CHAPTER 14. Shock Management
Reneé Semonin Holleran
Competencies


 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

1. Describe the pathophysiology of shock.
2. Identify the patient at risk for shock.
3. Initiate critical interventions for management of shock before and during transport.
4. Identify the supportive care needed by the patient who is in shock.
5. Describe the treatment of selected coagulopathies.
Shock has been described as the “rude unhinging of the machinery of life or a momentary pause in the act of death.”52 The pathophysiology of shock causes inadequate tissue perfusion, which results in the body’s inability to meet its demands. This inability causes an alteration in cellular metabolism, which triggers the release of inflammatory mediators that promote a process that leads to coagulation disorders, continued hyperinflammatory response, organ damage, and death. 78 Despite the technologies and treatments available today, the mortality rate from shock remains high. Mortality and morbidity related to shock are best managed through prevention, early recognition, and rapid transport to definitive care. 2,16,26,28,33.34. and 35.51
Shock is divided into three major phases: a compensatory stage, a progressive stage, and an irreversible stage. Shock can result from alterations in circulating volume, cardiac pump function, and peripheral vascular resistance. It causes a myriad of physiologic changes in the nervous, respiratory, renal, and gastrointestinal systems. Alteration in circulating volume, particularly hemorrhage, is one of the most common causes of shock and one that is frequently encountered by transport teams.
A complication of hemorrhage is the development of coagulopathy, which can be caused by dilutional effects of massive transfusions, continued bleeding, and hypothermia. 7,23,29,44 Disseminated intravascular coagulation (DIC) is a potential secondary complication of shock. DIC may be found in critically ill patients when transport has been delayed. 2
This chapter discusses the etiology, pathophysiology, and initial management of shock. It also includes a discussion about coagulopathies that may challenge the care of patients in transport.
ETIOLOGY
Some of the causes of shock are summarized in Box 14-1. Although multiple causes have been identified as contributing to shock, the pathophysiology is essentially the same.
BOX 14-1
Etiology of Shock
Hemorrhagic: Acute blood loss from an internal or external vascular injury.
External: Penetrating trauma, amputation, and open fractures.
Internal: Injury (splenic, liver); fractures, particularly pelvic; body tissue injury; bleeding from other internal source such as GI tract; and esophageal varices.
Hypovolemia: Fluid loss such as from third spacing, burn injury, vomiting, diarrhea, diabetes mellitus, diabetes insipidus, and diuresis.
Neurogenic: Spinal cord injury; alteration in vascular tone from drugs, food, plants, and venom.
Anaphylaxis: Allergic reaction to a foreign substance including drugs, food, plants, and venom.
Obstructive: Obstruction of blood flow (e.g., from a tension pneumothorax or cardiac tamponade).
Cardiac: Pump failure that may result from a myocardial infarction, valvular malfunction, septal defect, right-sided infarct, or direct injury to the heart such as a myocardial contusion.
Sepsis: Infectious agent that compromises the host defense mechanism.
PATHOPHYSIOLOGY
The research on shock during the past 20 years has focused on the role of the immune system and the multisystem effects of clinical insult. The initial systemic inflammatory response that occurs after clinical insult is actually a protective mechanism. However, with prolonged inadequate tissue perfusion and consequential tissue oxygen debt, the body actually goes into a hyperinflammatory state that triggers a variety of systemic responses.
The immune system reacts with the activation of a complement cascade, which causes the release of cytokines such as tissue necrosis factor (TNF) and interleukin-1 (IN-1). In addition to cytokines, nitric oxide, reactive oxygen species, and growth factors are stimulated, which results in the triggering of polymorphonuclear neutrophils (PMNs), endothelium macrophages, and lymphocytes. 53 These substances lead to bronchoconstriction, platelet aggregation, capillary permeability, and resultant vasoconstriction and vasodilation. 60 Specific products used for shock resuscitation can also contribute to an inflammatory response. 53 Recent research has shown a decrease in multiple organ failure complications after shock when a decrease occurred in the amount of blood transfusions used during resuscitation. 27 This research may also affirm the role of the immune and inflammatory responses in shock.
