CHAPTER 34. Military Patient Transport
Christopher T. Paige and Timothy L. Hudson
Competencies



1. Describe military patient transport systems used during humanitarian and combat action.
2. Describe military patient movement through levels of care provided within the military medical system.
3. Identify different levels of military medical capability provided by each service (Air Force, Army, and Navy).
4. Identify military patient transport platforms (air and ground).
5. Identify the military medical training needed for transport personnel.
6. Recognize special military patient transport situations (search and rescue, peacetime).
This chapter describes the United States military patient transport system during combat operations. Not unlike the US medical system, the deployed military healthcare system is an integrated system that accomplishes triage and emergency treatment and then transports the patient to the appropriate level of care or returns the member to duty. In essence, the military builds a state-of-the-art trauma system in some of the most austere and dangerous locations for humanitarian or wartime contingences. 3 At the point of injury (POI), first aid is initiated. The patient is then rapidly transported through multiple medical support levels to include emergency medical response (Figure 34-1), advanced trauma surgery (Figure 34-2), and patient transport (Figures 34-3 and 34-4) towards hospital admission.
 |
| FIGURE 34-1 Two Army UH-60 Black Hawks arriving on scene to emergently evacuate injured soldiers. |
 |
| FIGURE 34-2 Military patient in advanced trauma surgery in forward location. |
 |
| FIGURE 34-3 Some military ground and air intratheater transport capabilities. |
 |
| FIGURE 34-4 Loading patients for intertheater patient transportation on Air Force C-17. |
Within the Department of Defense, the Air Force, Army, and Navy each have their own independent service surgeons general and doctrines. In the past, by design, the different medical services generally “took care of their own,” with each service caring for its members (i.e., Army soldiers seeing Army providers) and the Marines being cared for by the Navy. This system made sense because each of the military services is charged with a unique mission. The Navy and Marines primarily are tasked with the oceans and coastal areas, the Army with land security, and the Air Force with aerospace. However, today’s military operations are vastly more complicated, with the Navy, Marines, Army, and Air Force frequently sharing missions in and around the battle space in what are called Joint Operations. In addition, coalition partners and host nation military resources are frequently embedded together in operations. Joint Operations present a challenge to the military patient transport system. The interdependent Air Force, Army, and Navy medical transport capabilities must be interoperable and interchangeable. 11
LEVELS OF CARE
To best understand US military patient transport, one must first understand the different levels of patient care. After being introduced to the military medical levels of care, one can more easily understand the different transportation platforms, capacities, and resources found in the combat arena.
The military levels refer to the capability of care and are in sequential order of a patient’s movement through the military medical system. Figure 34-5 shows how traditional combat injuries move from a forward line of troops (front), level I, to definitive care (rear), level IV. This can be somewhat confusing at first as it is directly opposite to the civilian system of trauma levels. In the military system, the lower the level, the less capability to provide the patient with a full compliment of medical and surgical services. The purpose of creating graduating levels is for service members to be evaluated, treated, and released to duty at the lowest level possible. If medical care needed by the service member cannot be administered at a certain level of care, then they are transported to a higher level. Of note, in the urban environment, like Afghanistan and Iraq, where there is no “front,” transportation of a patient directly from level I to level III care for definitive care is not uncommon (Figure 34-6), 8 In recent conflicts surgical intervention has been moved closer to combat, which has blurred the lines between levels I and II. The levels presented here are adopted from the Army model but are similar among each service.
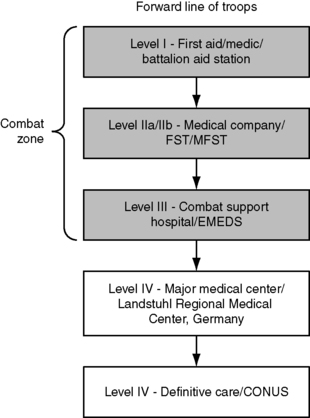 |
| FIGURE 34-5 Patient movement through levels in traditional battle lines; front, or forward line of troops. |
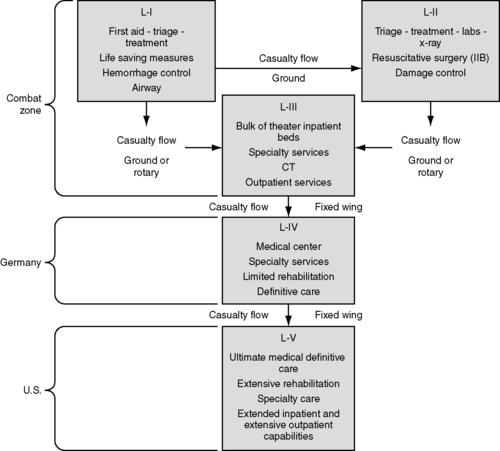 |
| FIGURE 34-6 Patient movement in urban environments such as Afghanistan and Iraq. |
Point of Injury Care
Point of injury care begins with patient assessment and triage, conducted immediately to identify whether life-saving measures must be taken. These measures encompass actions such as maintenance of airway, hemorrhage control, and prevention of shock. POI care is accomplished by the individual first on scene, which can be a nonmedical provider.
