Wrist Block
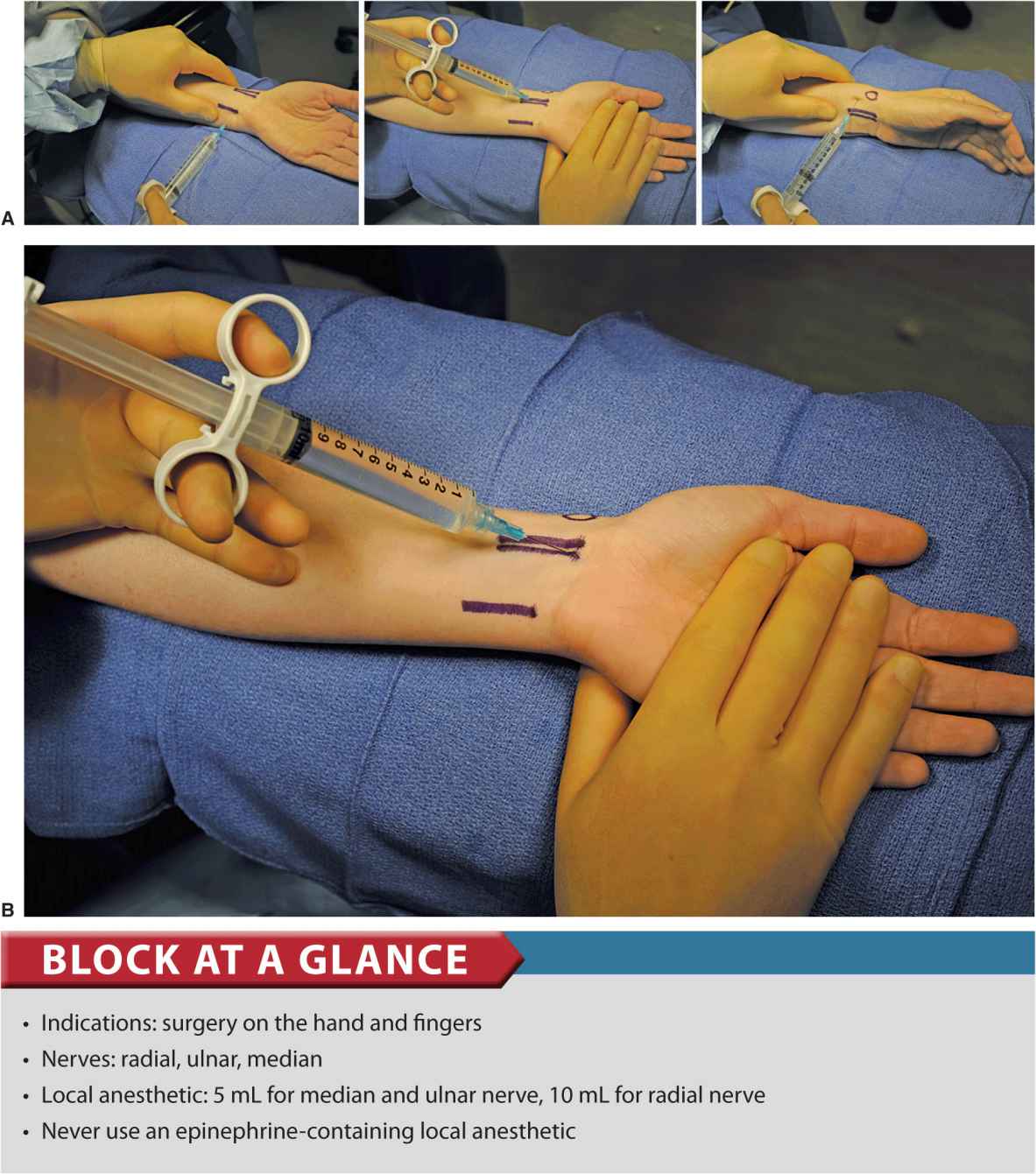
FIGURE 16-1. (A) Technique to accomplish a wrist block. (B) Median nerve block. Needle is inserted medial or lateral to the flexor palmaris longus tendon and carefully advanced to avoid paresthesia. Then 5 mL of local anesthetic is injected.
