Critical care ultrasonography (CCUS, or point-of-care ultrasound) has become increasingly popular in the management of critically ill patients as ultrasound technology has progressively become more portable, less expensive, and yet capable of high-quality imaging. Conceptually, CCUS functions as an extension of the physical examination. It is immediately available at the bedside, is noninvasive, and in skilled hands provides a wealth of information that can be used to narrow differential diagnoses and to initiate or modify treatment. CCUS is best used to complement results from other types of imaging, tests, and examinations and is not intended to replace them. Of the very broad range of techniques that comprise CCUS, in this chapter we will focus primarily on the use of ultrasound to evaluate cardiorespiratory status.
I. USE OF CRITICAL CARE ULTRASONOGRAPHY
A. Pros: The use of ultrasound at the patient’s bedside allows for rapid and noninvasive scanning. It can be used as an extension of the physical exam and be repeated often to monitor the progress of therapy or to evaluate an acute change in status. It does not involve risks associated with patient transport or radiation.
B. Cons: Implementation of a high-quality point-of-care ultrasound program in any ICU requires an initial outlay of funding for equipment and time for training of personnel. Equipment must be maintained and quality assurance programs need to be established to ensure safety and accuracy. The critical care physician may encounter difficulty obtaining adequate scanning windows due to the patient’s condition (pneumothorax, intra-abdominal free air, surgical dressings, and/or casts). Furthermore, the patient’s hemodynamics may be too unstable to tolerate a change in position to facilitate appropriate ultrasound scanning.
II. ULTRASOUND PHYSICS
A. The wavelength of a sound wave is the distance between two repetitive points along a single cycle. The wavelength helps to determine spatial resolution. The shorter the wavelength, the better the resolution. The frequency of a wave is the number of cycles per second. High-frequency waves provide excellent near-field resolution but poor tissue penetration, as they are subject to attenuation. Conversely, low-frequency waves offer improved tissue penetration, allowing visualization of deeper structures, but poor resolution. Thus we use a high-frequency probe for visualization of relatively superficial vascular structures, but a lower frequency probe for echocardiography of the heart.
B. Spatial resolution differs from temporal resolution. Spatial resolution relates to the ability to determine the location of a structure in space. Temporal resolution relates to the ability to determine the position of a structure at a particular instant in time. Temporal resolution is determined by the pulse repetition frequency (PRF). The higher the PRF, the higher the temporal resolution. A higher PRF increases the number of frames per second, and this allows for a smooth echo loop. This becomes important when assessing a fast-moving structure such as the heart.
C. Doppler ultrasonography is of great value in the assessment and quantification of blood flow through the heart (under both normal and pathologic conditions). Doppler techniques are divided into pulse wave Doppler, continuous wave Doppler, and color Doppler. Pulse wave Doppler (PWD) is used to measure flow velocities at a single defined location, such as at a point (defined by the sampling volume) in the left ventricular outflow tract. However, the maximum velocities that it can accurately measure is limited, beyond which PWD is susceptible to a form of sampling error called aliasing. Continuous wave Doppler (CWD) on the other hand, is not limited by aliasing and can be used to measure very high flow velocities (such as those from a stenotic aortic valve). However, the trade-off here is range ambiguity, that is, CWD cannot identify the precise location of the maximum velocity—it simply measures the maximum velocity anywhere in the path of the ultrasound beam. Color Doppler is a form of pulsed Doppler (and thus subject to aliasing) that measures flow at multiple sampling volumes on a two-dimensional grid rather than along a single line. One important caveat to the use of these techniques is that they are all angle dependent. In other words, they are accurate when the angle of the transducer beam is <20° to the direction of blood flow. Consequently, Doppler measurements may underestimate true flows, or provide inconsistent values on serial examination. Doppler examinations are not part of most basic critical care ultrasound protocols.
D. An important ultrasound feature for echocardiography that is frequently used in the ICU and the operating room is M-mode or motion mode. M-mode uses a single scan line of information and therefore provides the highest temporal resolution. This is useful for accurately measuring the size of structures such as the IVC or maximum aortic valve opening (see Figs. 3.1F and 3.2D).
