly while continuing to aspirate
If no flash is obtained, withdraw the needle slowly while continuing to aspirate
![]() If redirecting the needle, always withdraw the needle to the level of skin before advancing again
If redirecting the needle, always withdraw the needle to the level of skin before advancing again
![]() Once the needle enters the vessel, blood will flow freely into the syringe
Once the needle enters the vessel, blood will flow freely into the syringe
![]() Stabilize and hold the introducer needle with the nondominant hand
Stabilize and hold the introducer needle with the nondominant hand
![]() Remove the syringe and ensure that venous blood continues to flow easily
Remove the syringe and ensure that venous blood continues to flow easily
![]() Use a finger to occlude the needle hub to prevent air embolism
Use a finger to occlude the needle hub to prevent air embolism
![]() Seldinger Technique
Seldinger Technique
![]() Advance the guidewire through the introducer needle. The wire should pass easily. Do not force the guidewire.
Advance the guidewire through the introducer needle. The wire should pass easily. Do not force the guidewire.
![]() If resistance is met, withdraw the wire and rotate it, adjust the angle of needle entry, or remove the wire and reaspirate with the syringe to ensure the needle is still in the vessel.
If resistance is met, withdraw the wire and rotate it, adjust the angle of needle entry, or remove the wire and reaspirate with the syringe to ensure the needle is still in the vessel.
![]() When at least half of the guidewire is advanced through the needle, remove the needle over the wire. Keep one hand holding the wire at all times. Never let go of the guidewire.
When at least half of the guidewire is advanced through the needle, remove the needle over the wire. Keep one hand holding the wire at all times. Never let go of the guidewire.
![]() Make a superficial skin incision with the bevel of the scalpel blade angled away from wire
Make a superficial skin incision with the bevel of the scalpel blade angled away from wire
![]() Ensure the incision is large enough to allow easy passage of the dilator
Ensure the incision is large enough to allow easy passage of the dilator
![]() Dilation
Dilation
![]() Thread the dilator over the guidewire, always holding onto the wire
Thread the dilator over the guidewire, always holding onto the wire
![]() While holding the guidewire with the nondominant hand, advance the dilator through the skin into the vessel with a firm, twisting motion
While holding the guidewire with the nondominant hand, advance the dilator through the skin into the vessel with a firm, twisting motion
![]() Remove the dilator, leaving the guidewire in place
Remove the dilator, leaving the guidewire in place
![]() Catheter Insertion
Catheter Insertion
![]() Thread the catheter over the wire and retract the wire until it emerges from the catheter’s port
Thread the catheter over the wire and retract the wire until it emerges from the catheter’s port
![]() While holding the guidewire, advance the catheter through the skin into the vessel to the desired depth. Optimal depth depends on patient size and is typically 12 to 18 cm for the right IJV and 15 to 20 cm for the left IJV.
While holding the guidewire, advance the catheter through the skin into the vessel to the desired depth. Optimal depth depends on patient size and is typically 12 to 18 cm for the right IJV and 15 to 20 cm for the left IJV.
![]() Withdraw the guidewire through the catheter
Withdraw the guidewire through the catheter
![]() Use a syringe to aspirate blood from the catheter to confirm placement in the vein
Use a syringe to aspirate blood from the catheter to confirm placement in the vein
![]() Confirmation
Confirmation
![]() Manometry
Manometry
![]() Blood gas analysis
Blood gas analysis
![]() Sonographic confirmation of the catheter in the vein
Sonographic confirmation of the catheter in the vein
![]() Post procedure chest x-ray (CXR)
Post procedure chest x-ray (CXR)
![]() Confirm the catheter tip in the superior vena cava just proximal to the right atrium
Confirm the catheter tip in the superior vena cava just proximal to the right atrium
![]() Rule out pneumothorax
Rule out pneumothorax
![]() Flush and Secure
Flush and Secure
![]() Aspirate, flush, and heplock each central line lumen
Aspirate, flush, and heplock each central line lumen
![]() Suture the catheter to the skin using silk or nylon sutures
Suture the catheter to the skin using silk or nylon sutures
![]() Cover the skin insertion site with a sterile dressing (bacteriostatic if available)
Cover the skin insertion site with a sterile dressing (bacteriostatic if available)
![]() Ultrasound-guided Technique
Ultrasound-guided Technique
![]() Use a high-frequency linear probe (5–10 MHz)
Use a high-frequency linear probe (5–10 MHz)
![]() Probe marker on the ultrasound probe should point toward the operator’s left so that it corresponds with the marker on left side of the ultrasound screen (FIGURE 23.2)
Probe marker on the ultrasound probe should point toward the operator’s left so that it corresponds with the marker on left side of the ultrasound screen (FIGURE 23.2)
![]() Identify the IJV and CA (FIGURE 23.3)
Identify the IJV and CA (FIGURE 23.3)

FIGURE 23.2 Correct positioning of the ultrasound machine in line with the operator’s sight and procedure site with the probe marker facing the operator’s left. (Image courtesy of Mount Sinai Emergency Medicine site, http://sinaiem.us/tutorials/peripheral-iv-access)

Full access? Get Clinical Tree