Even when shock or inadequate perfusion has been recognized, the resultant tissue ischemia and cell death continues to incite an inflammatory response. This process is known as reperfusion and inflammatory injury. 43
Ischemic tissue in vulnerable organs converts xanthine dehydrogenase found in the vascular endothelium to xanthine oxidase (XO). Even when oxygen becomes available to ischemic tissues, the XO creates a burst of reactive oxygen metabolites that actually cause additional tissue injury. 60 Tissue injury stimulates more PMNs and the inflammatory process continues to contribute to multiple organ failure. 43
Systemic Inflammatory Response Syndrome
In 1977, Eisman, Beart, and Norton36 introduced a term called multiple organ failure. These authors described a man-made syndrome that involved principally the failure of the at least two major organ systems (i.e., pulmonary, renal, gastrointestinal, or hematologic). The authors tied it into an infectious process. 36
The mechanism by which bacteria destroys so many remote organs remains unknown. Various toxins have been suspected but not universally proven.
Another interesting point raised in this paper was the expense and the ethics involved in keeping these patients alive. 36
In the 1980s, several endogenous mediators were discovered that mimic a septic shock response in animal models. Multiple insults were also found to trigger these responses. 87 Soon, similar cascades were observed in patients, and reports began to appear in the literature to offer potential explanations as to why not all patients could be successfully resuscitated from an uncompensated or irreversible shock state. 59 However, many patients in whom septic shock, and eventually multiple organ failure and death, developed were discovered to not be infected at all.
In 1991, a consensus conference introduced the concept of systemic inflammatory response syndrome (SIRS) and the criteria to describe where patients fall on the continuum of shock. 15 These definitions are summarized in Box 14-2. This is the inflammatory model of shock or, as stated by Gross, “the rude unhinging of the machinery of life.”19
BOX 14-2
Definitions
Sepsis Syndrome
Clinical evidence of infection
Rectal temperature, >38.3° C or <35.6° C
Tachycardia (>90 beats per minute)
Tachypnea (>20 breaths per minute)
At least one of the manifestations of inadequate tissue function/perfusion:
• Alteration in mental status
• Hypoxemia (PaO 2 < 72 mm Hg at FiO 2 0.21; overt pulmonary disease not the direct cause of hypoxemia)
• Elevated plasma lactate level
• Oliguria (urine output, 30 mL or 0.5 mL/kg for at least 1 h)
Systemic Inflammatory Response Syndrome
Two or more of the following conditions:
• Temperature, >38° C or <36° C
• Heart rate, >90 beats per minute
• Respiratory rate, >20 breaths per minute or PaO 2 < 32 mm Hg
• White blood cell count, >12.10 9 /L, <4.10 9 /L, or >10% immature (band) forms
Sepsis
The systemic response to infection manifested by two or more of the conditions mentioned under SIRS (SIRS related to infection).
Severe Sepsis
Sepsis associated with organ dysfunction, hypoperfusion, or hypotension. Hypoperfusion and perfusion abnormalities may include, but are not limited to, lactic acidosis, oliguria, or acute alteration in mental status.
Septic Shock
Sepsis-induced hypotension despite adequate fluid resuscitation along with the presence of perfusion abnormalities that may include, but are not limited to, lactic acidosis, oliguria, or acute alteration in mental state. Patients who are receiving inotropic or vasopressor agents may not be hypotensive at the time that perfusion abnormalities are measured.
Multiple Organ Dysfunction Syndrome
The presence of altered organ function in an acutely ill patient such that homeostasis cannot be maintained without intervention.
Multiple Organ Dysfunction Syndrome
Bone15 has described multiple organ dysfunction syndrome (MODS) as a clinical syndrome characterized by the development of potentially reversible physiologic dysfunction in two or more organ systems. 15,33 This pathology can be caused by a variety of acute insults, including trauma, sepsis, and poison. Research has shown that little consensus exists on what exactly constitutes MODS. However, most experts agree that the following seven systems are generally included in the definition: cardiovascular, central nervous, gastrointestinal, hematologic, hepatic, renal, and respiratory systems.
The patient with MODS is generally transported after a referring center can no longer provide care. 2 These patients present a unique challenge because they are more likely to have multiple invasive lines, treatment with many medications, and complex ventilator settings. Chapter 12 discusses the ventilatory management of these cases.
