Ultrasound-Guided Popliteal and Lateral Sciatic Block
Steven L. Orebaugh
Vihang D. Shah
Paul E. Bigeleisen
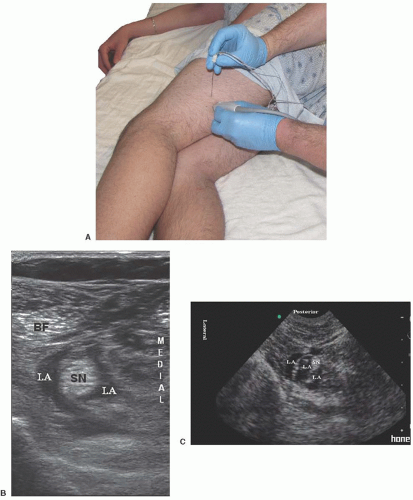
 Background and indications: Block of the sciatic nerve at the popliteal fossa is the most distal of the many approaches to the sciatic nerve. When ultrasound is used for imaging, local anesthetic is readily deposited around the sciatic nerve or around the tibial and common peroneal nerves when the block is done distal to the bifurcation of the sciatic nerve. Historically, the block was done with the patient prone (posterior approach). With the advent of ultrasound, the patient is usually placed in the lateral decubitus position with the operative side up or in the supine position.
Background and indications: Block of the sciatic nerve at the popliteal fossa is the most distal of the many approaches to the sciatic nerve. When ultrasound is used for imaging, local anesthetic is readily deposited around the sciatic nerve or around the tibial and common peroneal nerves when the block is done distal to the bifurcation of the sciatic nerve. Historically, the block was done with the patient prone (posterior approach). With the advent of ultrasound, the patient is usually placed in the lateral decubitus position with the operative side up or in the supine position.Block of the sciatic nerve at the popliteal fossa is indicated for surgical procedures involving the toes, foot, or subtalar joint. It may not be suitable as a primary anesthetic for major ankle procedures because surgeons often choose a thigh (rather than calf) tourniquet for control of bleeding during the procedure.
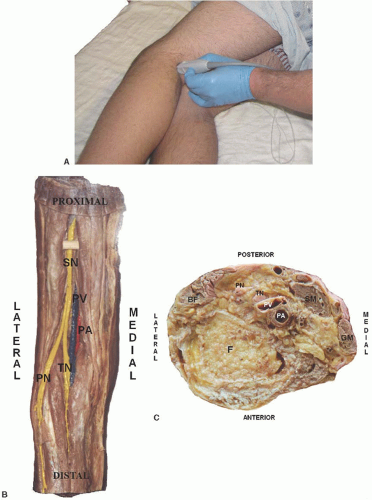
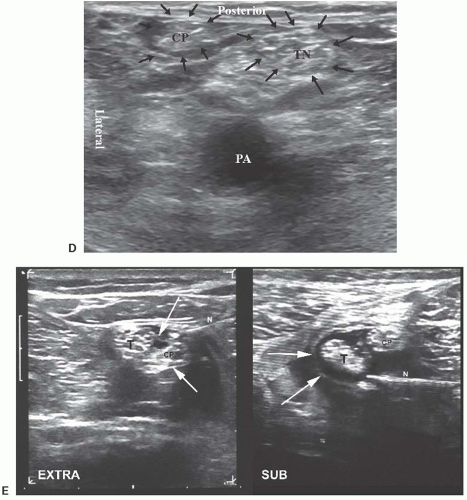
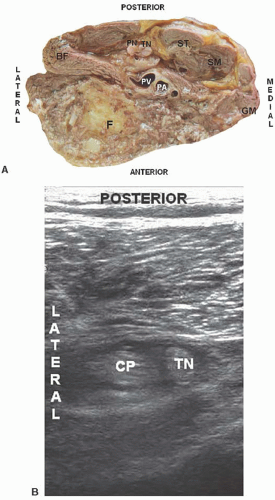
 Anatomy: It is useful to identify the arteries and veins in the area because of their position relative to the nerve. In the popliteal region, the popliteal artery and vein can be located at the flexor crease (Fig. 32.1). The tibial nerve is usually visible at this level, just lateral and/or superficial to the vein. Lateral to the nerve lies the biceps femoris muscle. Medial to the nerve lie the semimembranosus and semitendinosis muscles (Fig. 32.1). Once the tibial nerve is identified at the flexor crease, the probe can be moved slowly proximally, keeping the nerve in the center of the image. The tibial nerve is joined by the common peroneal nerve as the hamstring muscle bellies in the surrounding area enlarge and more subcuTaneous adipose tissue becomes evident (Fig. 32.2). Between 5 and 10 cm above the flexor crease, the smaller peroneal nerve will be seen lateral to the tibial nerve; above this level, a single rounded nerve structure is apparent (Fig. 32.3), which represents the conjoined tibial and peroneal nerves. The peroneal nerve is frequently more difficult to locate than the tibial because it is smaller and often appears to be made up of one or more large fascicles with little surrounding connective tissue.
