CHAPTER 31
Urinary Tract Infections
Levita K. Hidayat, PharmD • Veena Venugopalan, PharmD, BCPS-AQID
Urinary tract infection (UTI) is the most common bacterial infection encountered in the ambulatory care setting in the United States, accounting for 8.6 million visits (84% by women) in 2007 (Schappert & Rechtsteiner, 2011). Infections of the urinary tract represent a wide variety of syndromes and may range in severity from urethritis, cystitis, and prostatitis to pyelonephritis. A UTI is defined as the presence of microorganisms in the urinary tract that cannot be accounted for by contamination. The organisms present have the potential to invade the tissues of the urinary tract and adjacent structures (Dipiro et al., 2012). Both men and women experience UTIs, although the incidence in females far exceeds that in males. Approximately 60% of females will develop a UTI during their lifetime, with about one-fourth having a recurrence within a year (Naber, Cho, Matsumoto, & Schaeffer, 2009). Infections in men occur much less frequently until the age of 65 years, at which point the incidence rates in men and women are similar (Dipiro et al., 2012).
Infection may involve either only the lower urinary tract or both the upper and lower tracts. For example, cystitis and urethritis are considered lower-tract infections, involving the bladder and urethra, respectively. In contrast, pyelonephritis is considered an upper-tract infection because it involves inflammation of the renal pelvis or parenchyma.
UTIs are further classified as uncomplicated and complicated. Uncomplicated refers to an infection in an otherwise healthy female who lacks structural or functional abnormalities of the urinary tract that interfere with the normal flow of urine or voiding mechanism. These infections occur in females of childbearing age (15–45 years) who are otherwise normal, healthy individuals. The estimated incidence in postmenopausal women (55–75 years) was much lower when compared to females of childbearing age (Jackson et al., 2004). Infections in males generally are not classified as uncomplicated because these infections are rare and most often represent a structural or neurologic abnormality (Dipiro et al., 2012).
Complicated UTIs are the results of structural or functional abnormalities of the genitourinary tract or underlying diseases that interfere with host defense mechanisms. Some predisposing factors that can lead to complicated UTIs include a congenital abnormality or distortion of the urinary tract, a stone, indwelling catheter, prostatic hypertrophy, obstruction, or neurologic deficit that interferes with the normal flow of urine and urinary tract defenses.
 ANATOMY, PHYSIOLOGY, AND PATHOLOGY
ANATOMY, PHYSIOLOGY, AND PATHOLOGY
The urinary tract can be viewed as an anatomic unit united by a continuous column of urine extending from the urethra to the kidneys. Organisms typically gain entry into the urinary tract via three routes: the ascending, hematogenous (descending), and lymphatic pathways. The ascending route is the most common. The female urethra is commonly colonized by bacteria, which are believed to originate from the fecal flora. Anatomic differences in women that predispose them to UTIs include a shorter urethra, which also is in close proximity to the rectal area, making it more susceptible to fecal contamination. Other factors that promote urethral colonization in women can result from direct inoculation during sexual activity and the use of spermicides and diaphragms as methods of contraception (Hooton, 2012; Naber et al., 2009).
Urinary infection may be localized to the bladder, may involve the kidneys as well as the bladder, and, for men, may also be localized in the prostate. Once bacteria have reached the bladder, the organisms quickly multiply and can ascend the ureters to the kidneys. Escherichia coli is the predominant pathogen in uncomplicated UTI. However, the introduction of bacteria into the bladder does not inevitably lead to sustained and symptomatic infection. The interplay of host, pathogen, and environmental factors determines whether tissue invasion and symptomatic infection will ensue. For example, bacteria often enter the bladder after sexual intercourse, but normal voiding and innate host defense mechanisms in the bladder eliminate these organisms. However, any foreign body in the urinary tract, such as a urinary catheter or stone, may provide an inert surface for bacterial colonization. Abnormal micturition and/or significant residual urine volume promote true infection. In short, anything that increases the likelihood of bacteria entering and staying in the bladder increases the risk of infection (Dipiro et al., 2012; Longo et al., 2013).
The hematogenous route of bacterial entry involves bloodborne pathogens that infect renal parenchyma. However, hematogenous spread accounts for <2% of documented UTIs, and usually results from bacteremia caused by relatively virulent organisms, such as Salmonella and S. aureus (Dipiro et al., 2012; Longo et al., 2013). Additional organisms include Candida spp., Mycobacterium tuberculosis, and enterococci. Overall, <5% of documented UTIs result from hematogenous spread of microorganisms. There are lymphatic communications between the bowel and kidney, as well as between the bladder and kidney. There is no evidence, however, that microorganisms are transferred to the kidney via this route.
