Transverse ultrasound imaging of the lumbar vertebral level L3–L4 in a 1-month-old infant. Epidural space lies between the ligamentum flavum (LF) and the posterior dura mater (DM). Note the anterior placement of the cauda equina fibers (hyperechoic dot and linear structures) within the thecal sac and the anechoic space occupied by the cerebrospinal fluid.
The sagittal scan provides a wide longitudinal view of several intervertebral spaces (Figure 18.2). A paramedian approach gives the best position to visualize the neuraxis. The first osseous structure visualized appears as a “sawtooth” hyperechoic line characteristic of the complex formed by the spinous process and lamina. Superficially, the erector spinae muscles lie on the lamina. In contrast, when the transducer moves laterally, the sonographic appearance of the articular processes of the facets joint produces an unbroken hyperechoic line. Through the intermittent interlaminae acoustic windows, the spinal canal is visible – posteriorly, the ligamentum flavum and dura mater forms two highly hyperechogenic lines. The epidural space is a thin hypoechoic linear zone between these two hyperechoic lines. During the initial scanning or scout scan at the L3/4 and L4/5 interlaminar spaces, the nerve roots comprising the cauda equina lie in the anterior portion of the thecal sac and produce multiple horizontal hyperechoic striae. Cranial translation of the probe allows determination of the level of the conus medullaris (Figure 18.2). In children older than 1 year of age, the normal position is classically established within the confines of the lower third of the body of L1 and the upper third of L2. In the neonate, the normal spinal anatomy is such that the spinal cord ends lower down the vertebral column at L3/4 and usually at the top of the body of L3 in a term infant or the bottom of the body of L3 in a preterm infant. In the sagittal view, cephalad to the conus, spinal cord is broadly hypoechoic with hyperechoic outer layer due to the reflection of the pia mater and a central line of hyperechogenicity reflecting the median sulcus.
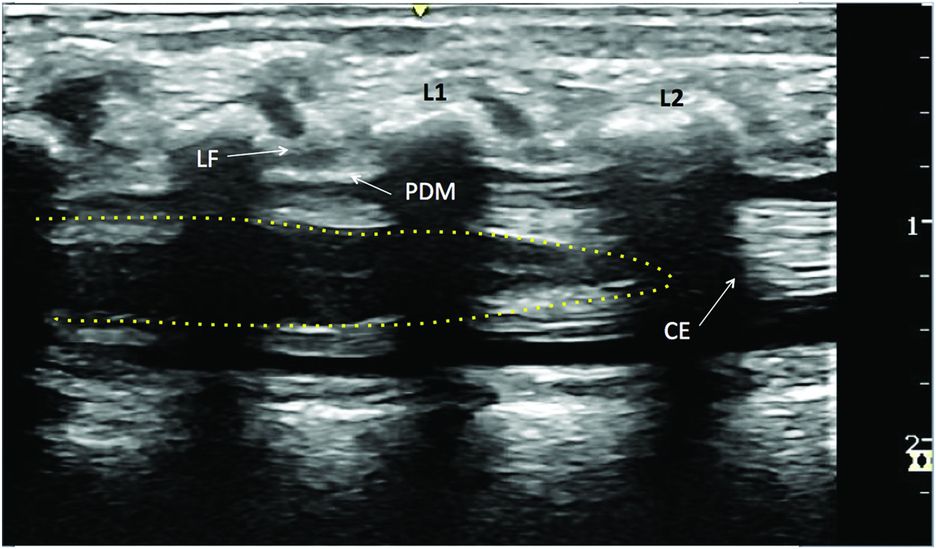
Longitudinal ultrasound imaging of the lumbar vertebral in a 1-month infant. Epidural space lies between the ligamentum flavum (LF) and the posterior dura mater (PDM). Cauda equina (CE) produces multiple horizontal hyperechoic striae. The yellow dotted line represents the conus medullaris.
Landmarks
In the most common situation where the child is anesthetized, the patient is placed in the lateral decubitus position with the knees drawn up to the chest and the head bent forward. Ultrasonography provides useful pre-puncture information on neuraxial structures, such as the location of the position of the conus medullaris and the dural sac and the detection of unknown structural abnormalities. Furthermore, the knowledge of the ideal intervertebral level of skin puncture, on the one hand, and of the angle and depth of needle insertion, on the other hand, enhances and improves the safety of the procedure (Grau et al., 2001; Tsui and Suresh, 2010). The main objective involves identifying the target intervertebral space that correlates with the required innervation for the surgical procedure and to estimate the depth of the epidural and intrathecal spaces. Both the transverse and longitudinal views are useful for this pre-procedural evaluation.
Block performance
Ultrasound scanning of the neuraxis is more complicated than peripheral blocks and multiple views are often required to generate a complete picture of the sonoanatomy. Each view has particular benefits and limitations – a combination of scanning positions may offer the best approach.
In the longitudinal approach or scan, the paramedian window appears to provide the best access for a sonoanatomic review of the spine (Grau et al., 2001). The probe is placed parallel to the long axis of the vertebral column, just lateral to the spinous processes in the midline and tilted to orient the ultrasound beam in a medial direction toward the median sagittal plane (Figure 18.3). For the transverse scan, the transducer is rotated through 90 degrees and positioned perpendicular to the spine between 2 spinous processes to get free of the acoustic shadow (Figure 18.4).