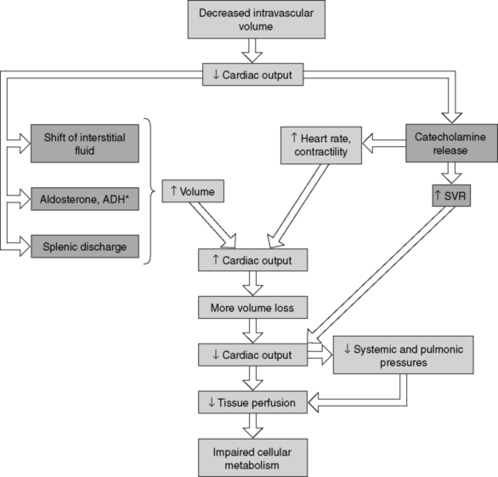
Cellular Response
A reduction in the amount of available oxygen causes an alteration in cellular metabolism, resulting in a cascade of significant cellular changes and leading to injury and death if interventions prove ineffective or are too late. Figures 14-1 and 14-2 illustrate the cellular and micropathophysiologic changes that occur during cellular ischemia. 20,38,59,61
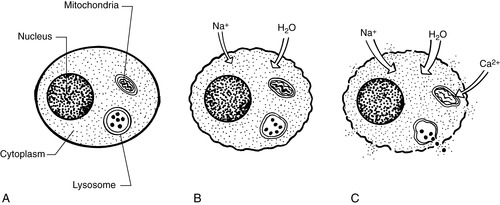 |
| FIGURE 14-1 A, Normal cell. B, Massive amounts of water and sodium enter cytoplasm, causing blebs to develop. C, Calcium changes in mitochondria cause destruction; lysosomes rupture, spilling proteolytic enzymes into cytoplasm; cell wall loses integrity, and cell dies. (Modified from Kitt S, et al: Emergency nursing, Philadelphia, 1995, Saunders.) |
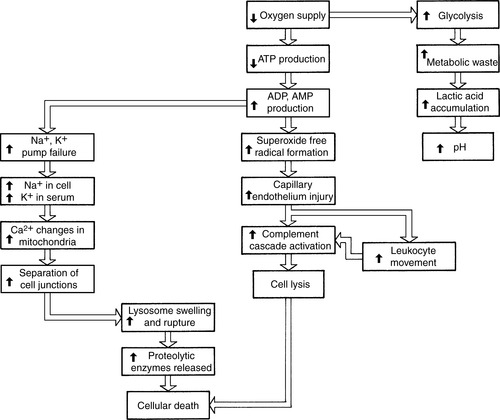 |
| FIGURE 14-2 Micropathophysiologic changes that occur during cellular ischemia.ATP, Adenosine triphosphate; ADP, adenosine diphosphate; AMP, adenosine monophosphate; Na +, sodium ion; K +, potassium ion; Ca2 +, calcium ion; pH, logarithm of reciprocal of hydrogen ion concentration. (Modified from Kitt S, et al: Emergency nursing, Philadelphia, 1995, Saunders.) |
Body Systems Response
The transport team must always be cognizant of the causes of shock and the subtlety of its signs and symptoms in its early stages. They must also take into account comorbid risk factors that cause additional stress on the patient’s body systems and that may increase a patient’s risk of compromise, even with a moderate illness or injury. Some of these factors include a history of cardiovascular disease, pulmonary disease, or diabetes. Research continues to show that shock needs to be treated and reversed as soon as possible to prevent additional injury and eventual death. 5,9,77
Regardless of the source of shock, if it is not quickly recognized, the concomitant changes that occur in blood pressure, blood flow, and volume and the alterations in oxygen transport that cause hypoxia lead to tissue hypoxia, organ dysfunction, multiple organ failure, and death. 1,23,49,60
As previously discussed, the lack of available oxygen to the cell initiates a cellular response that results in body system changes. As shown in Figure 14-3, the immune system reacts with the activation of a complement cascade that eventually releases cyto-kines such as TNF and IN-1. These cytokines are key in the production of cellular toxins, such as arachidonic acid, thromboxane, and leukotrienes. These substances lead to bronchoconstriction, platelet aggregation, capillary permeability, and vasoconstriction or vasodilation. 1,39,41
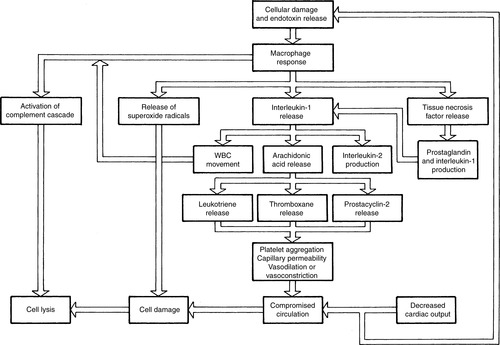 |