In summary, after organisms reach the urinary tract, three factors determine the development of infection: the size of the inoculum, the virulence of the microorganism, and the competency of the host’s natural defense mechanisms (Dipiro et al., 2012).
 EPIDEMIOLOGY
EPIDEMIOLOGY
UTI is the most common bacterial infection encountered in the ambulatory care setting in the United States, accounting for 8.6 million visits (84% by women) in 2007 (Hooton, 2012). The incidence of symptomatic UTI in young healthy adult men is much lower than that in women. Approximately 5 to 8 UTIs occur per year per 10,000 young- to middle-aged men (Krieger, Ross, & Simonsen, 1993). Among sexually active young women, the incidence of symptomatic UTI is high. In one university cohort of 796 women, the incidence was 0.5 to 0.7 UTIs per person-year (Hooton et al., 1996). A study in college women also noted 0.7 episodes of cystitis per person-year in women starting a new contraceptive method (Foxman et al., 2000). As shown in Table 31.1, among sexually active young women, the incidence of symptomatic UTI is high. Furthermore, the risk is strongly and independently associated with recent sexual intercourse, recent use of a diaphragm with spermicide, and a history of recurrent UTIs.
UTI Risk Factors |
 Extremes in age
Extremes in age
 History of recent UTI
History of recent UTI
 Neurologic dysfunction: spinal cord injury, stroke, atherosclerosis, diabetes mellitus
Neurologic dysfunction: spinal cord injury, stroke, atherosclerosis, diabetes mellitus
 Renal disease
Renal disease
 Sexual intercourse
Sexual intercourse
 Contraceptive methods (e.g., diaphragms, spermicides)
Contraceptive methods (e.g., diaphragms, spermicides)
 Urinary tract instrumentation (e.g., catheterization)
Urinary tract instrumentation (e.g., catheterization)
 Urinary tract obstruction
Urinary tract obstruction
 UTI
UTI
UTI, urinary tract infection.
Cystitis also occurs in postmenopausal women. In a population-based prospective cohort study of 1,017 postmenopausal women aged 55 to 75 years followed for 2 years, the estimated incidence of culture-confirmed acute cystitis was 0.07 episodes per person per year (Jackson et al., 2004). In contrast, acute uncomplicated pyelonephritis is less common than cystitis (estimated ratio, 1 case of pyelonephritis to 28 cases of cystitis), with a peak annual incidence of 25 cases per 10,000 women 15 to 34 years of age (Czaja, Scholes, Hooton, & Stamm, 2007; Ikäheimo et al., 1996). In adults aged 65 years and older, the incidence rate approaches 10% in women and, in men older than 80 years, 5.3% (Foxman & Brown, 2003).
 DIAGNOSTIC CRITERIA
DIAGNOSTIC CRITERIA
The definitive diagnosis of a UTI is the detection of the appropriate quantitative counts of uropathogen in the presence of clinical symptoms. The American College of Obstetricians and Gynecologists (ACOG) and The Society of Obstetricians and Gynaecologists of Canada (SOGC) have agreed that common signs and symptoms of acute uncomplicated lower UTI include dysuria, frequent and urgent urination, suprapubic pain or tenderness, and possibly hematuria (Epp et al., 2010). The probability of cystitis is >50% in women with any symptoms or UTI and >90% in women who have dysuria and frequency without vaginal discharge or irritation (Bent, Nallamothu, Simel, Fihn, & Saint, 2002). Additionally, the presence of vaginal symptoms (e.g., vaginitis, urethritis) should prompt a pelvic examination and/or alternative diagnoses.
Laboratory diagnostic tools consist of urinalysis (either by microscopy or by dipstick) and urine culture with susceptibility data. Urinalysis in the absence of urine culture is sufficient for diagnosis of uncomplicated cystitis if symptoms are consistent with UTI. However, if there is reason to suspect antimicrobial resistance or other complicating features, a urine specimen for culture is essential to confirm the diagnosis and determine antimicrobial susceptibilities of the infecting organism. This latter facilitates appropriate antimicrobial therapy. Additionally, urine culture and antimicrobial susceptibility testing of uropathogens should be performed in all women with acute pyelonephritis.
