FIGURE 36-1. Needle insertion for the fascia iliaca block. The blue dot indicates the position of the femoral artery.
General Considerations
Fascia iliaca block is a low-tech alternative to a femoral nerve or a lumbar plexus block. The mechanism behind this block is that the femoral and lateral femoral cutaneous nerves lie under the iliacus fascia. Therefore, a sufficient volume of local anesthetic deposited beneath the fascia iliaca, even if placed some distance from the nerves, has the potential to spread underneath the fascia and reach these nerves. Traditionally, it was believed that the local anesthetic could also spread underneath fascia iliaca proximally toward the lumbosacral plexus; however, this has not been demonstrated consistently. The non-ultrasound technique involved placement of the needle at the lateral third of the distance from the anterior superior iliac spine and the pubic tubercle, using a “double-pop” technique as the needle passes through fascia lata and fascia iliaca. However, block success with this “feel” technique is sporadic because false “pops” can occur. The ultrasound-guided technique is essentially the same; however, monitoring of the needle placement and local anesthetic delivery assures deposition of the local anesthetic into the correct plane.
Ultrasound Anatomy
The fascia iliaca is located anterior to the iliacus muscle (on its surface) within the pelvis. It is bound superolaterally by the iliac crest and medially merges with the fascia overlying the psoas muscle. Both the femoral nerve and the lateral cutaneous nerve of the thigh lie under the iliacus fascia in their intrapelvic course. Anatomic orientation begins in the same manner as with the femoral block: with identification of the femoral artery at the level of the inguinal crease. If it is not immediately visible, sliding the transducer medially and laterally will eventually bring the vessel into view. Immediately lateral and deep to the femoral artery and vein is a large hypoechoic structure, the iliopsoas muscle (Figure 36-2). It is covered by a thin layer of connective tissue fascia, which can be seen separating the muscle from the subcutaneous tissue superficial to it. The hyperechoic femoral nerve should be seen wedged between the iliopsoas muscle and the fascia iliaca, lateral to the femoral artery. The fascia lata (superficial in the subcutaneous layer) is more superficial and may have more then one layer. Moving the transducer laterally several centimeters brings into view the sartorius muscle covered by its own fascia as well as the fascia iliaca. Further lateral movement of the transducer reveals the anterior superior iliac spine (Figure 36-2). Additional anatomical detail can be seen in cross sectional anatomy in Section 7. Since the anatomy is essentially identical, it is not repeated here.
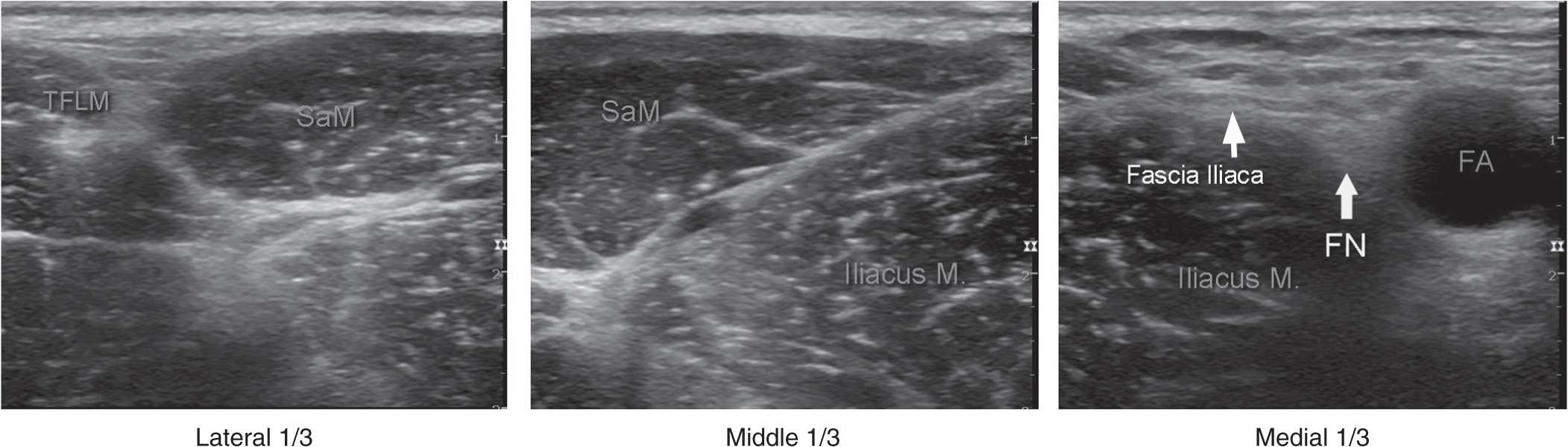
FIGURE 36-2. A panoramic view of ultrasound anatomy of the femoral (inguinal) crease area. From lateral to medial shown are tensor fascia lata muscle (TFLM), sartorius muscle (SaM), Iliac muscle, fascia iliaca, femoral nerve (FN), and femoral artery (FA). The lateral, middle and medial 1/3s are derived by dividing the line between the FA and anterior-superior iliac spine in three equal 1/3 sections.
Distribution of Blockade
The distribution of anesthesia and analgesia that is accomplished with the fascia iliaca block depends on the extent of the local anesthetic spread and the nerves blocked. Blockade of the femoral nerve results in anesthesia of the anterior and medial thigh (down to and including the knee) and anesthesia of a variable strip of skin on the medial leg and foot. The femoral nerve also contributes to articular fibers to both the hip and knee. The lateral femoral cutaneous nerve confers cutaneous innervation to the anterolateral thigh. For a more comprehensive review of the femoral and lateral femoral cutaneous nerves and lumbar plexus nerve distribution, refer to Chapter 01, Essential Regional Anesthesia Anatomy.
Equipment
Equipment needed is:
• Ultrasound machine with linear transducer (6–14 MHz), sterile sleeve, and gel
• Standard nerve block tray (described in the equipment section)
• Two 20-mL syringes containing local anesthetic
• 80- to 100-mm, 22-gauge needle (short bevel aids in feeling the fascial “pops”)
• Sterile gloves
Landmarks and Patient Positioning
This block is typically performed with the patient in the supine position, with the bed or table flattened to maximize access to the inguinal area (Figure 36-3). Although palpation of a femoral pulse is a useful landmark, it is not required because the artery is quickly visualized by placement of the transducer transversely on the inguinal crease, followed by slow movement laterally or medially.
FIGURE 36-3. The ruler is positioned to divide the distance between the femoral artery and anterior superior spine in 3 equal parts as described in Figure 36-2.

Full access? Get Clinical Tree