General Considerations
A wrist block consists of anesthetizing the terminal branches of the ulnar, median, and radial nerves at the level of the wrist. It is an infiltration technique that is simple to perform, essentially devoid of systemic complications, and highly effective for a variety of procedures on the hand and fingers. The relative simplicity, low risk of complications, and high efficacy of the procedure mandates this block to be a standard part of the armamentarium of an anesthesiologist. Several different techniques of wrist blockade and their modifications are in clinical use; in this chapter, however, we describe the one most commonly used at our institution. Wrist blocks are used often for carpal tunnel and hand and finger surgery.
Functional Anatomy
Innervation of the hand is shared by the ulnar, median, and radial nerves (Figure 16-2 and 16-3). The ulnar nerve provides sensory innervation to the skin of the fifth digit and the medial half of the fourth digit, and to the corresponding area of the palm. The same area is covered on the corresponding dorsal side of the hand. Motor branches innervate the three hypothenar muscles, the medial two lumbrical muscles, the palmaris brevis muscle, all the interossei, and the adductor pollicis muscle. The median nerve traverses the carpal tunnel and terminates as digital and recurrent branches. The digital branches supply the skin of the lateral three and a half digits and the corresponding area of the palm. Motor branches supply the two lateral lumbricals and the three thenar muscles (recurrent median branch).
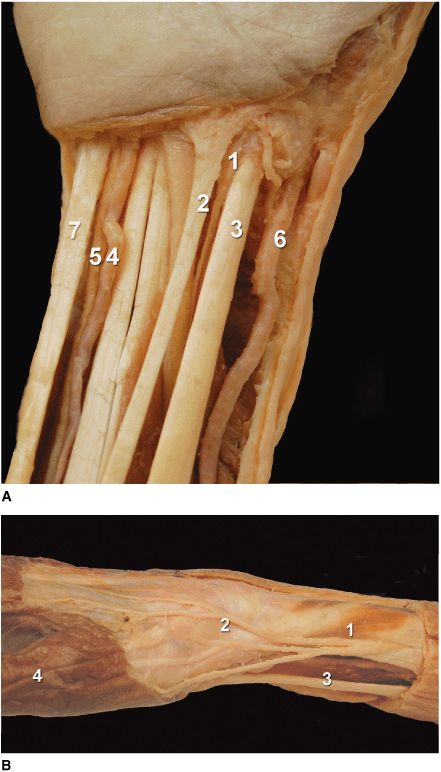
FIGURE 16-2. (A) Anatomy of the right wrist. ![]() median nerve.
median nerve. ![]() flexor palmaris longus.
flexor palmaris longus. ![]() flexor carpi radialis.
flexor carpi radialis. ![]() ulnar artery.
ulnar artery. ![]() Ulnar nerve.
Ulnar nerve. ![]() radial artery
radial artery ![]() flexor carpi ulnaris. (B) Anatomy of the right superficial radial nerve.
flexor carpi ulnaris. (B) Anatomy of the right superficial radial nerve. ![]() superficial radial nerve.
superficial radial nerve. ![]() radial styloid.
radial styloid. ![]() flexor carpi radialis tendon.
flexor carpi radialis tendon. ![]() thumb.
thumb.