| FIGURE 14-3 Cascading response of immune system in shock. (Modified from Kitt S, et al: Emergency nursing, Philadelphia, 1995, Saunders.) |
Figure 14-4 summarizes the other system changes associated with the hypoxia of shock that result in some of the classic signs and symptoms of shock. These signs and symptoms include altered mental status, changes in skin color and temperature, and a decrease in or absence of urinary output because of inadequate perfusion to the kidneys, which initiates a compensatory response to conserve water. 1,2,4,5
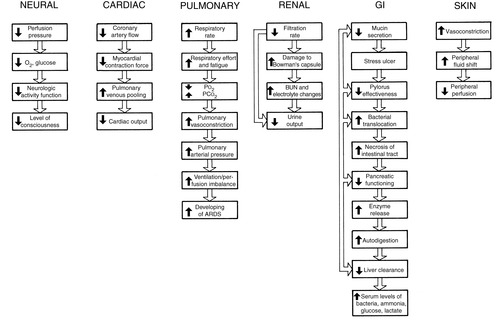 |
| FIGURE 14-4 Major organ system changes that occur from hypoxia associated with shock.O 2, Oxygen; P o2, partial pressure of oxygen; P co2, partial pressure of carbon dioxide; ARDS, adult respiratory distress syndrome; BUN, blood urea nitrogen. (Modified from Kitt S, et al: Emergency nursing, Philadelphia, 1995, Saunders.) |
STAGES
Shock has been divided into the following three specific stages: the compensatory stage, the progressive stage, and the irreversible stage. No matter what the origin of shock, a decrease in available oxygen triggers cellular responses, which in turn affect all body systems. 35
Compensatory
During the compensatory phase of shock, the body attempts to maintain perfusion in the face of illness or injury. Several compensatory mechanisms are stimulated so that the body may compensate and maintain end organ perfusion. The results of the triggering of these mechanisms, which include shifts of interstitial fluid, secretion of stress hormones, and increase in systemic vascular resistance, produce some of the classic signs and symptoms of shock. These signs and symptoms include tachycardia, tachypnea, pale skin, and diaphoresis. Figure 14-5 illustrates the compensatory mechanisms triggered in hypovolemic shock. This stage of shock is generally reversible.
 |
| FIGURE 14-5 Compensatory mechanisms triggered in hypovolemic shock. (From McCance KL, Huether SE: Pathophysiology: the biologic basis for disease in adults and children, ed 5, St Louis, 2006, Mosby.) |
Progressive
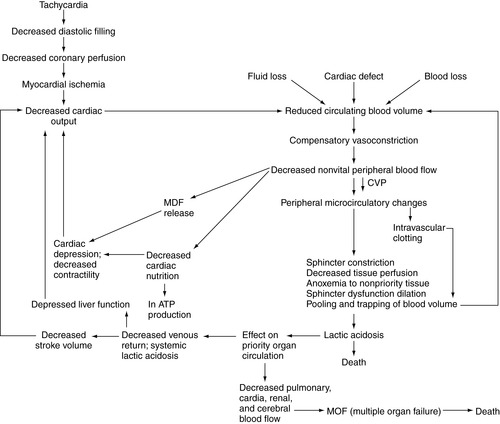
If the presence of shock goes unrecognized or the cause of it is not managed, the shock cycle continues to progress. The initial insult that caused shock continues to activate vicious cycles of compensatory mechanisms that, if not appropriately managed, lead to death. During this progressive phase, the effects of tissue hypoxia and anaerobic metabolism are experienced. 10.11. and 12. Cytokines such as TNF and the interleukins, especially 1 and 6, initiate the pathophysiologic changes that may eventually lead to multiple organ failure.