Most episodes of cystitis and pyelonephritis are generally considered to be uncomplicated in otherwise healthy nonpregnant adult women. A complicated UTI, whether localized to the lower or upper tract, is associated with an underlying condition that increases the risk of failing therapy. Such conditions include obstruction, anatomic abnormality, urologic dysfunction, and/or a multidrug-resistant uropathogen (Hooton et al., 2010). Differentiating between a lower-tract infection and an upper-tract infection may be difficult, however, based on symptoms alone. Some patients with upper-tract infections fail to present with the components of infections. Therefore, a urinalysis is important to identify any other components of infection (Hooton et al., 2010).
Microbiology
The microbial spectrum of uncomplicated cystitis and pyelonephritis consists mainly of E. coli (75–95%), with occasional other species of Enterobacteriaceae, such as Proteus mirabilis and Klebsiella pneumoniae, and Staphylococcus saprophyticus. Other gram-negative and gram-positive species are rarely isolated in uncomplicated UTIs. The resistance patterns of E. coli strains causing uncomplicated UTI vary considerably between regions and countries; therefore, a specific treatment recommendation may not be universally suitably for all regions or countries. Thus, antimicrobial susceptibility patterns of E. coli should be considered in empiric antimicrobial selection for uncomplicated UTIs (DiPiro et al., 2012).
Gram-negative rods are the most common etiologic agent, with E. coli causing approximately 58% to 88% of infections in women versus 75% to 80% of episodes in men with acute versus chronic prostatitis (Cornia, Takahashi, & Lipsky, 2006; Schaeffer, 2006). Enterococcus faecalis, Klebsiella pneumoniae, P. mirabilis, Pseudomonas aeruginosa, and other gram-negative bacilli are the next most commonly reported organisms (Lipsky, Byren, & Hoey, 2010; Naber, Busch, & Focht, 2000).
A single organism usually causes bacteriuria in patients having short-term catheters (Krieger, Kaiser, & Wenzel, 1983; Hooton et al., 2010). E. coli is the species most frequently isolated, although it comprises less than one third of isolates (Nicolle, 2005). Other Enterobacteriaceae, such as Klebsiella species, Serratia species, Citrobacter species, and Enterobacter species; nonfermenters such as P. aeruginosa; and gram-positive cocci, including coagulase-negative staphylococci and Enterococcus species, are also isolated (Nicolle, 2005). Funguria, mostly candiduria, is reported in 3% to 32% of patients catheterized for short periods of time (Hooton et al., 2010; Nicolle, 2005). In contrast to patients with short-term catheterization, UTIs in patients with long-term catheterization are usually polymicrobial (Hooton et al., 2010).
 HISTORY AND PHYSICAL EXAMINATION
HISTORY AND PHYSICAL EXAMINATION
Specific signs and symptoms were mentioned earlier.
Diagnostic Studies
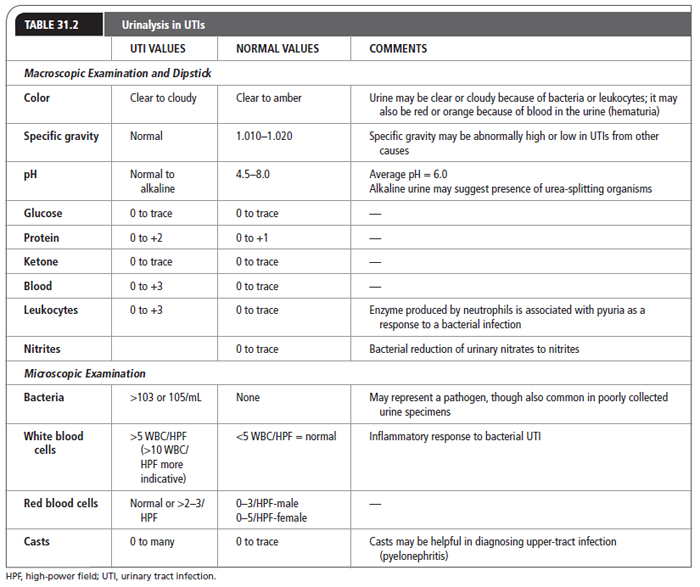
Among patients with clinical symptoms suggestive of a UTI, the diagnosis can be confirmed by sending a clean-catch specimen for urinalysis and culture. Urinalysis is invaluable in the diagnosis of urologic conditions such as calculi, UTI, and malignancy (Simerville, Maxted, & Pahira, 2005). A urinalysis to look for pyuria and hematuria is indicated if UTI is suspected. It includes both macroscopic and microscopic analysis and is done by the dipstick method. These include measuring or analyzing the urine for color, specific gravity, pH, glucose, protein, ketone, blood, and bilirubin (Table 31.2). Pyuria is present in almost all women with acutely symptomatic UTI and in most women with urethritis caused by Neisseria gonorrhoeae or Chlamydia trachomatis. The absence of pyuria strongly suggests an alternative diagnosis. Microscopic examination is an indispensable part of urinalysis; the identification of casts, cells, crystals, and bacteria aid in the diagnosis of a variety of conditions. To prepare a urine specimen for microscopic analysis, a fresh sample of 10 to 15 mL of urine should be centrifuged at 1,500 to 3,000 rpm for 5 minutes (Simerville et al., 2005).
