Vascular Emergencies: Introduction
Most vascular emergencies are due to either disruption of the blood vessel wall with bleeding (eg, from penetrating trauma) or to occlusion of the blood vessel lumen (eg, by an embolus or thrombus). The major consequences of these events are blood loss or acute distal ischemia. If vascular injury is untreated, hypotension or tissue necrosis may occur.
Vascular Emergencies Due to Trauma
Treat associated life-threatening head, thoracic, and abdominal injuries (Chapters 12, 22, 24, and 25).
Stop active bleeding from arterial or venous hemorrhage by gentle manual compression.
Avoid clamping the bleeding vessel because this will cause further injury.
Avoid the use of tourniquets.
Do not remove embedded objects because they may be preventing further bleeding.
(See also Chapter 11) Insert two or more large-bore (≥16-gauge) intravenous catheters. Two intravenous access sites are preferable if the patient is already in shock or is bleeding profusely.
While intravenous catheters are being inserted, draw blood for complete blood count (CBC), serum electrolytes, glucose and creatinine measurements, prothrombin time (PT), partial thromboplastin time (PTT), and typing and crossmatching (reserve 6–8 units of packed red blood cells or whole blood).
Begin intravenous infusion of crystalloid solutions (eg, normal saline or lactated Ringer’s) to support blood pressure. Up to 2–3 L of crystalloid solution may be given before blood products are administered. Replace blood. The number of units administered depends on the severity of existing blood loss and on anticipated loss from projected surgery. Use fresh whole blood whenever possible.
All fractures and joint dislocations associated with abnormal pulses should be carefully reduced and splinted to reduce further neurovascular damage. Control hemorrhage by pressure; avoid clamping vessels to stop hemorrhage. Consider adjunctive studies for further evaluation as appropriate (eg, computed tomography [CT] scan, angiography).
Keep ischemic limbs horizontal. Do not use tourniquets.
Provide adequate analgesia; if necessary, give narcotic analgesics.
All documented or suspected vascular injuries should be examined promptly by a general or vascular surgeon before the patient is transferred from the emergency department.
Hospitalize all patients with arterial or major venous injuries.
Acute vascular injury may result in either hemorrhage or tissue ischemia.
Obvious external hemorrhage is present in many patients. Occult bleeding into soft tissue, the retroperitoneum, the pelvis, or body cavities may also occur.
Ischemia from arterial injury must be recognized and treated promptly, because increased tissue pressure and swelling from ischemia further compromise arterial perfusion, and prolonged ischemia results in irreversible tissue damage.
Obvious or occult bleeding usually occurs following venous injury. It is rarely life-threatening except in the case of injuries to central veins (eg, vena cava) or their immediate branches (eg, femoral vein).
Tissue ischemia from venous trauma alone is rare, although venous obstruction and resultant tissue congestion may worsen preexisting tissue ischemia resulting from arterial injury.
Penetrating trauma is the most common cause of peripheral vascular injury and ranges in severity from innocuous simple puncture wounds to extensive wounds caused by high-velocity missiles. Penetrating injuries to the central vessels may lead to massive hemorrhage and death.
Blunt trauma may also cause vascular injury. Contusions or crushing injuries of an artery may cause either transmural disruption with hemorrhage, or partial disruption of the artery and elevation of the intima from an intramural hematoma (ie, dissection). Thrombosis of a segment of artery may also occur. Blunt trauma with dislocation of a joint may result in disruption of the arteries crossing that joint line, leading to ischemia distal to the site of injury (eg, disruption of the popliteal artery with posterior dislocation of the knee). Blunt trauma may also contribute indirectly to vascular occlusion by creating large hematomas near a blood vessel. Hematoma formation may lead to arterial spasm, distortion, or compartment syndromes, all of which may interfere with arterial flow.
Chemical injury to blood vessels is increasing in frequency. It is generally iatrogenic or associated with parenteral drug abuse. Intra-arterial injection of drugs that are chemically irritating to tissues (eg, barbiturates) causes occlusion of small peripheral vessels. If occlusion is severe, all or part of the limb may be lost. Extravasation of an intravenously administered chemical may also cause associated arterial spasm or tissue necrosis. Barbiturates, phenytoin, vasopressors, and chemotherapeutic agents (eg, doxorubicin) are notable examples. High doses of certain intravenously administered vasopressors (eg, dopamine) can cause intense peripheral vasoconstriction with ultimate digital ischemic necrosis.