Irreversible
In the irreversible phase of shock the body becomes refractory to treatment. In the final stages of shock, the patient may still be alive, but treatments such as fluid resuscitation, antibiotic administration, and ventilatory management become ineffective (Figure 14-6). The reason this occurs remains unknown but is probably related to the hyperinflammatory response of the body in shock as previously discussed.
 |
| FIGURE 14-6 Compounding factors in irreversible shock. |
PATIENT ASSESSMENT AND SHOCK MANAGEMENT
The assessment and management of the patient in shock begins with the recognition that the patient is in shock. Early recognition of shock inversely affects the morbidity or mortality of the patient. Shock can be diagnosed on the basis of history and clinical signs. 2,37
Assessment
Inspection
▪ Determine the patient’s level of consciousness; restlessness, anxiety, and confusion may be indications of inadequate perfusion.
▪ Assess breathing effectiveness and respiratory rate; tachypnea occurs with increasing acidosis.
▪ Identify any source of uncontrolled bleeding. Inspect the chest, abdomen, and extremities.
▪ Assess the patient’s skin color and presence of any moisture; the patient in shock may be pale, ashen, and diaphoretic.
Auscultation
▪ Obtain blood pressure; the patient’s blood pressure may need to be palpated.
▪ Calculate the pulse pressure and monitor for trends in the blood pressure. A narrow pulse pressure indicates a fall in cardiac output and is an ominous sign.
▪ Listen to heart sounds; muffled heart tones may indicate a cardiac tamponade.
▪ Listen to breath sounds; absent breath sounds may indicate a pneumothorax or a hemothorax.
▪ Listen for bowel sounds; absent or hypoactive bowel sounds are common in shock.
Percussion
▪ Dullness in the chest may indicate blood in the thoracic cavity.
▪ Dullness in the abdomen may indicate blood in the peritoneal cavity.
Palpation
▪ Palpate central and peripheral pulses to assess adequate perfusion.
▪ Weak and thready pulse indicates decreased stroke volume as a result of hypovolemia.
Radiographic Studies
▪ Chest radiography is used to determine a pneumothorax or hemothorax.
▪ Computed tomographic (CT) scan of the chest is used to determine injury.
▪ Pelvic radiography is used to locate a fracture for a potential source of blood loss.
▪ Femur radiography.
▪ CT scan of the abdomen.
Other Studies
▪ Focus abdominal sonography for trauma (FAST).
▪ Diagnostic peritoneal examination (DPL).
Laboratory Studies
▪ Hemoglobin and hematocrit.
▪ Serum osmolarity.
▪ Electrolytes.
▪ Blood urea nitrogen (BUN) and creatinine.
▪ Lactate level.
▪ Arterial blood gases (ABGs).
▪ Clotting studies.
Management
1. Correction of the initial insult.
2. Maintenance of adequate oxygen delivery.
3. Correction of secondary consequences such as acidosis, hypothermia, and coagulopathy.
4. Identification and management of preexisting disease.
A complete assessment and general therapy are accomplished almost simultaneously and should proceed as shown in Box 14-3.
BOX 14-3
Steps in Initial Management of the Patient in Shock
1. Assess airway patency, administer 100% oxygen, perform advanced airway management as indicated.
2. Assess breathing effectiveness, perform decompression if indicated.
3. Inspect for and control active bleeding.
4. Assess perfusion: peripheral and central pulses, capillary refill, skin temperature, color, jugular veins.
5. Initiate fluid resuscitation, closely monitoring patient during resuscitation.
6. Assess neurologic function: AVPU, GCS, pupillary function, motor and sensory response; immobilize patient if indicated.
7. Assess skin and skeleton; note abnormalities, deformities of skeleton, potential sources of blood, volume loss.
8. Keep patient warm.
9. Apply monitoring devices: cardiac, pulse oximeter, end-tidal.
10. Check invasive lines if in place.
11. Check urinary catheter if in place; monitor output.
12. Review laboratory studies before transport when available.
13. Review radiographic and diagnostic studies when available.
Correction of Hypoxia
The goal for hypoxia during the initial resuscitation of the patient in shock is to correct the oxygen deficit that has occurred. The transport team should secure the patient’s airway if indicated and provide oxygenation as soon as possible. This must always be done with consideration for safety of both the patient and the team. Respiratory muscle effort is the major site of oxygen expenditure for the resting patient and may place undue metabolic demands on the heart. Assisted ventilation that provides maximal analgesia, sedation, and neuromuscular blockade may be necessary for the transport of a critically ill or injured patient. Mechanical ventilation of a critically ill or injured patient is discussed in Chapter 12.