Anatomy: It is useful to identify the arteries and veins in the area because of their position relative to the nerve. In the popliteal region, the popliteal artery and vein can be located at the flexor crease (Fig. 32.1). The tibial nerve is usually visible at this level, just lateral and/or superficial to the vein. Lateral to the nerve lies the biceps femoris muscle. Medial to the nerve lie the semimembranosus and semitendinosis muscles (Fig. 32.1). Once the tibial nerve is identified at the flexor crease, the probe can be moved slowly proximally, keeping the nerve in the center of the image. The tibial nerve is joined by the common peroneal nerve as the hamstring muscle bellies in the surrounding area enlarge and more subcuTaneous adipose tissue becomes evident (Fig. 32.2). Between 5 and 10 cm above the flexor crease, the smaller peroneal nerve will be seen lateral to the tibial nerve; above this level, a single rounded nerve structure is apparent (Fig. 32.3), which represents the conjoined tibial and peroneal nerves. The peroneal nerve is frequently more difficult to locate than the tibial because it is smaller and often appears to be made up of one or more large fascicles with little surrounding connective tissue.When imaging the level at which the sciatic nerve bifurcates, the popliteal vessels are usually considerably deeper than the nerve (Fig. 32.2). Because significant pressure is often required to optimize the nerve image, it is imporTant to periodically decrease the pressure applied with the transducer; this will help reveal the popliteal vein, which otherwise may remain compressed and invisible. Deep to the vessels, the hyperechoic, arcuate form of the cortex of the femur is evident.
At this level, the sciatic nerve is encased by a thick mesoneurial sheath. Within the nerve, both the peroneal and tibial nerves are encased by their proper epineurium. Within the epineurium of each nerve lie the fascicles, each of which is bounded by perineurium. Currently, the term used to describe the fascial sheath of the sciatic nerve, which surrounds both components (tibial and common peroneal nerve), is a topic of contention. Authors have referred to this anatomic structure as a paraneural sheath1 or complex fascial layer,2,3 whereas others termed it a common epineural sheath4 (Fig. 32.1E). The authors’ preference is to call this the mesoneurium. Deposition of local anesthetic within the paraneural sheath at the level of the nerve bifurcation, but outside the epineurium of the tibial and peroneal nerves, may afford some advantages in the block.5
 Patient position/transducer: Patients should be positioned in the lateral decubitus position with the operative side up. A linear 5- to 10-MHz transducer is ideal for this application. Only for the heaviest patients would a lower frequency, curvilinear transducer be necessary. For small or thin subjects, a higher frequency linear transducer, such as 10 to 13 MHz, will provide excellent images. The transducer is held in the transverse position, directly over the flexor crease, and is moved proximally (Fig. 32.3). Very commonly, the image is optimized with a significant degree of caudad tilt of the transducer. For the supine approach, a 40- to 60-mm curved array oscillating at 3 to 5 MHz is required. For thin patients, a small curved array oscillating at 6 to 10 MHz will suffice.
Patient position/transducer: Patients should be positioned in the lateral decubitus position with the operative side up. A linear 5- to 10-MHz transducer is ideal for this application. Only for the heaviest patients would a lower frequency, curvilinear transducer be necessary. For small or thin subjects, a higher frequency linear transducer, such as 10 to 13 MHz, will provide excellent images. The transducer is held in the transverse position, directly over the flexor crease, and is moved proximally (Fig. 32.3). Very commonly, the image is optimized with a significant degree of caudad tilt of the transducer. For the supine approach, a 40- to 60-mm curved array oscillating at 3 to 5 MHz is required. For thin patients, a small curved array oscillating at 6 to 10 MHz will suffice.
Full access? Get Clinical Tree