The nonmedical provider (combat soldier or marine) is trained to perform first-aid procedures to begin early life-saving treatment. The primary focus is stabilization of the patient condition and transport to a higher level of care. This is not the only care available to the warrior. The corpsman or medic is a trained emergency medical technician with the combat team that is on scene to provide trauma care. In addition to emergency care, many are trained in public health, disease prevention, and evaluation of diseases and injuries that are not related to battle.
Level I
For support of the many medical needs of a security force, small medical teams are placed far forward near combat operations (level I). 8 They are commonly referred to as Battalion Aid Stations (BASs). The team includes a physician, physician assistant, and medics. Traditionally, surgical intervention is minimal at the BAS. Recently, in an effort to bring more surgical capability closer to the POI, trauma teams that were built into the level II facility were brought forward and attached to the BAS. The Marines (staffed by Navy medical providers) moved a Forward Resuscitative Surgical System (FRSS) attached to the BAS, as did the Army with their Forward Surgical Team (FST) during the Iraq War in 2003. 7 This shift forward of surgical capability has blurred level I and level II care by increasing surgical capability closer to the POI.
Level II
Level II care has more capabilities than the BAS. These facilities, like level I, are 100% mobile (Figure 34-7). They do, however, have limited inpatient bed capacity with increased access to primary care, laboratory, emergency dental, combat stress/mental health, optometry, and basic radiography and can be augmented with surgical assets. Each service has similar but slightly modified capability at level II. The patient is triaged to determine transport priority based on current medical assets and the patient’s condition. At times, patients can be treated and returned to duty. Usually this decision is made immediately or before 72 hours. 8 If needed, emergent care, including resuscitation, is provided and more complete medical and surgical measures are taken. Because the level II facility is close to combat operations, the relative safety of the tactical situation at times dictates what extent of medical care can be administered. Recent data suggest minimal intervention at level II (2 hours or less) provides a better outcome. 5
 |
| FIGURE 34-7 Emergency entrance to level II facility. |
The Navy can place an Amphibious Ready Group (ARG) offshore during a humanitarian crisis or war. This ARG can include up to six ships with assault helicopters on their decks. These helicopters are used for assault but can double as both amphibious assault and patient transport platforms. One ship in the ARG is called a Casualty Receiving and Treatment Ship. It has up to 48 beds, six operating rooms (ORs), and 17 intensive care beds. See Box 34-1 for more information on level II capabilities among the services.