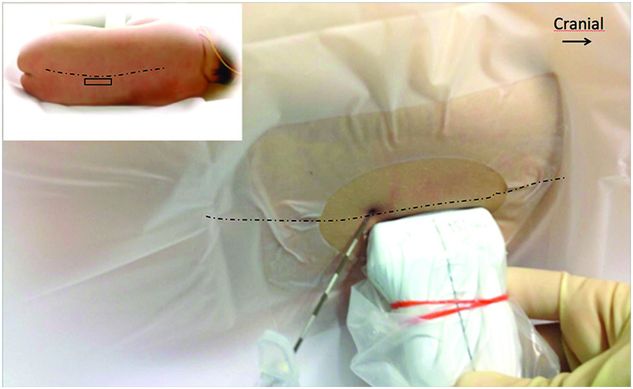
Patient position with probe placement for paramedian longitudinal scan and in-plane Tuohy needle insertion.
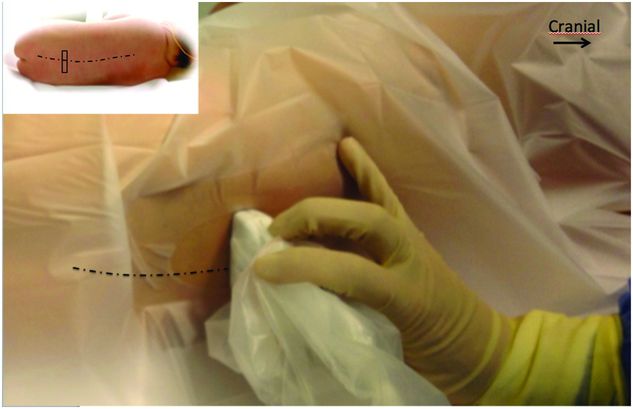
Patient position with probe placement for transverse view.
It should be noted that ultrasound neuraxial blocks are generally using ultrasonography as “assistance,” although real-time ultrasound guidance for epidural block techniques has also been reported in children (Rapp et al., 2005; Willschke et al., 2007). This practice is still in its infancy in clinical practice because of the complexity of its implementation requiring frequently the need for an extra pair of hands dedicated to handling the ultrasound probe. However, direct visualization of drug spread, concomitant ventral movement of the dura mater, and the expansion of the epidural space, confirm the epidural location while the catheter insertion can be identified and visualized immediately.
According to body weight and the morphology of the child, the size of a blunt tip “Tuohy” type needle is carefully determined (Table 18.1): for neonates, a 20-gauge 50 mm needle combined with a 24-gauge catheter is advocated. An intermediate 19-gauge needle with 24-gauge catheter is also suitable for an infant until 6 months of age. For older children, an 18-gauge needle and 20-gauge catheter is commonly used.
| Age (months) | <1 | 1–6 | >6 | |
|---|---|---|---|---|
| Tuohy needle | 20-G 50 mm | 19 / 20-G 50 mm | 18-G 50 / 80 mm | |
| Drug Induction dose | Concentration | Levobupivacaine 0.125% Ropivacaine 0.1% | Levobupivacaine 0.125%-0.25% Ropivacaine 0.1%-0.2% | Levobupivacaine 0.25% Ropivacaine 0.2% |
| Volume | 0.5-0.7 ml/kg (max 1.6 mg/kg) | 05–0.7 ml/kg (max 1.8 mg/kg) | 0.5-0.7 ml/kg (max 2 mg/kg or 15 ml) | |
| Adjuvant (µg / ml LA) | – | Clonidine 0.5–1 µg/ml Sufentanil 0.1–0.5 µg/ml Fentanyl 0.5–1 µg/ml | Clonidine 0.5-1 µg/ml Sufentanil 0.1-0.5 µg/ml Fentanyl 0.5-1 µg/ml | |
| Drug Infusion dose | Concentration | Levobupivacaine 0.125% Ropivacaine 0.1% | Levobupivacaine 0.125% Ropivacaine 0.1% | Levobupivacaine 0.25% Ropivacaine 0.2% |
| Maintenance | 0.2 ml/kg/h | 0.2 ml/kg/h | 0.2 ml/kg/h | |
| Adjuvant (µg/ml LA) | – | Clonidine 0.5–1µg/ml Sufentanil 0.1–0.2 µg/ml Fentanyl 0.5–1 µg/ml | Clonidine 0.5-1µg/ml Sufentanil 0.1-0.2 µg/ml Fentanyl 0.5-1 µg/ml | |
| PCEA NCEA | – | – | Basal: 0.08-0.1 ml/kg/ h Bolus: 0.1 ml/kg/h Refractory period: 20-30 mn Max/h: 0.2 ml/kg/h | |
G, gauge; LA, local anesthetic; PCEA, patient-controlled epidural analgesia; NCEA, nurse-controlled epidural analgesia.

Full access? Get Clinical Tree








