Sonoanatomy of the inguinal (femoral) region.
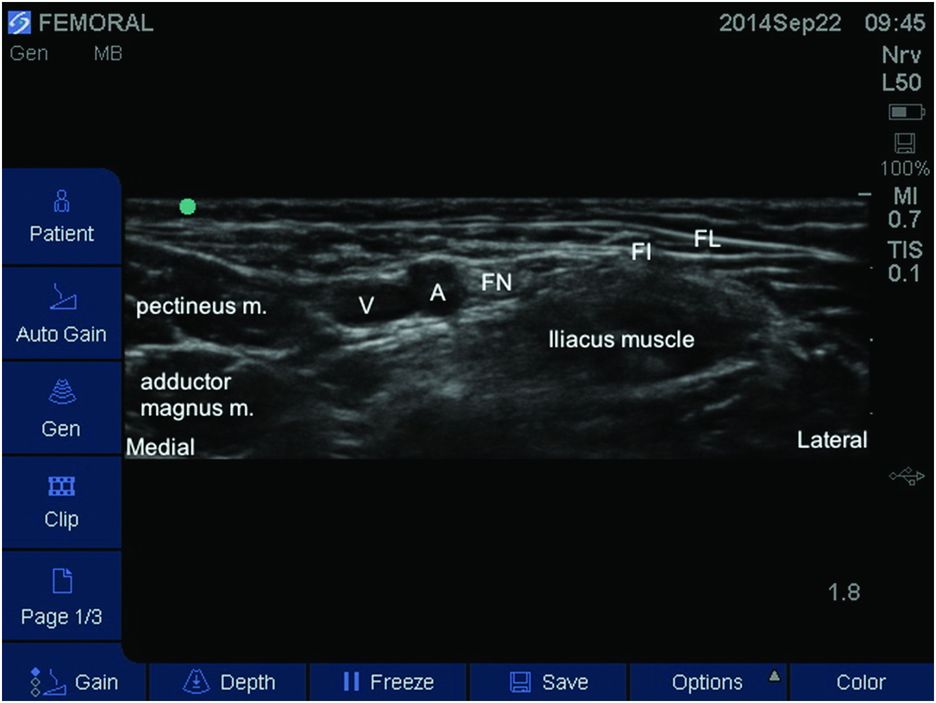
Sonoanatomy of the inguinal (femoral) region. The femoral nerve (FN) appears laterally to the femoral artery (A). Both fasciae (lata – FL and iliaca – FI) can be visualized. The femoral vein (V) is commonly visualized medially to both the femoral artery and nerve.
Landmarks
Depending on whether the anesthesiologist is right- or left-handed, the ultrasound machine is generally placed to the opposite side of the operator and the practitioner faces the screen. With the child usually in the supine position, the femoral region is best visualized when the lower limb is slightly abducted with external rotation. Under ultrasound guidance, a high-frequency linear array probe is positioned in the inguinal crease (parallel and just below the inguinal ligament) and placed perpendicular to the nerve axis (Figure 11.3). After a transverse back and forth scan (with gentle slide/tilt/rotation), the femoral nerve is easily located laterally to the femoral artery (the latter appearing as an anechoic circular non-compressive pulsatile structure; Doppler ultrasound might be helpful to identify the femoral artery for beginners). Ultrasound guidance may reduce the risk of femoral artery puncture compared with conventional techniques. The profunda femoris artery or the superficial iliac circumflex artery might be visualized if the probe is cranially or caudally applied to the femoral region. The femoral nerve appears as a rough triangle-shaped hyperechoic structure lying on the iliopsoas muscle sulcus at a 1–2 cm depth and covered by the fascia iliaca. With a certain expertise, the practitioner can locate the femoral nerve lying below both fascias lata and iliaca separately, encountered at this level as thin hyperechoic layers, and the easily collapsed femoral vein. (A gentle pressure exerted by the operator of the probe on the patent is highly recommended to prevent femoral vein collapse and may improve visualization.)
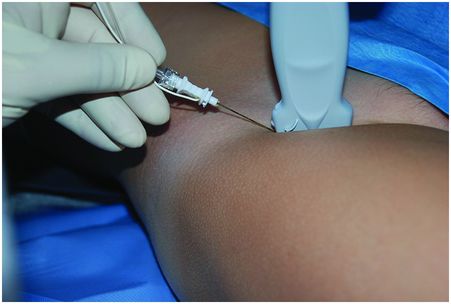
Probe placement and patient position.
The femoral nerve is usually greatly sensitive to anisotropy (i.e. change in ultrasound direction), and one must frequently adjust cranially and caudally the transducer to optimize correct visualization of the femoral region and accurately distinguish musculoskeletal and nerve structures. For coverage of the medial/lateral aspects of the lower limb and depending on surgical incision location, the practitioner should consider combining the FNB with either a lateral femoral cutaneous nerve block, sciatic nerve block, or obturator nerve block.
Block performance
Depending on body weight or anatomy of the child, a 25, 50, or 100-mm 22-gauge echoic needle is generally used, and a transducer probe with a small footprint habitually facilitates block performance in infants or toddlers.
After sterile preparation of the site, and most commonly under general anesthesia or local infiltration, the block needle is inserted and advanced under ultrasound guidance. After optimizing the femoral nerve view, the shaft needle is usually best visualized in the long axis (Figure 11.4).