Late sequelae associated with major vascular injuries include the development of false aneurysms and arteriovenous fistulas.
False aneurysms do not contain all three layers of the vessel wall (intima, media, and adventitia). They result from walled-off disruptions of vessel walls. They enlarge over time, may compress adjacent veins or nerves, and may rupture without warning.
Fistulas may occur after adjacent arteries and veins are injured simultaneously, usually as a result of stab wounds or missile injury. The fistula may enlarge over time and cause increased cardiac output if a large left-to-right shunting of blood is present. If the fistula involves the blood supply to an extremity, dilated veins may be observed in that extremity. Turbulent blood flow through the fistula results in an obvious thrill or bruit. Fistulas may also compress adjacent nerves or impede collateral circulation, or they may rupture, causing a severe hemorrhage.
If there is a wound in the vicinity of a major blood vessel, assume that vascular injury has occurred. The findings listed below may not appear for hours to days following a significant vascular injury, and absence of these findings does not rule out the possibility of vascular injury.
Clinical manifestations of vascular injury include an expanding or pulsating hematoma, to-and-fro or continuous murmurs of arteriovenous fistulas, a false aneurysm, loss of pulses, progressive swelling of the injured part, unexplained ischemia or dysfunction, and unilateral cool or pale extremities.
Perform a complete vascular examination unless treatment of other life-threatening injuries precludes it.
Palpate all peripheral pulses: carotid, axillary, brachial, radial, femoral, popliteal, dorsalis pedis, and posterior tibial.
The presence of blood flow in a peripheral vessel can be detected using a standard pocket Doppler apparatus. Any assessment of the normality of this flow requires concomitant pressure measurements or waveform analysis.
Auscultate over injured areas to detect bruits or murmurs.
Assess neurologic function. Paresthesia may be an early sign of developing vascular problems (eg, compartment syndrome).
Arteriography and CT scan with contrast or CTA are the imaging modalities to evaluate vascular injury. In addition, ultrasonography may be useful in specific circumstances (discussed below).
Caution: Diagnostic imaging should not be performed in a patient whose condition is unstable and who needs emergency laparotomy or thoracotomy. The procedure should be delayed until after resuscitation and treatment of the life-threatening emergency, either in the emergency department or in the operating room.
See also Chapter 23.
- History of blunt or penetrating trauma
- Consider concomitant injury to nonvascular structures
- CT scan and/or arteriography confirms diagnosis
Vascular injury to the neck is most often due to penetrating injuries; however, blunt trauma to the cervical vessels can result in intimal disruption, dissection, and thrombosis. Concomitant injury to nonvascular structures of the neck (eg, trachea, esophagus, and spinal cord) may also occur. The cervical spine must be protected until injury is excluded.
In penetrating trauma to the neck, two immediate concerns are massive hemorrhage and airway compromise secondary to a rapidly expanding hematoma.
Control hemorrhage, preferably with direct pressure, along with ongoing fluid resuscitation; neither of these measures should delay transport to the operating room for definitive repair. If a rapidly expanding hematoma is suspected, tracheal intubation via direct laryngoscopy or intubating bronchoscope should be conducted before compression of the trachea makes this procedure more difficult or impossible. Transtracheal jet insufflation and cricothyrotomy are methods of last resort; in this setting, emergency tracheostomy in the operating room is preferable.
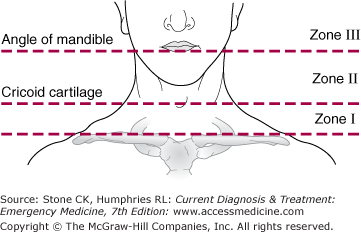
Further management is a function of the patient’s hemodynamic stability and the location of the wound. All actively bleeding, hemodynamically unstable patients are taken immediately to the operating room for surgical exploration. For stable patients with wounds that penetrate the platysma muscle, management is a function of the zone of the neck affected (Figure 40–1). Wounds should never be probed beyond the level of the platysma muscle in the emergency department.
These wounds are frequently associated with injury to the great vessels and require imaging with CT or angiography to exclude major arterial injury.
These injuries may be further evaluated by surgical exploration or imaging of the vessels and nonvascular structures with CT or angiography at the discretion of the attending surgeon.