Commercially available dipsticks that test for both leukocyte esterase and nitrites are often utilized to assess for pyuria and bacteriuria. The dipstick nitrite test depends on the conversion of nitrate (from dietary metabolites) to nitrite by bacteria in the urine. As demonstrated in Table 31.2, normally no detectable nitrite is present. Leukocyte esterase detects the enzyme produced by neutrophils associated with pyuria as a response to bacterial infections. The dipstick test is most accurate for predicting UTI when the test shows positive results for the presence of either leukocyte esterase or nitrite, with a sensitivity of 75% and a specificity of 82% (Bent et al., 2002; Hooton, 2003). A meta-analysis of 70 publications concluded that urine dipstick test alone is useful to exclude the presence of infections when both nitrite and leukocyte esterase tests are negative (sensitivity: 68%–88%; Devillé et al., 2004). However, when history is strongly suggestive of UTI, negative dipstick results do not reliably rule out infection (Bent et al., 2002).
Suprapubic aspiration is the optimal method for obtaining a sterile urine specimen. This procedure avoids contamination of specimens with bacteria in the distal urethra. However, this method is rarely used because it is invasive and uncomfortable, while also requiring additional resources (Wilson & Gaido, 2004). Most urine specimens are obtained from adult patients via the clean-catch midstream technique. This technique is advantageous because it is not invasive or uncomfortable and it can be performed in almost any clinical setting with no risk of introducing bacteria into the bladder through catheterization, while also decreasing the risk of complications in collection. Colony counts from urine specimens collected by this method correlate reasonably well with those of specimens collected via suprapubic aspiration or straight catheterization (Barford, Anson, Hu, & Coates, 2008). Available evidence suggests that cleansing procedures prior to collection may not decrease urine contamination rates significantly and, therefore, may be unnecessary as a routine practice (Schneeberger et al., 2013). However, because urine is so easily contaminated with commensal flora, specimens for culture of bacterial urinary tract pathogens should be collected with attention to minimizing contamination from the perineal and superficial mucosal microbiota.
A urine culture is performed to confirm the presence of bacteriuria and the antimicrobial susceptibility of the infecting uropathogen. A quantitative count of ≥105 colony-forming units (CFU)/mL is considered indicative of a UTI. However, up to 50% of women will present with clinical symptoms of a UTI with lower counts (103 CFU/mL) (Nicolle, 2008). This test is indicated for all women with suspected pyelonephritis but is not necessary for the diagnosis of cystitis, given the reliability of the patient’s history in establishing the diagnosis and delayed availability of culture results (Bent et al., 2002; Hooton, 2003). Urine culture with three or more species of bacteria in a urine specimen usually indicates contamination at the time of collection and should not be interpreted (Baron et al., 2013). The indications for culture in young women include suspicion of a complicated infection, atypical symptoms, failure to respond to initial therapy, and recurrent symptoms <1 month after treatment of a previous UTI for which no culture was performed (Wilson & Gaido, 2004).
In summary, urinalysis in the absence of urine culture is sufficient for diagnosis of uncomplicated cystitis if symptoms are consistent with UTI, unless there is reason to suspect antimicrobial resistance or other complicating features. The standard definition of a positive urine culture is ≥105 CFU/mL together with pyuria (e.g., leukocyte count ≥105 WBC/mL). Normal values in a noninfected midstream, clean-catch sample are <105 CFU (primarily due to contaminating E. coli) and <10,000 leukocytes per mL of urine. Contamination in the absence of UTI is typically suggested by high CFU counts without significant leukocyturia in a patient with no urinary tract symptoms such as dysuria, frequency, or fever. Table 31.2 lists normal and abnormal levels for these components of the urinalysis (Cohen & Brown, 2003; LeBlond, Brown, & Degowin, 2012; Simerville et al., 2005).
