Fig. 5.1
The device with its central core and preperitoneal layer
Because of its geometrical structure, this device transforms expulsion forces into gripping forces, a key point of this sutureless repair. These forces lead to a better quality in tissue ingrowth, compared to other static meshes that are usually incorporated in a scar plate. This prolonged, low-load, cyclical stress to the abdominal wall seems to be the main cause of the obliteration of the defect and incorporation of the device with good quality tissue [6]. This entails less mesh shrinkage, as a result of the fact that the tissue covers the Freedom inguinal hernia device gradually, in a more physiological manner, unlike the case with commonly used polypropylene meshes that induce an acute fibrotic response. This may lead to a reduction in recurrence rate and patient discomfort [7].
5.3 5.3 Patient Selection
Almost every patient eligible for elective surgery for primary inguinal hernia could be selected for this kind of repair. Patients can be males or females, they should have a clinically relevant primary inguinal hernia with a defect size at operation between 20 and 35 mm in diameter, which corresponds to a M2/L2 in the European Hernia Society (EHS) groin hernia classification [8], and they should be diagnosed with direct or indirect defect.
Contraindications for this repair are: previous surgery on the hernia operative site, giant inguinoscrotal hernia, recurrent inguinal hernia, known collagen disorder, femoral hernia, body mass index >35, and cases in which peritoneum cannot be closed.
5.4 5.4 Surgical Technique
This procedure can be performed under local anesthesia and the patient can be discharged the same day of the operation.
After a horizontal skin incision of 3–6 cm, perform a dissection through the Scarpa’s fascia to external oblique aponeurosis. Then expose the external inguinal ring and external oblique aponeurosis, open the aponeurosis and dissect and elevate the cord, in order to define whether the defect is direct or indirect. The procedure is slightly different for each kind of hernia.
For an indirect defect, identify the internal inguinal ring and remove all the adhesions and scar tissue around it. Dissect the sac from the cord structures up to the internal inguinal ring, isolating it circumferentially. Identify the nerves of the region, taking care not to damage or stretch them. After that, reduce the sac through the ring without ligating it because it may cause initial or chronic pain. Finally, dissect with a finger the parietal peritoneum from the posterior abdominal wall, creating enough room to accommodate the preperitoneal disc of the implant (Fig. 5.2).
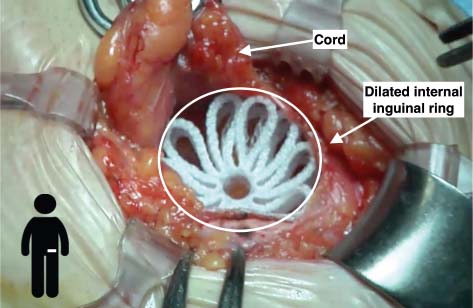
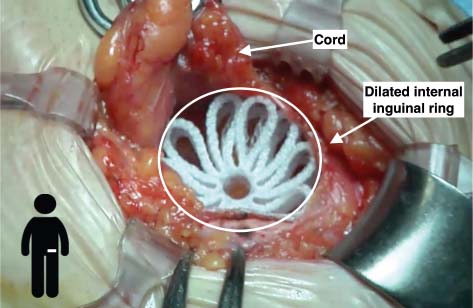
Fig. 5.2
Correct device positioning in a case of indirect defect
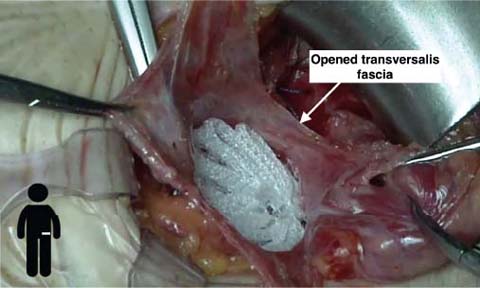
For a direct defect, dissect the sac from abdominal wall structures, paying attention to the nerves, removing adhesions and scar tissue around the hernia. Then open the transversalis fascia, with an incision as wide as necessary to detach the sac from the posterior wall. Dissect the parietal peritoneum with a finger and then check the integrity of the peritoneum (Fig. 5.3).