Ultrasound-Guided Infraclavicular Brachial Plexus Block

FIGURE 31-1. In-plane needle insertion technique during infraclavicular brachial plexus block.
General Considerations
The ultrasound-guided infraclavicular brachial plexus block is in some ways both simple and challenging. It is simple in the sense that geometric measuring of distances and angles on the surface of the patient, as is the case with the nerve stimulator–based technique, is not required. Identification of the arterial pulse on the sonographic image is an easy primary goal in establishing the landmark. However, the plexus at this level is situated deeper, and the angle of approach is more acute, making simultaneous visualization of the needle and the relevant anatomy more challenging. Fortunately, although it is not always possible to reliably identify the three cords of the plexus at this position, adequate block can be achieved by simply depositing the local anesthetic in a “U” shape around the artery. Infraclavicular block is well-suited for catheter technique because the musculature of the chest wall helps stabilize the catheter and prevents its dislodgment compared with the more superficial location with the interscalene or supraclavicular approaches.
Ultrasound Anatomy
The axillary artery can be identified deep to the pectoralis major and minor muscles. An effort needs to be made to obtain clear views of both pectoralis muscles and their respective fasciae. This is important because the area of interest lies underneath the fascia of the pectoralis minor muscle. Surrounding the artery are the three cords of the brachial plexus: the lateral, posterior, and medial cords. These are named for their usual position relative to the axillary artery, although there is a great deal of anatomic variation. With the left side of the screen corresponding to the cephalad aspect, the cords can often be seen as round hyperechoic structures at approximately 9 o’clock (lateral cord), 7 o’clock (posterior cord), and 5 o’clock (medial cord) (Figures 31-2, 31-3, and 31-4). The axillary vein is seen as a compressible hypoechoic structure that lies inferior, or slightly superficial, to the axillary artery. Multiple other, smaller vessels (e.g., the cephalic vein) are often present as well. The transducer is moved in the superior-inferior direction until the artery is identified in cross-section. Depending on the depth of field selected and the level at which the scanning is performed, the chest wall and lung may be seen in the inferior aspect of the image. The axillary artery and/or brachial plexus are typically identified at a depth of 3 to 5 cm in average size patients.
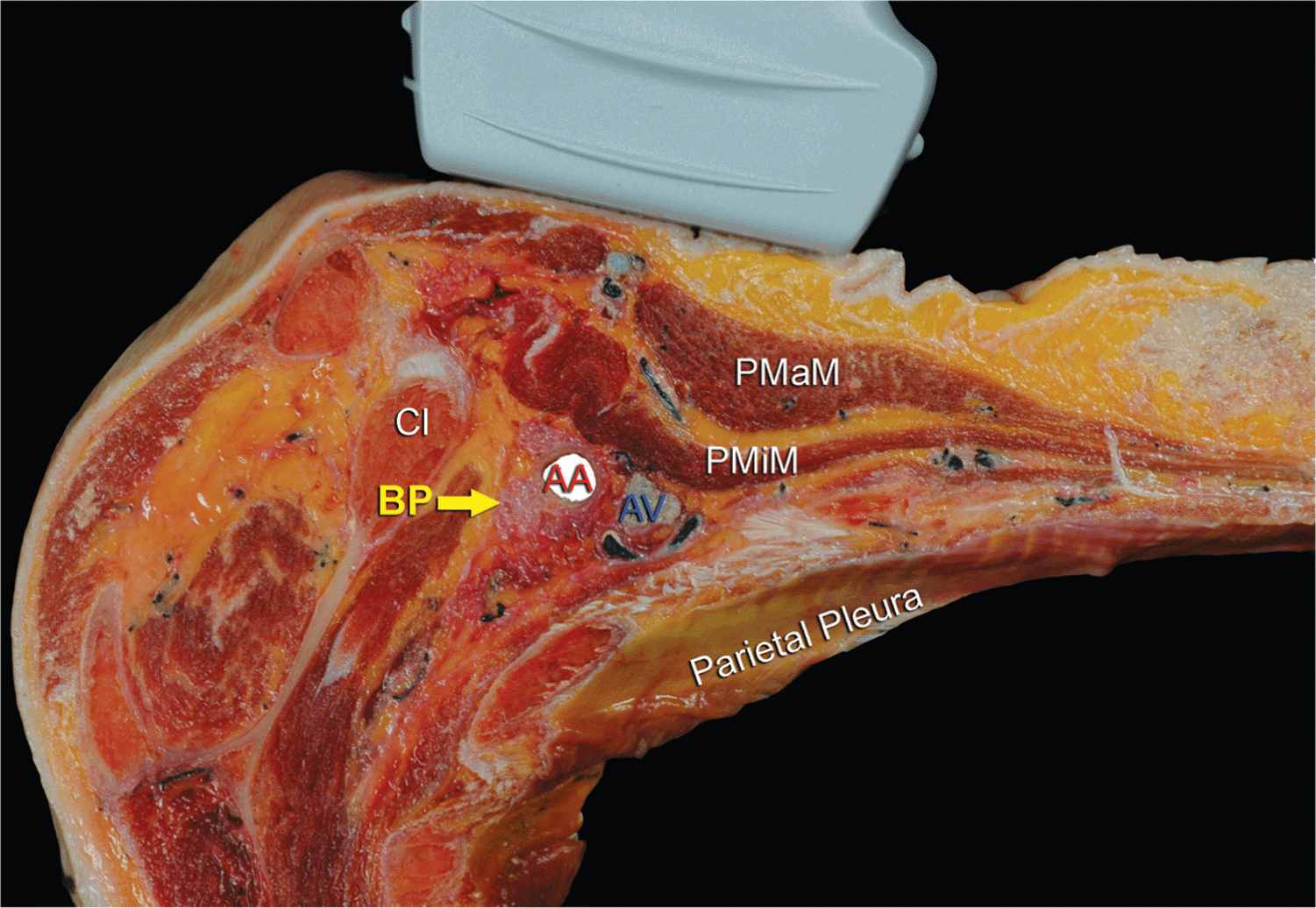
FIGURE 31-2. Anatomy of the infraclavicular brachial plexus and the position of the transducer. Brachial plexus (BP) is seen surrounding the axillary artery (AA) underneath the clavicle (Cl) and pectoralis minor muscle (PMiM). Note that the injection of local anesthetic should take place below the fascia of the PMiM to spread around the AA. PMaM, pectoralis major muscle.
FIGURE 31-3. Unlabeled ultrasound image of the infraclavicular fossa demonstrating pectoralis muscles, their respective sheets, axillary (subclavian) vessels, and the chest wall.
FIGURE 31-4. Labeled ultrasound image of the brachial plexus (BP) in the infraclavicular fossa. LC, lateral cord; PC, posterior cord; MC, medial cord. Note that the brachial plexus and the axillary artery (AA) are located below the fascia (red line) of the pectoralis minor muscle (PMiM). PMaM, pectoralis major muscle.
Distribution of Blockade
The infraclavicular approach to brachial plexus blockade results in anesthesia of the upper limb below the shoulder. The medial skin of the upper arm (intercostobrachial nerve, T2), if required, can be blocked by an additional subcutaneous injection on the medial aspect of the arm just distal to the axilla. A simpler approach is for surgeons to infiltrate the skin with the local anesthetic directly over the incision line, if necessary. For a more comprehensive review of the brachial plexus distribution, see Chapter 1, Essential Regional Anesthesia Anatomy.
Equipment
Equipment needed for this block includes the following:
• Ultrasound machine with linear transducer (8–14 MHz), sterile sleeve, and gel
• Standard nerve block tray
• 20 to 30 mL of local anesthetic drawn up in syringes
• 8- to 10-cm long, 21-22 gauge short-bevel insulated stimulating needle
• Peripheral nerve stimulator
• Sterile gloves
Landmarks and Patient Positioning
Any position that allows comfortable placement of the ultrasound transducer and needle advancement is appropriate. The block is typically performed with the patient in supine position with the head turned away from the side to be blocked (Figure 31-5). The arm is abducted to 90° and the elbow flexed. This maneuver reduces the depth from the skin to the plexus and substantially facilitates visualization of the pectoralis muscles as well as the cords of the brachial plexus.