Because the relationship of the blood vessels to the base of the skull makes surgical exploration and distal control of hemorrhage difficult, preoperative imaging with CT or angiography should be conducted to define the injury and help plan the surgical approach.
Blunt trauma to the carotid artery can result in intimal disruption, dissection, and thrombosis leading to acute cerebral ischemia manifest as a gross hemispheric neurologic deficit not explained by intracranial trauma. Conduct emergent imaging of the neck arteries with CTA or conventional angiography.
The use of multiplanar CT scanning with arterial enhanced imaging allow the neck vessels to be evaluated for injuries to include complete or partial transaction, arteriovenous fistula, pseudoaneurysms or thrombosis. In addition, conventional arteriography may be required in addition to CT in zone I and III injuries.
Asymptomatic patients with mild neck injuries due to blunt trauma or penetrating injuries that do not cross the platysma muscle may be discharged from the emergency department. Hospitalize all other patients with neck injuries, and consult with a general or vascular surgeon.
See also Chapter 24.
- Significant mechanism of thoracic trauma
- Tearing retrosternal or interscapular pain, dysphagia, hoarseness, or dyspnea
- In blunt trauma, less than half of patients will have visible signs of chest wall injury
- CT scan or TEE confirms diagnosis
Vascular injury to the chest occurs secondary to both penetrating and blunt trauma. If bleeding is not contained within fascial planes, these injuries can lead to exsanguination and death, often before the patient arrives in the emergency department. A high degree of suspicion for this type of injury must be maintained in any patient with a significant mechanism of thoracic trauma. CT with contrast has become the diagnostic study of choice in evaluating vascular injury in a hemodynamically stable patient with chest trauma.
Penetrating and blunt trauma may cause thoracic aortic injury (TAI). Though penetrating TAI may be caused by any variety of objects or weapons, blunt TAI involves large, violent deceleration forces (eg, falls, motor vehicle collisions including occupant ejection or auto-pedestrian). The greatest risk of TAI in a motor vehicle collision exists when the impact occurs on the same side of the vehicle as the occupant, when there is greater than 15 in of intrusion into the passenger compartment, and when the overall change in velocity experienced by the vehicle and its occupants is greater than 20 miles/h. A significant mechanism of injury should heighten suspicion of blunt TAI, because less than half of these patients will have visible signs of chest wall injury.
Patients may complain of tearing retrosternal or inter-scapular pain. Less frequently, dysphagia, hoarseness, stridor, or shortness of breath is present. The physical examination often reveals no external evidence of chest wall injury. Classically, a difference in upper-extremity pulses and a harsh systolic murmur across the precordium and in the interscapular area are noted. Signs and symptoms of shock may be present.
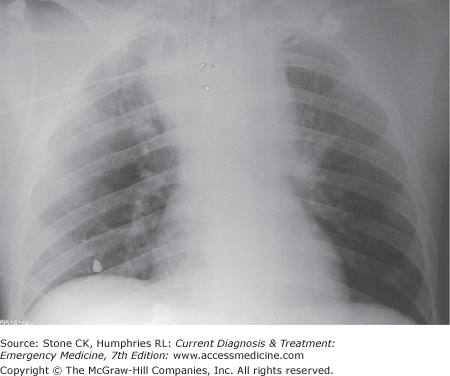
The chest X-ray is frequently the first imaging study obtained (Figure 40–2); the classic chest X-ray findings associated with TAI are listed in Table 40–1. However, 7% of patients with TAI can have a normal chest X-ray and further imaging studies may be warranted, based on clinical suspicion and mechanism of injury. In the past, aortography had been the study of choice in evaluating TAIs. However, CT scan has emerged as the study of choice after initial chest X-ray. It is more readily available than aortography and less invasive, and prospective clinical trials have shown spiral CT scan to be 100% sensitive and 99.7% specific in diagnosing TAI following blunt trauma. In centers where transesophageal echocardiography (TEE) is readily available, it is a highly sensitive (98%) and specific (100%) modality for diagnosing TAI. TEE can be done at the bedside, requires no contrast dye, and evaluates real-time cardiac function.
|
Patients with TAI will require emergency consultation with a vascular or thoracic surgeon. In the emergency department, it is important to maintain intravascular volume with crystalloid solutions and blood products. Systolic blood pressure should be lowered to less than 120 mm Hg. Exsanguinating hemorrhage may require emergency thoracotomy for the control of bleeding.