 TREATMENT OPTIONS, EXPECTED OUTCOMES, AND COMPREHENSIVE MANAGEMENT
TREATMENT OPTIONS, EXPECTED OUTCOMES, AND COMPREHENSIVE MANAGEMENT
The goals of UTI treatments are to eradicate the invading organism(s), to prevent or to treat systemic consequences of infection, and to prevent the recurrence of infection (Dipiro et al., 2012). The management of a patient with a UTI includes evaluation, selection of an antimicrobial agent and duration of therapy, and follow-up evaluation (Table 31.3; Dipiro et al., 2012).
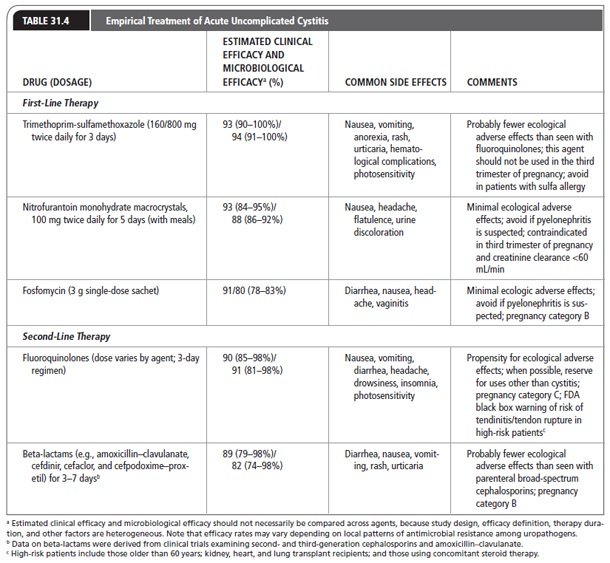
Table 31.4 presents considerations for selecting an agent for treatment of acute cystitis. These considerations include efficacy, pharmacokinetic/pharmacodynamic profile, side effects, resistance rates, propensity to cause ecological adverse effects of antimicrobial therapy (such as selection of drug-resistant organisms and development of colonization or infection with multidrug-resistant organisms), cost, and drug availability.
 PHARMACOLOGIC THERAPY
PHARMACOLOGIC THERAPY
The antimicrobial agent chosen for use should ideally have the following characteristics: well tolerated, well absorbed, achieves high urinary concentrations, and has a spectrum of activity limited to the known or suspected pathogen(s). Factors that affect the rate and extent of excretion through the kidney include the patient’s glomerular filtration rate (GFR) and whether or not the agent is actively secreted. As the GFR is reduced, the amount of drug that enters the urine is reduced (Dipiro et al., 2012).
UTI Management Considerations |
INITIAL EVALUATION OF PATIENTS |
Severity of illness (systemic sign and symptoms, complicated vs. uncomplicated infections) Site of infections (lower- vs. upper-tract infections) |
PATIENT-RELATED FACTORS |
Allergies Concomitant disease states Renal function or hepatic function |
PHARMACOLOGICAL FACTORS |
Antimicrobial concentration in urine Antimicrobial spectrum of activity Efficacy data Side effect profile Propensity to cause ecological adverse effectsa Dosing frequency Drug availability Cost |
aThe recently updated Infectious Diseases Society of America guidelines emphasize the importance of considering ecologic adverse effects of antimicrobial agents (i.e., selection for colonization or infection with multidrug-resistant organisms) when selecting a treatment regimen. UTI, urinary tract infection.
The traditional first-line agent in the United States and recommended in the original Infectious Disease Society of America (IDSA) guidelines (Warren et al., 1999) was trimethoprim-sulfamethoxazole (TMP-SMX). However, rising rates of resistance among uropathogens, especially outside of the United States, and consistent evidence that in vitro resistance correlates with bacterial and clinical failures, necessitates revision of this recommendation. Four randomized clinical trials compared TMP-SMX with other agents, including ciprofloxacin, norfloxacin, nitrofurantoin, and cefpodoxime–proxetil, and evaluated microbiological and clinical outcomes among women with acute cystitis (Arredondo-García et al., 2004; Gupta, Hooton, Roberts, & Stamm, 2007; Iravani et al., 1999; Kavatha et al., 2003). Overall findings from these studies demonstrate that TMP-SMX remains a highly effective treatment for acute uncomplicated cystitis in women when the rate of resistance is known or expected to be <20%, supporting a strong recommendation for use in such settings. Table 31.4 lists common side effects and precautions for TMP-SMX (Hooton, 2012).