III. CARDIAC ULTRASOUND: It is important to emphasize that intensivist-performed echocardiography is different from a formal cardiology echocardiographic exam. The critical care physician performs a “goal-directed” examination, designed to answer a specific question (most commonly, why is my patient hemodynamically unstable?), not a comprehensive examination. The primary skills involved in basic critical care ultrasound are image acquisition and pattern recognition. The critical care physician also uses the ultrasound as a monitoring tool, to evaluate the effect of his or her intervention. The real-time acquisition and interpretation of images in an acutely unstable patient that are then interpreted in the context of the patients’ physiology is the hallmark of critical care echocardiography. ICU echocardiography can be broadly divided into basic and advanced categories. The scope of basic, goal-directed critical care echocardiography (GDE) has been defined by a number of authorities and will be the focus of this chapter. Practitioners should have an awareness of their limitations when it comes to echocardiography, and help from more experienced echocardiographers or cardiologists should be freely sought to resolve equivocal findings.
A. Essential Views for Goal-Directed Echocardiography (see Fig. 3.1): It is helpful to establish a sequence of images that are obtained in each patient to maximize efficiency. Many ICU physicians follow the following sequence: Parasternal long-axis (PLAX), parasternal short-axis (PSAX—midpapillary view), apical four chamber (A4C), subcostal four chamber (SC), and subcostal inferior vena cava (IVC) views. This sequence may be modified depending on the clinical situation—for example, during CPR it is most practical to begin with the subcostal four-chamber view (which will not interrupt chest compressions).
B. Using Goal-Directed Echocardiography in the Hemodynamically Unstable Patient: Acute hypotension is often caused by hypovolemia, left ventricular or right ventricular dysfunction, severe valvular disease (such as acute regurgitation), or pericardial tamponade. GDE can pick up all these findings, which are then integrated with the patient’s history to categorize shock into one of the classic pathophysiologic mechanisms (hypovolemic, cardiogenic, obstructive, and distributive). A finding should be confirmed in at least two orthogonal views to reduce the risk of misinterpretation.