Fluid Resuscitation
Fluid resuscitation has become one of the most controversial topics in shock management. Research has questioned some of the previously common methods used to manage shock in prehospital and transport environments.
The purpose of volume resuscitation is to restore oxygen transport and cellular uptake of needed oxygen, mitigate against the oxygen debt accumulation, repay a preresuscitation oxygen deficit, and prevent the complications of SIRS and the development of multiple organ failure. The prehospital and transport management of fluid resuscitation must pay careful attention to the long-term consequences of any intervention. 2,3,11,13,14,29,31,32,45,50,56,58,62,63,68,73,75,76,81,82,84,89,91,92
Multiple fluids have been used for resuscitation, including lactated Ringer’s, normal saline, hypertonic saline, Hetastarch, and Plasmanate. In hemorrhagic shock, blood and blood products are needed for resuscitation. Massive transfusion protocols have been developed in multiple centers and should be used as a guideline in the use of blood and blood products in patient resuscitation. However, some transport programs do not carry blood or blood products. Regardless of which fluids are chosen for resuscitation, the patient needs to be monitored closely for the effectiveness of resuscitation and the potential complications that may occur.
Research has shown that hypotension may be a protective mechanism. Unless the source of bleeding can be adequately managed in the prehospital care environment, aggressive resuscitation may do more harm than good. Increasing a patient’s blood pressure increases the risk of bleeding, may dislodge formed clots, and, depending on the resuscitation fluid, dilutes circulating volume and increases clotting time. Crystalloids and colloids do not carry oxygen, which is one of the primary survival needs for cells. 2,3,11,13,14,29,31,32,45,50,58,62,63,68,72,73,75,76,81,82,84,89,91,92
The amount of fluid needed by patients in shock, particularly those in hemorrhagic or hypovolemic shock, depends on the amount of intravascular volume depletion. During resuscitation, the transport team needs to monitor the patient closely for sufficiency of volume replacement. The patient’s blood pressure, pulse rate, level of consciousness, and urinary output (when available) provide parameters that can be monitored during transport. These parameters may also provide the transport team with indications of fluid overload. 2,22,37,70,71
The complications of massive fluid resuscitation include hypothermia, coagulopathy, metabolic derangements such as hypocalcemia and hypokalemia, organ dysfunction, and extravascular fluid shifts. These complications may lead to the development of adult respiratory distress syndrome (ARDS), sepsis syndrome, acute renal failure, DIC, pneumonia, multiple organ failure, and death. 69,79,89,90
Pneumatic Antishock Garment
One of the most common methods once used in the management of the injured patient in shock was the application of pneumatic antishock garments (PASG) or military antishock trousers (MAST). As the original name, MAST, suggests, this device was found to be of great use during the Vietnam War. However, little research had been done related to the effectiveness and potential complications that could occur once they were applied. 3,17,24,25,88,92
Mattox et al57 published a landmark study in 1989 that demonstrated several important points about the use of PASG. This study and other animal model studies proved that PASG did work but that their application in certain patient populations may actually increase patient morbidity and mortality rates. 57
Currently, the International Trauma Life Support Course22 recommends that the indications for the application of PASG in the prehospital environment include external hemorrhage that can be controlled (PASG possibly used initially until fluid replacement occurs), neurogenic shock without evidence of internal injuries, isolated fractures of legs without evidence of other internal injuries, and systolic blood pressure of less than 50 mm Hg (which still remains controversial). 22 Absolute contraindications to the use of PASG include pulmonary edema and bleeding that cannot be controlled. PASG must be used with caution in the woman who is pregnant, with pressure kept off the fetus. 22
When PASG are used during transport, the transport team needs to weigh the advantages over the disadvantages and monitor the patient closely. Continued use of PASG can lead to the development of decubiti and other stasis injuries. 5,22
Despite controversies, PASG are still used in some parts of the world to manage acute hemorrhage, particularly related to delivery. It might not be a bad idea to keep the PASG in a cool dry place and see what the future may bring.