Nitrofurantoin is another highly effective agent against most strains of E. coli and organisms previously sensitive to this agent. Such organisms rarely develop resistance. However, other organisms that may be associated with the development of UTIs, such as Proteus spp. and Klebsiella spp, are generally resistant to nitrofurantoin. As seen in Table 31.4, this drug is contraindicated in patients with anuria, oliguria, or renal impairment (estimated creatinine clearance <60 mL/min) because of possible toxicity resulting from impaired excretion. Four randomized trials of nitrofurantoin demonstrated a clinical cure rate of 88% to 93% and a bacterial cure rate of 81% to 92% when compared with a different antibacterial agent (Christiaens et al., 2002; Gupta et al., 2007; Iravani et al., 1999; Stein, 1999). These studies demonstrate that nitrofurantoin monohydrate/macrocrystals (100 mg twice daily for 7 days) has clinical cure rate similar to that of ciprofloxacin (100 mg twice daily for 3 days; 93% vs. 95%), TMP-SMX (160/800 mg twice daily for 7 days; 93% vs. 95%), and 3-g single-dose fosfomycin (Manurol) (89% vs. 90%) (Christiaens et al., 2002; Iravani et al., 1999; Stein, 1999). A 5-day regimen, rather than the traditional 7-day course, can be considered an effective duration of treatment based on a recent randomized clinical trial (Gupta et al., 2007). In summary, current randomized clinical trial data provide strong support for consideration of nitrofurantoin as an effective agent for treatment of acute cystitis. Demonstration of efficacy, with minimal drug resistance or propensity for collateral damage, makes nitrofurantoin an attractive agent for cystitis.
Fosfomycin tromethamine (Manurol), a phosphonic acid derivative, is available only in the oral form in the United States. This agent is approved as a one-dose antibiotic for the treatment of uncomplicated UTI, such as acute cystitis. A 3-g single dose of fosfomycin was compared with a 7-day course of nitrofurantoin monohydrate/macrocrystals 100 mg twice daily in one study and with a 5-day course of trimethoprim 100 mg twice daily in another (Minassian et al., 1998; Stein, 1999). The study by Stein was a Phase III multicenter (26 centers in the United States), double-blind randomized trial of fosfomycin 3 g orally given once, compared with nitrofurantoin 100 mg orally prescribed twice daily for 7 days. The early clinical responses to these medications (cure or improvement at 5–11 days after starting therapy) were not significantly different, at 91% (240/263) versus 95% (232/245) for fosfomycin and nitrofurantoin, respectively. However, the microbiologic cure rate was significantly higher with nitrofurantoin (86%), compared with fosfomycin (78%), at the first follow-up visit (p = .02). Microbiologic cure rates 4 to 6 weeks after therapy were 96% for fosfomycin and 91% for nitrofurantoin, but included only approximately 50% of the original study sample. The latter study only evaluated the microbiologic outcome and reported that single-dose fosfomycin and 5 days of twice-daily trimethoprim each had an 83% bacterial cure rate (147/177 fosfomycin and 70/84 trimethoprim-treated women, respectively) at the early follow-up visit (Minassian et al., 1998). Overall, the bacterial efficacy of fosfomycin is lower than that of other first-line agents, but clinical efficacy (based on a single study) was comparable (see Table 31.4). Of importance, several in vitro studies noted the activity of fosfomycin against multidrug-resistant pathogens, including vancomycin-resistant Enterococci (VRE), methicillin-resistant S. aureus (MRSA), and extended-spectrum beta-lactamase (ESBL)–producing gram-negative rods (Popovic, Steinort, Pillai, & Joukhadar, 2010). However, clinical results have not been reported from randomized, controlled studies. That is, only observational studies support clinical efficacy (Popovic et al., 2010; Rodríguez-Baño et al., 2008). Fosfomycin is unique in its mechanism of action and less likely to select for coresistance. Thus, this antibiotic may have a place in the treatment of both simple cystitis and more complicated UTI, although the literature on the latter is scant.

Full access? Get Clinical Tree