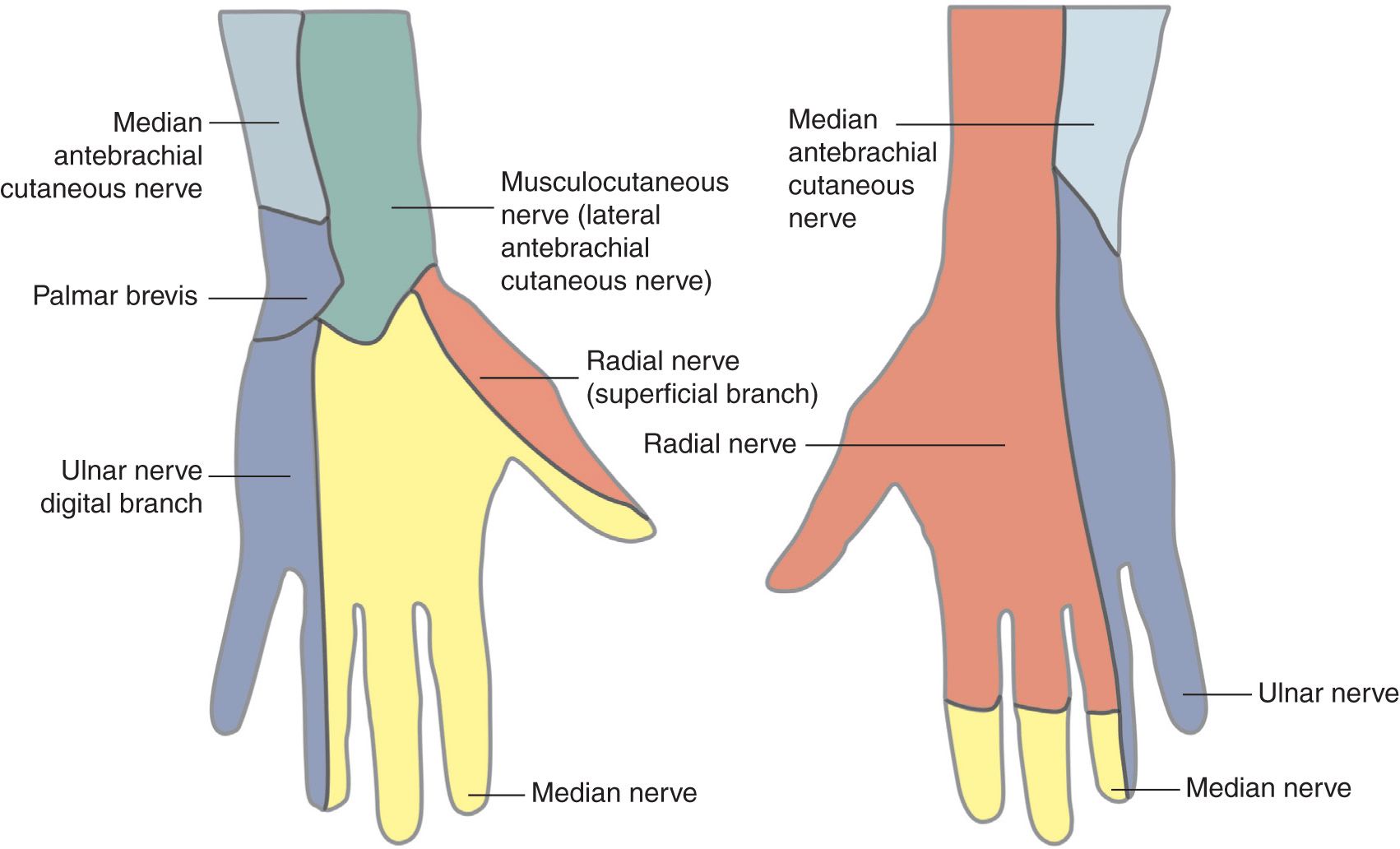
FIGURE 16-3. Cutaneous innervation of the left hand.
Although there is significant variability in the innervation of the ring and middle fingers, the skin on the anterior surface of the thumb is always supplied by the median nerve and that of the 5th finger by the ulnar nerve. The palmar digital branches of the median and ulnar nerves also innervate the nail beds of the respective digits.