Tourniquet Use
The use of tourniquets to control bleeding is not new. Recent information from the battlefields has shown a resurgence of the use of tourniquets. Tourniquets have been found to be of use in traumatic amputations related to battlefield injuries. Because of some successes, renewed interest has been seen in the use of tourniquets in civilian management of severe injuries with uncontrolled bleeding.
If tourniquets are used, the transport team must be familiar with their application and when they should be removed. 86
Pharmacologic Management
The pharmacologic management of shock depends on the source of the shock. For example, usually little need exists for pharmacologic agents in traumatic hemorrhagic shock. The primary therapy is administration of fluids, blood, and blood products. However, once the primary therapy has been initiated, pharmacologic management may be indicated if the patient’s condition does not improve.
Commonly used medications in the management of shock include inotropic agents, vasopressors, vasodilators, antibiotics, and steroids. Because dosages depend on age, size, and severity of the patient’s condition, the transport team needs to be familiar with the indications, dosages, and side effects of the medications that may be used. 2,4,5,30,34,40,54
Other Interventions
As summarized in Box 14-1, multiple causes of shock exist. When the blood flow is obstructed, as in cardiac tamponade and tension pneumothorax, the patient exhibits signs and symptoms of shock. Critical interventions in obstructive shock include pericardiocentesis and thoracic decompression. Although some disease states may induce a pericardial tamponade or tension pneumothorax and contribute to obstructive shock, the most common causes of these life-threatening maladies are blunt and penetrating thoracic trauma. 2,5,22
Pericardiocentesis is indicated for the patient in shock when blunt or penetrating trauma to the chest (particularly the sternum) has occurred and the patient is hypotensive and has bradycardia, distended neck veins, and muffled heart sounds. 2,5,22
Needle decompression or chest tube insertion is indicated when the patient is in shock and has severe respiratory distress, hypotension, bradycardia, jugular vein distention, and tracheal deviation. When the patient is intubated, difficulty in ventilation should alert the transport team to the potential of a tension pneumothorax, once again in the patient with a history of blunt and penetrating trauma. 2,5,22
Another source of a tension pneumothorax that should be considered by the transport team is barotrauma. Aggressive bagging or mechanical ventilation could cause a pneumothorax that contributes to a tension pneumothorax and obstructive shock. Chapter 12 discusses the potential complications related to the use of mechanical ventilation during transport.
Other interventions that may be used in the management of shock are the mechanical devices to assist circulation or increase tissue perfusion. Some of these devices include intraaortic balloon pumps (IAB), left ventricular assist devices (LVAD), and extracorporeal oxygenation devices (ECMO). The uses of these types of equipment require special skills and significant preparation. Chapter 23 contains a discussion about the indications and management of some of these devices. 74
Clinical Monitoring
Depending on the time, location, and initiation of interventions, the patient in shock may not have clinical monitoring devices in place. Multiple methods may be used to monitor the patient in shock, including hemodynamic and venous oxygen saturation (SvO 2) monitors. Box 14-4 contains a summary of some of these clinical monitors. 4,55,83
BOX 14-4
Cardiopulmonary and Metabolic Measurements in Shock
Arterial pressure
Left ventricular function (pulmonary artery catheter)
Cardiac output
Cardiac index
Mixed venous blood gases
Lactic level
Base deficit
Intramucosal pH
Central venous and pulmonary artery catheter pressures provide an index of the status of absolute and relative blood volume, the need for fluid replacement, and the effects of interventions. Accurate serial measurement of heart rate and rhythm, respiratory rate, cardiac filling pressure, cardiac output, tissue perfusion indices, and end organ function (mental state and urinary output) must be done when possible. 8,18,26
Regardless of the types of clinical monitor used, the transport team needs to ensure that they can be used during transport. All ports, intravenous and invasive lines, and monitors need to be secured and accessible and protected from the possibility of contamination, particularly when invasive lines are in place. 4 If invasive monitors are used, the transport team should document an initial reading once equipment has been changed and according to transport protocols or as the patient’s condition indicates during transport. 2
SELECTED CAUSES OF SHOCK
Hemorrhage
Description
Circulation can be compromised in various ways. Failure of circulation occurs either locally or systemically and results in shock. Systemic circulation failure is caused by inadequate blood volume or a pump defect. The first of three types of inadequate volume is hemorrhage, or loss of plasma and red cell mass from the vascular system. Hemorrhage is either internal or external; the amount depends on the vessel, the extent of damage, and the ability to form and maintain a clot. The effect of hemorrhage depends on the preexisting state of the cardiovascular, respiratory, renal, and hematologic systems. 16,64
Normal blood volume is approximately 7% of the ideal adult body weight (approximately 70 mL/kg) and 80 to 90 mL/kg in children. 5 In hemorrhage, a graded physiologic response is based on the percentage of blood volume lost acutely. The clinical symptoms progress as blood loss increases.