BOX 34-1
Level II Capabilities
| US Army | US Air Force | US Navy |
|---|---|---|
Treatment Platoon • Basic/emergency treatment is continued. • Packed Red Blood Cells (type O, Rh positive and negative), limited radiography, laboratory, and dental. • 20 to 40 cots with 72-hour holding. • No surgical capability. Forward Surgical Team (FST) • Continuous operations for up to 72 hours. • Life-saving resuscitative surgery, including general, orthopedic, and limited neurosurgical procedures. • Twenty-person team with one orthopedic and three general surgeons, two nurse anesthetists, critical care nurses, and technicians. • Operational within 1 hour of arrival at the supported company. • May be transported by ground, fixed-wing, or helicopter; some are airborne deployable. • Two operating tables for a maximum of 10 cases per day and for a total of 30 operations within 72 hours. • Postoperative intensive care for up to 8 patients for up to 6 hours. | Mobile Field Surgical Team (MFST) • Five-person team (general surgeon, orthopedist, anesthetist, emergency medicine physician, and OR nurse/technician). • Ten life-saving/limb-saving procedures in 24 to 48 hours from five backpacks. • Designed to augment an aid station or flight line clinic. Small Portable Expeditionary Air Medical Rapid Response (SPEARR) Team • Ten-person team: five-person MFST, three-person critical care transport/two-person preventive medicine team (flight surgeon, public health officer). • Stand alone capable: 7 days. • Ten life-saving/limb-saving procedures in 24 to 48 hours. • Designed to provide surgical support, basic primary care, postoperative critical care, and preventive medicine for early phase of deployment. • Highly mobile unit, with all equipment fitting in a one pallet-sized trailer. Expeditionary Medical Support (EMEDS) Basic • Medical and surgical support for an airbase, sick call, resuscitative surgery, dental care, limited laboratory and radiography capability. • Twenty-five staff includes SPEARR. • Four holding beds/one OR table. • Ten life-saving/limb-saving procedures in 24 to 48 hours. • Can augment: 10 beds/56-person staff (EMEDS + 10). | Forward Resuscitative Surgical System (FRSS) • Rapid assembly, highly mobile. • Resuscitative surgery for 18 patients within 48 hours without resupply. • One OR, two surgeons (general/orthopedic). • No holding capability. • No intrinsic evacuation capability. • Typically augmented with an en route care team to allow for evacuation capability. • Also requires host unit for logistics and security. Surgical Company • Provides surgical care for a Marine Expeditionary Force. Basis of allocation is one per infantry regiment. • Three ORs, 60-bed capability. • Patient holding time up to 72 hours. • Stabilizing surgical procedures. Casualty Receiving and Treatment Ships (CRTS) • Provides medical care for an Amphibious Ready Group. • Helicopter assets with casualty receiving capability. • Laboratory, radiography. • Fleet Surgical Team: three to four physicians, one surgeon, one certified registered nurse anesthetist, and support staff. • Augment: two orthopedic, two general surgeons, and oral maxillofacial surgeon with dental unit. • Excellent casualty flow capability because of large helicopter flight deck. • Forty-seven to 48 beds, four to six ORs, 17 intensive care beds. |
After stabilization, the patient is packaged for transport to the next level of care (level III), a Combat Support Hospital (CSH; pronounced “cash”; Army) or a Fleet Hospital (Navy).
Level III
Level III medical assets are the highest level of medical care available within the combat zone and contain the majority of hospital beds within the theater. 8 These level III facilities are similar in capability to a US civilian trauma center. Most are modular (Figure 34-8), with the exception of the Fleet Hospital. Modular build allows medical planners to tailor medical personnel and size of facility to actual or predicted requirements. The Fleet Hospital comes with up to 500 beds and is comparable with the Army level III hospital. It is equipped to provide resuscitation, initial wound surgery, and postoperative treatment. Patients at a level III hospital are stabilized for continued transport through the system or returned to duty. Level III capability is similar between the services and has proven to be interoperable, interchangeable, and interdependent with deployment rotations. 8 The Army CSH level III facilities can have up to 248 beds, which are usually divided into 48 intensive care unit (ICU) beds and 200 intermediate care beds (medical/surgical). Patients who need minimal care are handled by a 120-bed Minimal Care Medical Detachment. The surgical capability can provide up to six OR tables with a maximum of 96 operating hours per day. Surgical services include general, orthopedic, urologic, dental, and oral maxillofacial. Units include a robust blood bank, laboratory, radiology (to include computed tomographic [CT] scan and magnetic resonance imagery [MRI]), nutrition, and physical therapy and a specialty clinic section. This clinic provides patient services including sick call for staff and attached units. It also provides preventative medical surveillance capability to monitor disease and nonbattle injury. This clinic also provides outpatient psychiatry and inpatient neuropsychiatric consultation services.
 |
| FIGURE 34-8 Level III facility. Note proximity to airport for intertheater movement back to level IV or V facility. |
In the corps CSH, the hospital Company A (84 beds) and hospital Company B (164 beds), with support in headquarters sections and transportation element, are completely functional hospital companies. Company A provides hospitalization for up to 84 patients and consists of two wards that provide critical care nursing for up to 24 patients and three wards that provide intermediate care nursing for up to 60 patients. Company B provides hospitalization for up to 164 patients, consisting of two wards that provide critical care nursing for up to 24 patients and seven wards that provide intermediate care nursing for up to 140 patients.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree






