CHAPTER 11 Cervical plexus block
Clinical anatomy
The branches of the superficial cervical plexus supply the skin and superficial structures of the head, neck, and shoulder. There are four cutaneous branches, which become subcutaneous at the posterior border of the sternocleidomastoid muscle (Fig. 11.1). The lesser occipital and great auricular are derived from the C2 and C3 roots and run in a cephalad direction. The lesser occipital nerve supplies sensation to the upper side of the neck, the upper part of the auricle, and the adjoining skin of the scalp. The great auricular nerve is the largest cutaneous branch and divides into an anterior and a posterior branch. The posterior branch supplies the skin lying behind the ear and the medial and lateral surfaces of the lower part of the auricle. The anterior branch supplies the skin in the lower posterior part of the face and the concave surface of the auricle. The transverse cervical nerve, also from C2 and C3 roots, runs horizontally across the neck and provides sensory innervation to the anterolateral aspect of the neck from the mandible to the sternum. The supraclavicular branch, from the C3 and C4 roots, runs caudally over the clavicle and divides into three branches: medial, intermediate, and lateral. It provides sensory innervation to the lower aspect of the neck, acromial region of the neck, and as far as the second intercostal space on the chest.
Surface anatomy
The main landmarks for the superficial cervical plexus block (Fig. 11.2) include the mastoid process, suprasternal notch, and posterior border of the sternocleidomastoid muscle at the level of the cricoid cartilage. The sternocleidomastoid muscle and its posterior border can be accentuated by asking the patient to perform a head lift. The external jugular vein crosses the posterior border of the sternocleidomastoid muscle close to the injection site. It can be accentuated by asking the patient to perform a Valsalva maneuver. The carotid artery can be palpated medial to the sternocleidomastoid muscle and indicates the vascular nature of the territory.
The main landmarks for the deep cervical plexus block (Fig. 11.3) include the mastoid process; the posterior border of the sternocleidomastoid muscle at the level of the cricoid cartilage; C6 transverse process (the most prominent cervical transverse process); and the thyroid cartilage.
Sonoanatomy
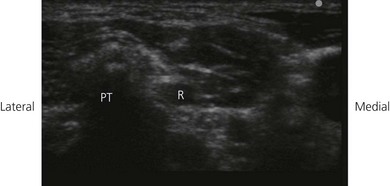
The cervical plexus is found at the level of the first four cervical vertebrae deep to the sternocleidomastoid, in the layer superficial to the scalenus medius and levator scapulae. The cervical plexus can be further divided into a superficial and deep portion. The superficial branches perforate the cervical fascia to supply skin and other integumental structures whilst the deep branches predominantly supply muscle. The patient is positioned supine with the head slightly turned to the opposite side. Perform a systematic survey from superficial to deep, medial to lateral and cranially. A high frequency ultrasound transducer is placed in a coronal plane anterolateral to the neck to identify the respective vertebral level The transverse process of C7 usually does not have an anterior tubercle, but only one prominent posterior tubercle (Fig 11.4). Additionally, the C6 transverse process is sonographically verified by tracing the course of the vertebral artery, which usually enters the foramen at that vertebra. After achieving a coronal echoplane with the depiction of the transverse processes of C6 and C7, the transducer is shifted cranially and the fourth cervical vertebra (C4) is identified by counting the respective vertebral levels upwards. Parts of the superficial plexus can be identified in the double fascial layer in all patients at the level of C4. This double fascial layer is formed by the fascia of the sternocleidomastoid muscle and the deep cervical fascia (Fig. 11.5). Here the C4 nerve root can also be seen arising between the anterior and posterior tubercles of the fourth transverse process (Fig. 11.5). This level correlates with the carotid bifurcation in most patients (Fig. 11.5).
< div class='tao-gold-member'>

Full access? Get Clinical Tree