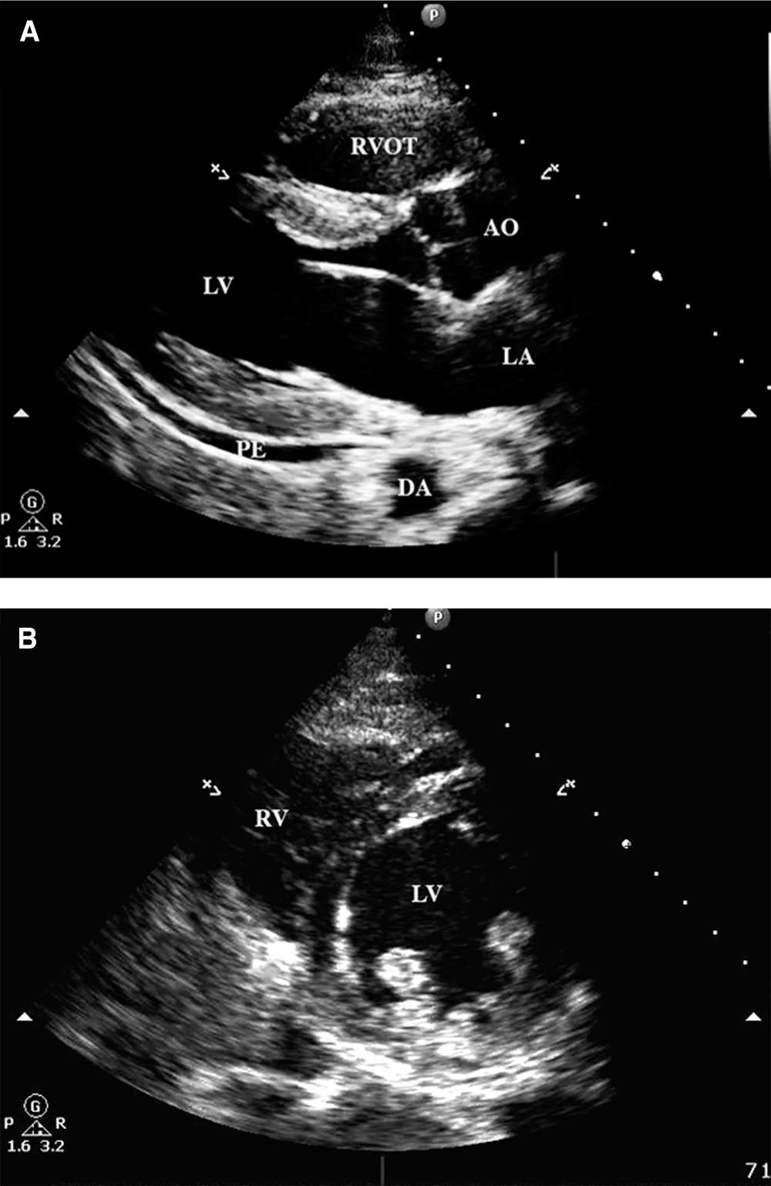
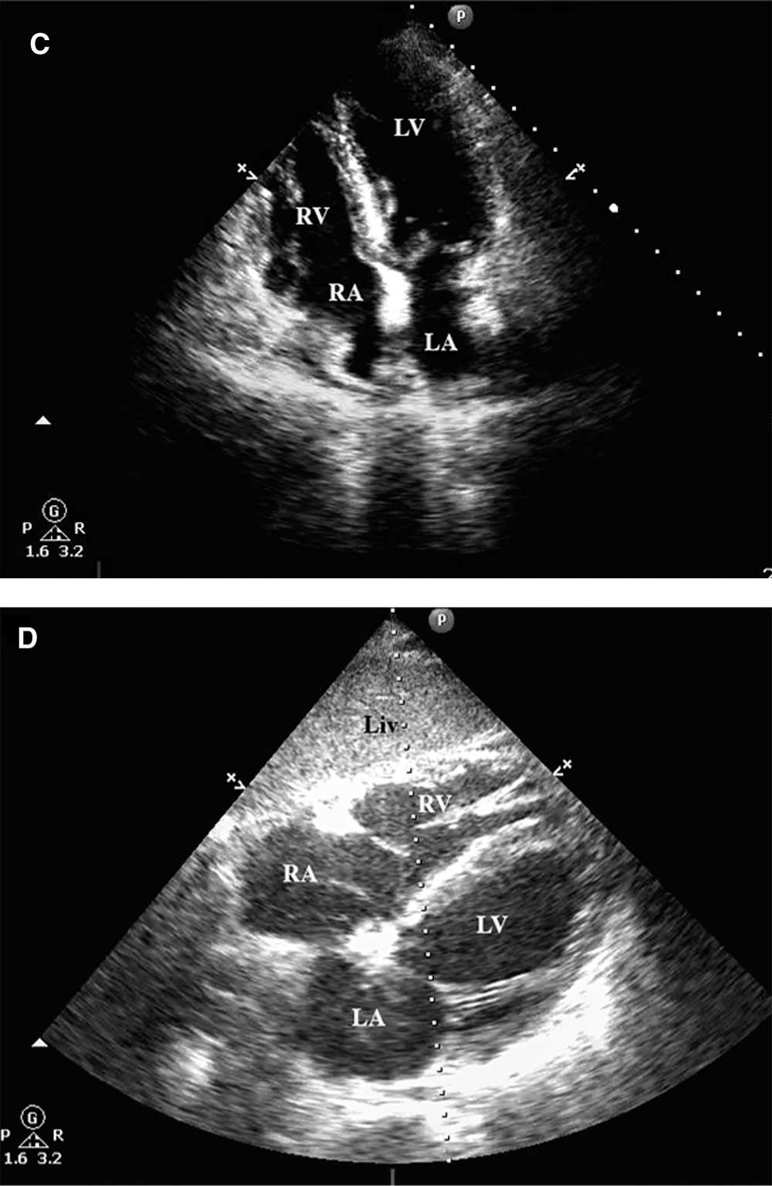
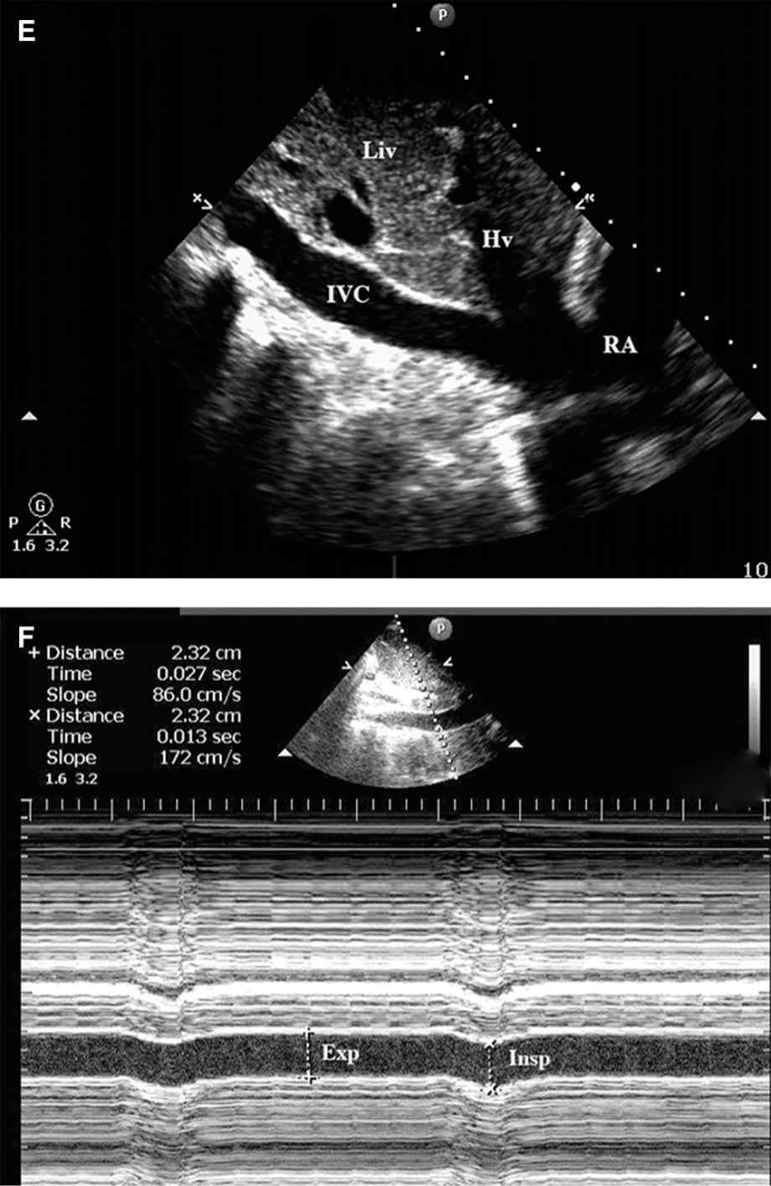
FIGURE 3.1 Transthoracic echocardiograms showing the views needed for a goal-directed echocardiographic examination in the ICU. Salient anatomic features are noted on the figures. (A) Parasternal long-axis view in diastole (mitral valve wide open; aortic valve closed). Note the small posterior pericardial effusion (PE); (B) Parasternal short-axis view. (C) Apical four-chamber view; (D) Subcostal four-chamber view; (E) Visualization of the inferior vena cava; (F) M-mode interrogation of the IVC—no change in diameter between inspiration and expiration. AO: Ascending Aorta; DA: Descending thoracic aorta; Hv: Hepatic vein; LA: Left atrium; LV: Left ventricle; Liv: Liver; PE: Pericardial effusion; RA: Right atrium; RV: Right ventricle; RVOT: Right ventricular outflow tract; Insp: Inspiration; Exp: Expiration (Images courtesy of Aranya Bagchi, MBBS).

Full access? Get Clinical Tree