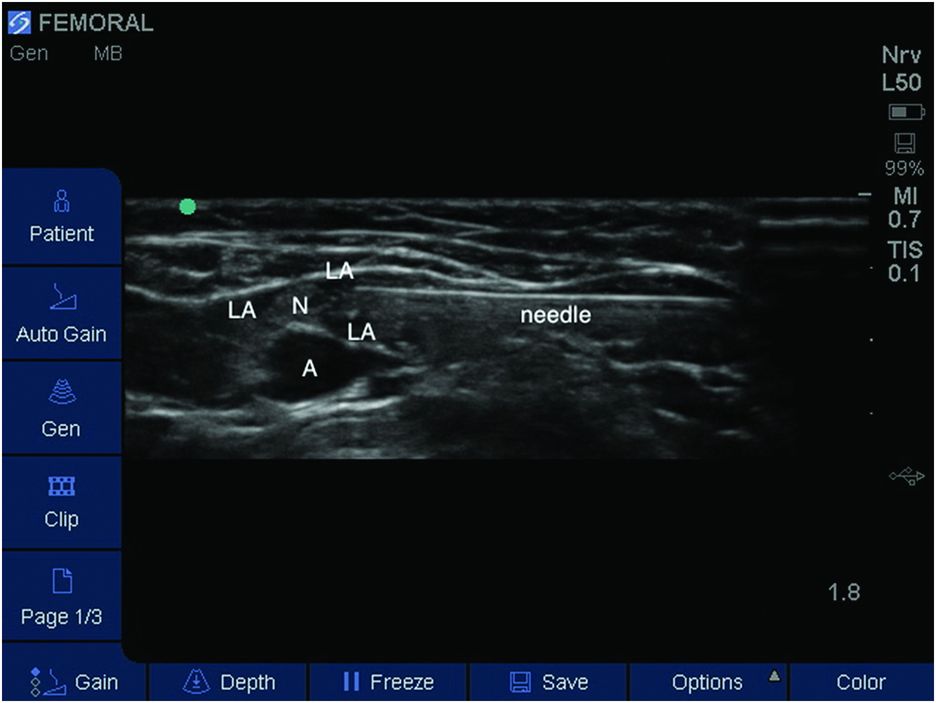
Transverse sonogram of the femoral region. In-plane needle technique. A, femoral artery; LA, local anesthetic; N, femoral nerve.
The needle tip is advanced in an “in-plane” manner towards the lateral side of the femoral nerve after penetrating both fascias and the LA is customarily deposited below and laterally to the femoral nerve after test aspiration. Studies evaluating LA spread are lacking in the pediatric population, i.e. above/below or circumferential of LA diffusion. The LA should be injected once the first layer of the fascia iliaca is penetrated, above the femoral branches division and adjacent to the posterolateral or anterior aspects of the femoral nerve. The deposited LA solution spreads as a hypoechoic collection while sheath distention is observed and femoral nerve echogenicity is increased. Some practitioners systematically scan the femoral region proximally and distally to assess the extent of the injectate. The injection of the solution must be executed without resistance; in that case, repositioning the needle tip is mandatory to prevent intrafascicular injection. The LA usually spreads superficially above the femoral nerve unless the needle tip is located in the wedge-shaped fascia iliaca.
The optimal volume of LA has not been evaluated for this block in children, but a volume of 0.2 ml/kg is recommended.
An out-of-plane technique has been described but has mostly not favored pediatric anesthesiologists, because tracking the needle tip can be challenging in that situation.
A South African study supports an ultrasound approach in comparison with nerve stimulator guidance in a study of 14 children (Oberndorfer et al., 2007). The use of ultrasound was associated with increased success rate and prolonged duration of sensory blockade with reduced amounts of LA (0.15 vs. 0.30 ml/kg of levobupivacaine 0.5%). In adults though, using that approach, more nerve needle contact might occur with potential adverse neurologic nerve events (Ruiz et al., 2014).
Finally, depending on surgical incision location, deliberate injection of additional volume may lead to lateral spread underneath the fascia iliaca and blockade of the lateral femoral cutaneous nerve (Flack et al., 2012). Miller has recently described a combined femoral nerve and lateral femoral cutaneous nerve blockade under ultrasound guidance using the same needle (Miller, 2011a). In brief, once the femoral nerve is blocked, the transducer is moved laterally along the inguinal ligament and the lateral femoral cutaneous nerve is identified between both fascia lata and iliaca layers above the sartorius muscle; 1–2 ml of LA solution is suffice to surround nerve branches.
Ultrasound-guided fascia iliaca block
In children, the femoral nerve can also be blocked using the ultrasound-guided fascia iliaca compartment block approach. An in-plane long-axis approach directed cephalad has been recently described for the first time by Miller in three children undergoing hip or femur surgery and appears a reliable and successful procedure for pain relief (Miller, 2011b). The needle tip was placed just below the fascia iliaca into the iliacus muscle. However, as a case report study, there has been no evaluation of the minimum volume of LA required. Rather, a 0.63–0.80 ml/kg ropivacaine 0.2% single shot has been injected in these cases. Further studies are required to clearly demonstrate efficacy in this promising technique.

Full access? Get Clinical Tree