- Usually due to penetrating thoracic or abdominal injury
- Rapidly expanding hemothorax on chest X-ray
Most patients present with penetrating chest or abdominal trauma and rapidly expanding hemothorax, visible on chest X-ray. Rarely, blunt chest trauma is associated with pulmonary vascular injury.
Most patients can be managed with a 36–42 F chest tube that uses suction and allows the lung to reexpand and tamponade the bleeding vessel. Continued massive bleeding requires prompt surgery. Consider the use of autotransfusion. Prompt consultation with a general, vascular, or thoracic surgeon is required, because exsanguination can occur rapidly. Hospitalization is indicated for all patients.
See also Chapter 25.
- History of abdominal trauma
- Signs and symptoms of shock that fail to respond to resuscitation efforts
Patients with injuries to major vessels within the abdominal cavity present mainly with hemorrhagic shock that fails to respond to resuscitative efforts. In hemodynamically stable patients, CT with contrast is used to evaluate intrabdominal vascular and solid organ injury.
Immediate operation is the only effective treatment for abdominal vascular injuries. Support blood pressure with infusion of intravenous fluids (colloid or crystalloid solutions) until surgery can be performed. Packed red blood cells or whole blood should be used as soon as available.
- History of blunt or penetrating trauma
- Presence of a pulse does not rule out vessel injury
- Use CT or arteriography to evaluate
Vascular injuries are present in 25–35% of patients with penetrating trauma to the extremities. Occasionally vascular trauma is present without the usual physical findings, and the presence of a pulse does not rule out injury to the vessel. Imaging should be considered whenever the weapon’s trajectory has passed close to major blood vessels.
Vascular injury may also occur after blunt trauma, especially if fractures and joint dislocations are present. Even if the pulse is restored with splinting and traction, an arteriogram is necessary to rule out significant injury to the intima.
Posterior dislocation of the knee is associated with popliteal artery injury in half of cases, and arteriography is therefore mandatory.
Stabilize the patient, and stop hemorrhage as outlined above. Splint fractures. Do not clamp vessels or use a tourniquet.
All patients with suspected vascular injury should undego diagnostic imaging. CT angiography (CTA) in now the primary limaging modality for evaluating extremity arterial injuries in both blunt and penetratig extremity injuries. Obtain general or vascular surgical consultation for all penetrating extremity injuries.
- History of trauma
- Injuries to major venous structures manifested by progressive hemorrhagic shock (not ischemia)
- Venography may aid diagnosis
Trauma to peripheral veins without associated arterial injury usually does not require operative correction; however, disruption of the central large veins (vena cava or its immediate branches, subclavian or iliac veins)—especially where they are not enclosed by dense fascia or muscles—requires prompt operation.
Venous injury is usually manifested by hemorrhage, not ischemia. Patients with bleeding from the central veins present with progressive hemorrhagic shock (Chapter 9). Superior vena cava and subclavian vein hemorrhage is usually associated with hemothorax visible on chest X-ray.
In contrast, hemorrhage from the inferior vena cava and iliac vein is more difficult to detect. The only common finding is progressive hemorrhagic shock, and many of these injuries are not suspected before they are discovered at surgery.because most patients are too unstable to allow detailed radiologic evaluation.
Surgical correction in the operating room is indicated.
Vascular Emergencies Not Due to Trauma
- History of arrhythmia, myocardial infarction, valvular disease, or atherosclerosis may be presen
- Pain, paresthesias, and coolness of affectedextremity
- Pale, mottled, cyanotic limb with decreased or absent pulses
- Angiography confirms diagnosis
Acute arterial occlusion may be caused by an embolus, thrombosis, or trauma to an artery. Occlusion leads to distal ischemia, which if not corrected can progress to irreversible tissue damage and necrosis.
Embolic occlusion is caused by the dislodgment of an intravascular thrombus that travels distally and occludes a smaller artery. The majority of thrombi originate in the heart, but they may come from anywhere within the vascular system. A history of arrhythmia, myocardial infarction, or valvular heart disease suggests an embolic cause for acute peripheral ischemia.

Full access? Get Clinical Tree