FIGURE 31-5. Patient position in needle insertion for infraclavicular brachial plexus block. The transducer is positioned parasagittally just medial to the coracoid process and inferior to the clavicle.
The coracoid process is an important landmark and can be easily identified by palpating the bony prominence just medial to the shoulder while the arm is elevated and lowered. As the arm is lowered, the coracoid process meets the fingers of the palpating hand. Scanning is usually begun just medial to the coracoid process and inferior to the clavicle. As scanning experience increases, it eventually becomes unnecessary to identify the coracoids process before scanning.
Technique
With the patient in the proper position, the skin is disinfected and the transducer is positioned in the parasagittal plane to identify the axillary artery (Figures 31-3 and 31-4, and 31-5). This may require adjustment of the depth, depending on the thickness of the patient’s chest wall musculature. The axillary artery (or the transition of the subclavian to axillary artery) is typically seen between 3 and 5 cm. Once the artery is identified, an attempt is made to identify the hyperechoic cords of the brachial plexus and their corresponding positions relative to the artery, although these may not always be identifiable. Fortunately, exhaustive efforts to visualize the cords are not necessary for successful blockade.
The needle is inserted in-plane from the cephalad aspect, with the insertion point just inferior to the clavicle (Figure 31-5). The needle is aimed toward the posterior aspect of the axillary artery and passes through the pectoralis major and minor muscles. If nerve stimulation is used concurrently (0.5-0.8 mA, 0.1 msec), the first motor response is often from the lateral cord (either elbow flexion or finger flexion). As the needle is further advanced beneath the artery, a posterior cord motor response may appear (finger and wrist extension). After careful aspiration, 1 to 2 mL of local anesthetic is injected to confirm the proper needle placement and spread. The injectate should spread cephalad and caudad to cover the lateral and medial cords, respectively (Figure 31-6). When injection of the local anesthetic with a single injection does not appear to result in adequate spread, additional needle repositions and injections around the axillary artery may be necessary (Figure 31-7).
FIGURE 31-6. Ultrasound image demonstrating an ideal needle path for the infraclavicular brachial plexus block. Blue-shaded area mimics an ideal spread of the local anesthetic around axillary artery (AA) and reaching all three cords of the brachial plexus (LC, PC, MC) below the fascia (red line) of the pectoralis minor muscle. PMaM, pectoralis major muscle; PMiM, pectoralis minor muscle.
FIGURE 31-7. An ultrasound image demonstrating an actual needle placement above (cephalad) the axillary artery (AA) and an injection of local anesthetic (2 mL; blue shadow) to document the proper needle tip placement. LC, lateral cord; MC, medial cord; PC, posterior cord.

Full access? Get Clinical Tree








