Key Clinical Questions
- Infectious Mononucleosis
What are the major complications in Epstein–Barr virus–associated infectious mononucleosis (“mono”)?
What other viruses cause a mononucleosis-type clinical syndrome?
What are the appropriate diagnostic tests for acute Epstein–Barr virus infections?
What are the current treatment recommendations for Epstein–Barr virus–associated infectious mononucleosis?
- Varicella-Zoster Virus
What are the complications of adult varicella-zoster virus infection?
What are the treatment options for varicella-zoster virus infections?
What is the best way to treat postherpetic neuralgia?
What are the indications for the varicella-zoster vaccine in adults?
- Influenza
When should patients with influenza-like illness be hospitalized?
How good are rapid virus diagnostic tests for influenza virus?
How is influenza infection best treated with antiviral agents?
What are the major complications of acute influenza?
Infectious Mononucleosis
Viruses may infect any organ system of the body and present with common or rare clinical conditions. Viral infections may be trivial or life-threatening. Any given clinical syndrome, such as pneumonia, may have a multitude of viral causes. Additionally, some viruses, such as human cytomegalovirus (CMV), have protean clinical manifestations, including pneumonitis, colitis, encephalitis, and a mononucleosis-like syndrome. This chapter will discuss three common viruses in hospitalized patients: Epstein–Barr virus (EBV), varicella-zoster virus (VZV), and influenza virus, along with their complications.
Infectious mononucleosis is spread by close physical contact with infected secretions, and is often referred to as “kissing disease.” It is most often seen in adolescents and young adults and is not serious in most individuals. However, it can lead to significant time away from school or work, and may be associated with persistent fatigue and prolonged convalescence in some individuals.
Although other viruses produce a similar clinical syndrome, infectious mononucleosis is most often caused by acute EBV infection. Most people become infected with EBV before the age of 6. When EBV infection occurs early in life, it is usually asymptomatic or subclinical. Infection in young adulthood is more likely to lead to clinical “mono,” perhaps because of a more robust immune response. The major cell infected by EBV is the B lymphocyte; up to 20% of host B lymphocytes may be infected. Cellular immunity is heavily involved in containing EBV infection; the atypical lymphocytes seen in acute EBV infections are activated CD8+ T cells. The humoral immune system produces antibodies directed against the virus. For unclear reasons, antibodies are also produced against unrelated antigens found on sheep and horse red cells. These antibodies are known as heterophile antibodies, and they form the basis for the mononucleosis spot (“monospot”) test.
Infectious mononucleosis usually presents with exudative pharyngitis, fever, and symmetrically enlarged cervical lymph nodes. Sore throat may cause severe discomfort. Tonsillitis is common; if massive, “kissing tonsils” may impinge on the airway. Fever lasts from a few days to 2 weeks. The cervical lymphadenopathy can become generalized but usually subsides over 2 to 3 weeks. Splenomegaly, usually mild, is present in ˜50%. EBV needs to be distinguished from other causes of exudative pharyngitis, such as group A streptococcus, CMV, and acute human immunodeficiency virus (HIV) infection. Occasional complications (Table 206-1) include acute airway obstruction, spontaneous splenic rupture, rash, autoimmune hemolytic anemia, and neurologic syndromes such as meningoencephalitis, transverse myelitis, facial nerve palsy, optic neuritis, and Guillain–Barré syndrome.
|
Laboratory tests support the diagnosis of infectious mononucleosis but are not definitive. Most patients have an absolute lymphocyte count over 4500/mm3 and more than 10% atypical lymphocytes on peripheral blood smear. Total white blood cell counts are often elevated. Mildly elevated aminotransferase levels are common. The monospot test is a rapid latex agglutination assay for heterophile antibodies. Up to 90% of patients have heterophile antibodies at some time in the course of infectious mononucleosis. They persist for up to 1 year after acute EBV infection.
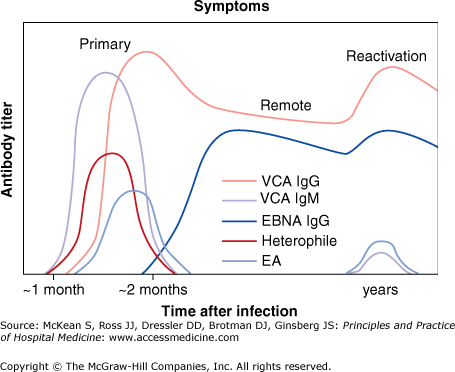
EBV-specific antibody assays are useful in patients with negative heterophile antibodies (see Figure 206-1). The viral capsid antigen (VCA) antibody test measures either specific immunoglobulin G (IgG) or IgM antibodies. Epstein–Barr nuclear antigen antibody (EBNA) test measures IgG, which rises during convalescence and stays elevated for life. Early antigen antibody assay (EA–D) is usually positive during acute infection. Polymerase chain reaction (PCR) assays are available but are rarely used in diagnosing infectious mononucleosis. EBV does not grow in routine tissue culture.
