Ultrasound-Guided Interscalene Brachial Plexus Block

FIGURE 29-1. Ultrasound-guided interscalene brachial plexus block; transducer and needle position to obtain the desired ultrasound image for an in-plane approach.
General Considerations
The ultrasound-guided technique of interscalene brachial plexus block differs from nerve stimulator or landmark-based techniques in several important aspects. Most importantly, distribution of the local anesthetic is visualized to assure adequate spread around the brachial plexus. Ultrasound guidance allows multiple injections around the brachial plexus, therefore eliminating the reliance on a single large injection of local anesthetic for block success as is the case with non–ultrasound-guided techniques. Ability to inject multiple aliquots of local anesthetic also may allow for the reduction in the volume of local anesthetic required to accomplish the block. Repetition of the block in case of inadequate anesthesia is also possible, a management option that is unpredictable without ultrasound guidance. Finally, the risk of major vessel and nerve puncture during nerve block performance is reduced.
Ultrasound Anatomy
The brachial plexus at the interscalene level is seen lateral to the carotid artery, between the anterior and middle scalene muscles (Figures 29-2, 29-3, and 29-4). Prevertebral fascia, superficial cervical plexus and sternocleidomastoid muscle are seen superficial to the plexus. The transducer is moved in the superior-inferior direction until two or more of the brachial plexus trunks are seen in the space between the scalene muscles. Depending on the depth of field selected and the level at which the scanning is performed, first rib and/or apex of the lung may be seen. The brachial plexus is typically visualized at a depth of 1 to 3 cm.
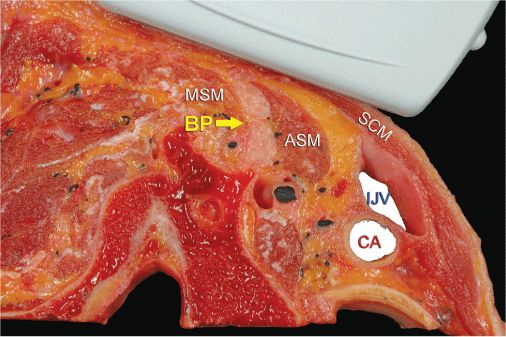
FIGURE 29-2. Relevant anatomy for interscalene brachial block and transducer position to obtain the desired views. Brachial plexus (BP) is seen sandwiched between middle scalene muscle (MSM) laterally and anterior scalene muscle (ASM) medially. Ultrasound image often includes a partial view of the lateral border of the sternocleidomastoid muscle (SCM) as well as the internal jugular vein (IJV) and carotid artery (CA). The transverse process of one of the cervical vertebrae is also often seen.
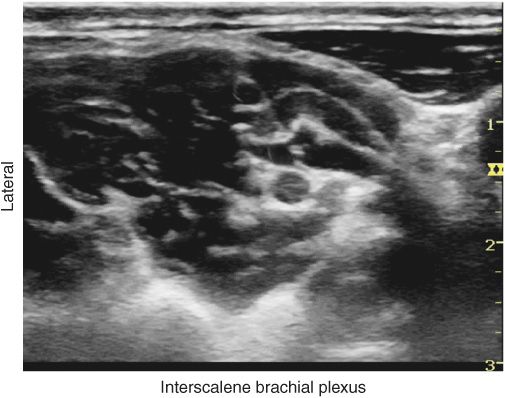
FIGURE 29-3. Interscalene brachial plexus is seen between middle scalene muscle and anterior scalene muscle. Carotid artery is seen medial at 1 cm depth in this image.
FIGURE 29-4. Typical image of the brachial plexus (BP). The BP is seen positioned between the anterior scalene muscle (ASM) and the middle scalene muscle (MSM). The superficial cervical plexus (white arrowhead) can be seen posterior to the SCM and underneath the prevertebral fascia. In this particular image, the vertebral artery (VA), carotid artery (CA), as well as the transverse process of C6 are also seen.
Distribution of Blockade
The interscalene approach to brachial plexus blockade results in anesthesia of the shoulder and upper arm. Inferior trunk for more distal anesthesia can also be blocked by additional, selective injection, deeper in the plexus. This is accomplished either by controlled needle redirection inferiorly or by additional scanning to visualize the inferior trunk and another needle insertion and targeted injection. For a more comprehensive review of the brachial plexus distribution, see Chapter 1 on Essential Regional Anesthesia Anatomy.
Equipment
Equipment needed includes the following:
• Ultrasound machine with linear transducer (8–14 MHz), sterile sleeve, and gel
• Standard nerve block tray (described in the equipment section)
• One 20-mL syringe containing local anesthetic
• 5-cm, 22-gauge short-bevel insulated stimulating needle
• Peripheral nerve stimulator
• Sterile gloves
Landmarks and Patient Positioning
Any position that allows comfortable placement of the ultrasound transducer and needle advancement is appropriate. The block is typically performed with the patient in supine, semisitting, or semilateral decubitus position, with the patient’s head facing away from the side to be blocked. The latter position may prove ergonomically more convenient, especially during an in-plane approach from the lateral side, in which the needle is entering the skin at the posterolateral aspect of the neck. A slight elevation of the head of the bed is often more comfortable for the patient, and it allows for better drainage and less prominence of the neck veins.
Adherence to strict anatomic landmarks is of lesser importance for the ultrasound-guided interscalene block than it is the case for the surface anatomy-based techniques. Regardless, knowledge of the underlying anatomy and the position of the brachial plexus is important to facilitate recognition of the ultrasound anatomy. Scanning usually begins just below the level of the cricoid cartilage and medial to the sternocleidomastoid muscle with a goal to identify the carotid artery.
Technique
With the patient in the proper position, the skin is disinfected and the transducer is positioned in the transverse plane to identify the carotid artery (Figure 29-5). Once the artery is identified, the transducer is moved slightly laterally across the neck (see algorithm at end of chapter). The goal is to identify the scalene muscles and the brachial plexus that is sandwiched between the anterior and middle scalene muscles.
FIGURE 29-5. Ultrasound image just below the level of the cricoid cartilage and medial to the sternocleidomastoid muscle. ASM, anterior scalene muscle; SCM, sternocleidomastoid muscle; IJV, internal jugular vein; CA, carotid artery; Th, thyroid gland.

Full access? Get Clinical Tree