Changes in blood pressure at times may not be seen until 30% to 40% of the total blood volume is lost. Specific attention should be paid to pulse rate, respiratory rate, skin circulation, pulse pressure, and the patient’s mental status. 5
Intrathoracic and intraabdominal bleeding (cavitary hemorrhage) are well recognized as causes of hypovolemia in trauma. Significant losses from noncavitary causes (pelvic fracture, skin laceration, and multiple long bone fractures) may result in a 20% to 50% total blood loss, which places the patient in a severe shock state.
An isolated closed femur fracture can result in up to 2 L of blood lost in the fracture hematoma. In pelvic fractures, 40% to 50% of the total blood volume may be lost. The mortality rate in pelvic fracture is 6.4% to 15%; however, 42% to 70% of the deaths are attributed to blood loss. These patients need aggressive resuscitation.
Noncavitary blood losses contribute to additional loss of blood in 85.2% of patients with intraabdominal or intrathoracic hemorrhage. Blood losses occur 2 to 5 hours after the injury, so transport team members should be alert for delayed hypovolemia. 64
Treatment requires tamponade of the bleeding and supporting and splinting fractures. Fluid management includes administration of crystalloid, blood, and blood products. Knowledge that severe volume losses can occur with noncavitary bleeding is essential for early recognition to ensure proper treatment and prevent wasted time in searching for cavitary hemorrhage. 2,3,11,13,14,29,31,32,45,50,58,62,63,68,72,73,75,76,80,81,82,84,89,91,92
Indicators
A history of any of the following factors should lead to suspicion of hemorrhage:
Trauma to the thorax, abdomen, pelvis, or an extremity.
Melena or hematochezia.
Hematemesis.
Hemoptysis or epistaxis.
Vaginal bleeding.
Surgery.
Predisposing Conditions
The following conditions can predispose to hemorrhage:
Anemia.
Hemoglobinopathies.
Thrombocytopenia.
Liver disease.
Any hemorrhagic diathesis, hemophilia, or DIC.
Neoplastic disease.
Peptic ulcer disease.
Alcoholism.
Atherosclerosis.
Sepsis.
Surgery.
Causes
Internal Hemorrhage
Pleural cavity hemorrhage: intrathoracic vessel trauma, leaking aortic aneurysm, aortic dissection, ruptured varices, fracture.
Peritoneal cavity hemorrhage: liver, spleen, or any artery trauma; abdominal aneurysm; tumor; arteritis; volvulus; strangulated ovarian cyst.
Retroperitoneal hemorrhage: tumor, trauma fracture, ectopic pregnancy; soft tissue extremity trauma, fracture, venipuncture; skin trauma, purpura.
Bladder hemorrhage: tumor, transurethral prostatectomy.
Cavity hemorrhage: complication of surgery.
External Hemorrhage
Gastrointestinal (GI) tract hemorrhage (associated with hematemesis): inflammatory gastritis, peptic ulcer disease (PUD), esophagitis, and tumor of esophagus, stomach.
Endotracheal hemorrhage: esophageal lacerations, foreign body ingestion, abdominal trauma.
Vascular hemorrhage: varices, aneurysms, mesenteric occlusion, and hematologic disease.
GI tract (associated with hematochezia): ulcerative colitis (inflammatory), shigellosis (infectious), amebiasis, tumor, vascular hemorrhoids, volvulus, mesenteric occlusion; Meckel’s diverticulum (congenital).
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree