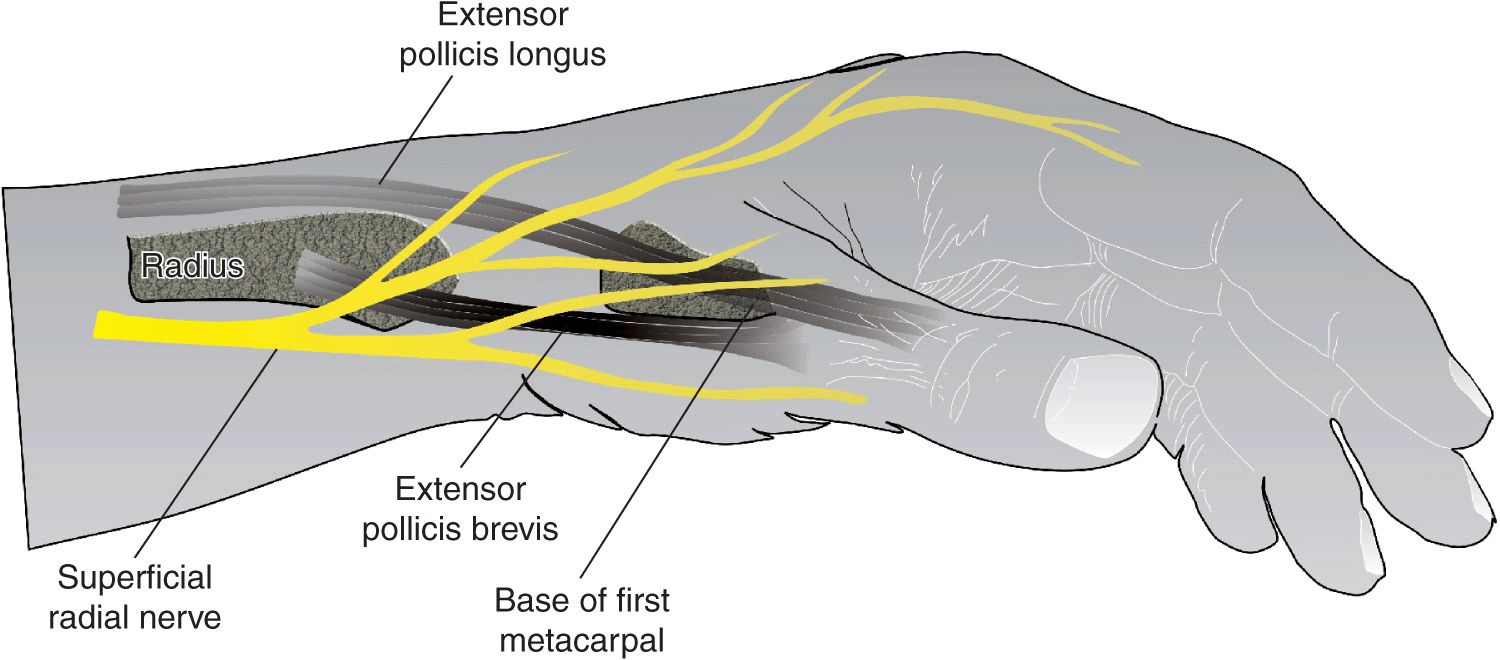
The radial nerve lies on the anterior aspect of the radial side of the forearm. About 7 cm above the wrist, the nerve deviates from the artery and emerges from the deep fascia, dividing into medial and lateral branches to supply sensation to the dorsum of the thumb and the dorsum of the hand (the first three and one-half digits as far as the distal interphalangeal joint).
Distribution of Blockade
Blocking the ulnar, median, and radial nerves results in anesthesia of the entire hand. The nerve contribution to innervation of the hand varies considerably; Figure 16-3 shows the most common arrangement.
Equipment
A standard regional anesthesia tray is prepared with the following equipment:
• Sterile towels and gauze packs
• Two 10-mL syringes containing local anesthetic
• A 1.5-inch, 25-gauge needle
Landmarks and Patient Positioning
The patient is positioned supine, with the arm in abduction. The wrist is best kept in slight extension.
Maneuvers to Facilitate Landmark Identification
The superficial branch of the radial nerve emerges from between the tendon of the brachioradialis and the radius just proximal to the easily palpable styloid process of the radius (circle) (Figure 16-4). Then it divides into the medial and lateral branches, which continue subcutaneously on the dorsum of the thumb and hand. Several of the branches pass superficially over the anatomic “snuffbox.”