Figure 206-1
Serologic titers distinguish primary infection from remote infection. Immunoglobulin G (IgG) anti–viral capsid antigen (VCA) and IgM anti-VCA rise in concert with symptoms of primary infection and a positive heterophile test. After symptoms resolve, remote infection is characterized by Epstein–Barr nuclear antigen (EBNA) and IgG anti-VCA without early antigen (EA), although EA and IgM may reappear with or without symptoms on viral reactivation or Epstein–Barr virus–related neoplasia. (Reproduced from Gulley M, et al. J Mole Diagn 2008;10:272–292 with permission from the American Society for Investigative Pathology.)
Most patients with infectious mononucleosis have a good prognosis and recover quickly. However, some cases can be severe and last for several months. A minority of patients develop chronic fatigue syndrome, which may be more common in women and in those with preexisting mood disorders. If airway obstruction or difficulty breathing is observed, tracheotomy or endotracheal intubation should be considered. If splenic rupture has occurred, admission for attempted splenic preservation or splenectomy will be necessary.
Supportive care with rest, fluids, and moderate doses of acetaminophen, ibuprofen, or other antiinflammatories is the mainstay of care for infectious mononucleosis. Warm saltwater gargles may relieve the discomfort of sore throat. Use of steroids for EBV-associated infectious mononucleosis remains controversial. A recent meta-analysis suggests there is insufficient evidence for its use in routine cases (Table 206-2). Many clinicians use corticosteroids in mononucleosis complicated by impending airway obstruction, autoimmune hemolytic anemia, thrombocytopenia, aplastic anemia, or neurologic complications, but the evidence to support its use in these settings is not robust.
|
Impending airway obstruction, as defined by difficulty breathing, mandates admission to the hospital and close observation. Otolaryngology consult should be considered in these patients. The clinical benefit of acyclovir for treating acute infectious mononucleosis remains unclear based on published studies.
Airway obstruction with acute infectious mononucleosis is rare but serious. It usually requires close observation with the ability to do emergent tracheotomy or endotracheal intubation. Splenic rupture presents with acute abdominal pain (or, rarely, left-sided chest pain) and symptoms and signs of hypovolemia. Kehr sign (radiation of pain to the left shoulder) is present in 50% of cases. Splenic rupture may be spontaneous or due to trauma and usually occurs within 3 weeks after clinical symptoms have begun. Computed tomography (CT) abdomen and surgical consultation should be obtained if the diagnosis is suspected. Hemodynamically unstable patients should undergo splenectomy. In stable patients, close observation with nonoperative management or spleen-sparing interventions such as partial splenectomy, splenorrhaphy, and splenic artery embolization may be considered. Other complications that may require subspecialty consultation are autoimmune hemolytic anemia, encephalitis, and pneumonitis.
Individuals who play sports should be warned against participation for at least 3 weeks, when they may resume noncontact training. Those who do weight lifting or strenuous contact sports should wait at least 1 month after their illness began. It may be useful to obtain an ultrasound to document resolution of splenomegaly, but this practice is not accepted by many individuals. Patients should be warned that fatigue may take months to resolve.
Knowledge and treatment gaps exist in the current management of mononucleosis. Studies of the utility of ultrasound follow-up of splenomegaly in athletes, along with additional studies outlining the natural history of recovery, could help to define when individuals can safely return to normal activity. New antivirals need to be found and tested in the acute management of EBV-associated infectious mononucleosis. Although there is currently no EBV vaccine available, trials are under way to see if candidate vaccines are immunogenic and safe.
Varicella-Zoster Virus
Varicella (or chickenpox) is primary infection with the VZV virus. It usually occurs in childhood in temperate climates, and in adolescence or young adulthood in the tropics. Before the introduction of the varicella vaccine in 1996, there were an estimated four million cases of chickenpox in the United States each year. Since the introduction and widespread use of the vaccine in childhood, the incidence of chickenpox has been reduced in many populations by as much as 90%.
Primary infection with VZV occurs in the nasopharynx with spread to lymphoid tissue and specifically to memory CD4 + T cells, with adherence to cutaneous epithelia within the first few days following infection. Cell-free virus is present in skin vesicles and can infect sensory nerve endings and epithelia and result in latency of virus and sensory ganglia. Latent VZV genomes are localized to < 10% of sensory ganglia and neurons. Herpes zoster increases with increasing age and with other causes of decreased cellular immunity. Susceptible children are more likely to develop chickenpox from exposure to virus of varicella patients than from exposure to herpes zoster lesions.
Primary varicella infection is an illness of 3 to 5 days in duration, associated with rash, malaise, and low-grade fever. The characteristic rash of varicella consists of macules and papules that evolve into vesicles and crust over. Lesions are usually in different stages of development at any given time. The vesicle sits atop an erythematous base and has been referred to as a “dewdrop on a rose petal” because of its appearance. Lesions may become superinfected with staphylococci or streptococci, and necrotizing fasciitis is an occasional complication. Disseminated infection occurs in the immunocompromised patient. In adults, varicella pneumonia is common, occurring in at least 1 in 400 patients; asymptomatic radiologic infiltrates are even more common.

Full access? Get Clinical Tree