FIGURE 16-4. Palpation of the radial styloid. The superficial radial nerve is blocked by an injection just proximal to the styloid.
The median nerve is located between the tendons of the flexor palmaris longus (white arrow) and the flexor carpi radialis (red arrow) (Figure 16-5A and B). The flexor palmaris longus tendon is usually the more prominent of the two, and it can be accentuated by asking the patient to oppose the thumb and 5th finger while flexing the wrist (Figure 16-6); the median nerve passes just lateral to it. The ulnar nerve passes between the ulnar artery and tendon of the flexor carpi ulnaris (Figure 16-7). The tendon of flexor carpi ulnaris is superficial to the ulnar nerve.
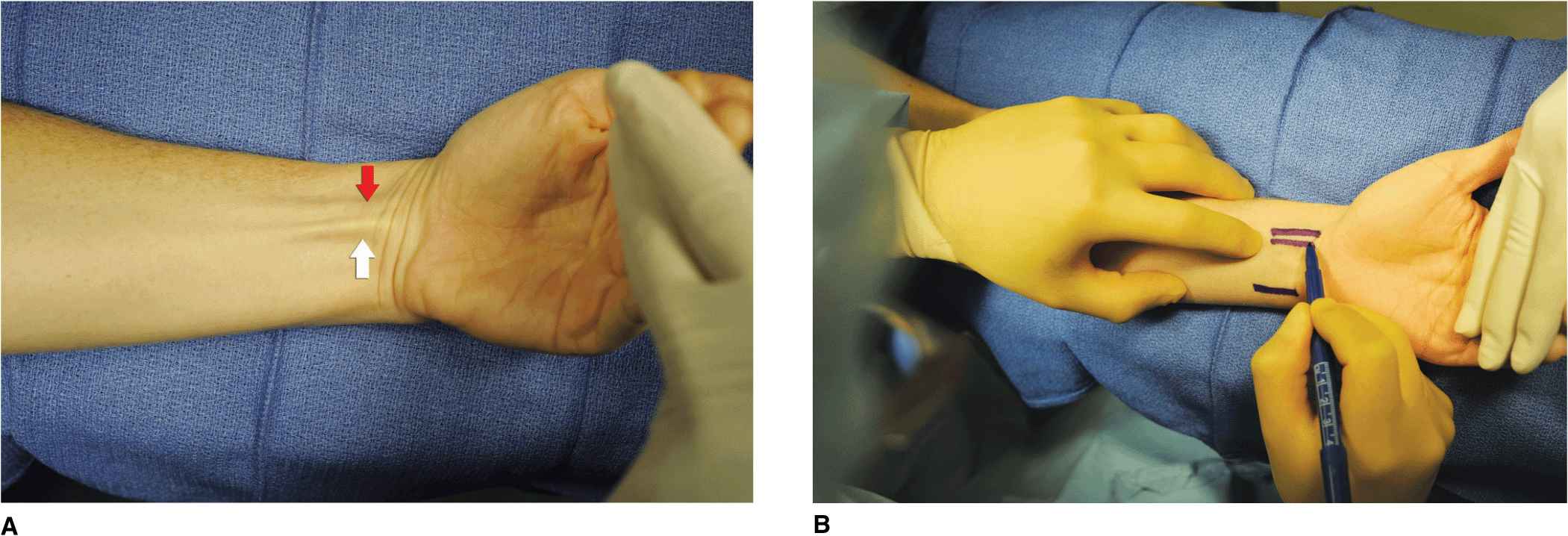
FIGURE 16-5. A maneuver to accentuate the tendons of the flexors of the wrist. (A) Shown are flexor palmaris longus (white arrow) and flexor carpi radialis (red arrow) tendons. (B) Outlining flexor palmaris longus tendon.
FIGURE 16-6. The flexor palmaris longus tendon can be accentuated by asking the patient to oppose the thumb and fifth finger while flexing the wrist.
FIGURE 16-7. Outlining flexor carpi ulnaris tendon.

Full access? Get Clinical Tree