Ultrasound-Guided Cervical Sympathetic Block
Michael Gofeld
 Background and indications: Stellate ganglion block technique was first described in the 1930s. First implemented by LEriche, and further refined by Findley and Patzer, the method has been practiced without major modifications since that time.1 It is a common intervention in the diagnosis and management of sympathetically maintained pain and vascular insufficiency of upper extremities. In addition, the block has been advocated in a variety of medical conditions, such as phantom pain, postherpetic neuralgia, cancer pain, cardiac arrhythmias, orofacial pain, and vascular headache.2
Background and indications: Stellate ganglion block technique was first described in the 1930s. First implemented by LEriche, and further refined by Findley and Patzer, the method has been practiced without major modifications since that time.1 It is a common intervention in the diagnosis and management of sympathetically maintained pain and vascular insufficiency of upper extremities. In addition, the block has been advocated in a variety of medical conditions, such as phantom pain, postherpetic neuralgia, cancer pain, cardiac arrhythmias, orofacial pain, and vascular headache.2The anatomy and position of the stellate ganglion has been confirmed by dissection, magnetic resonance, and computed tomography.3, 4, 5, 6, 7and 8 The stellate ganglion, or cervicothoracic ganglion, is described as a structure 1 to 2.5 cm in length, approximately 1 cm in width, and 0.5 cm thick. It is present in about 80% of the population as a fusion of the inferior cervical ganglion and the first thoracic ganglion. The shape of the ganglion may be fusiform, triangular, or globular.6 The ganglion sits just anterior to the transverse process of C7 and superior or anterior to the neck of the first rib.
An inferior C7 approach for stellate ganglion block has been described.9 The more common approach is administered according to anatomical landmarks: the prominent anterior tubercle of the C6 vertebra (Chassaignac tubercle), the cricoid cartilage, and the carotid artery.4 At the level of C6, only the traversing sympathetic fibers or middle cervical ganglion can be found.10 Thus, the procedure at this level should be named the cervical sympathetic block. Ultrasound-guided stellate ganglion blockade was described in 19954 but has recently gained popularity. A new lateral approach to the cervical sympathetic trunk has been recently described and validated against fluoroscopy.11,12
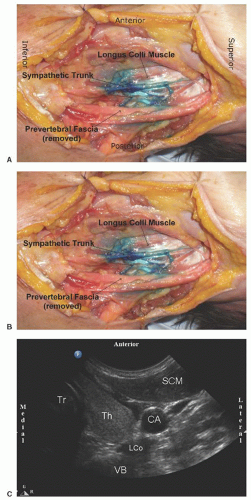
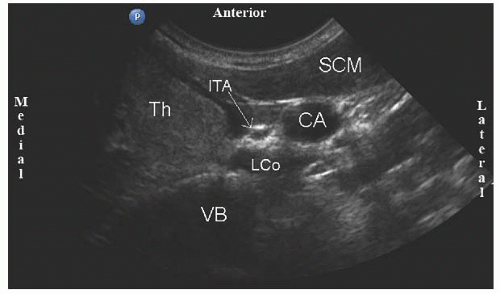
 Anatomy: The cervical sympathetic trunk is situated on the lateral surface of the longus colli muscle beneath the deep cervical fascia. The cervical sympathetic trunk lies medial to the anterior scalene muscle; lateral to the longus colli muscle, esophagus, trachea, and recurrent laryngeal nerve; and anterior to the transverse process of C6. A classic anterior neck sonogram at the level of the cricoid cartilage reveals the trachea medially, the carotid artery laterally, and the thyroid gland between those two structures. Immediately medial to the carotid artery, the inferior thyroid artery or the recurrent laryngeal nerve can be located (Fig. 45.1). The longus colli muscle is usually seen posterior to the thyroid gland on the anterolateral surface of the C6 vertebral body. On the left side of the neck, the esophagus is positioned just anterior to the longus colli muscle. Thus, insertion of a block needle in the usual trajectory would result in traversing the thyroid gland and esophagus. Although displacement of the carotid artery and thyroid by a pediatric-type curved transducer creates a passage for needle placement (Fig. 45.2), this approach requires application of pressure that may be very unpleasant and does not eliminate the chance for vascular and visceral damage.
Anatomy: The cervical sympathetic trunk is situated on the lateral surface of the longus colli muscle beneath the deep cervical fascia. The cervical sympathetic trunk lies medial to the anterior scalene muscle; lateral to the longus colli muscle, esophagus, trachea, and recurrent laryngeal nerve; and anterior to the transverse process of C6. A classic anterior neck sonogram at the level of the cricoid cartilage reveals the trachea medially, the carotid artery laterally, and the thyroid gland between those two structures. Immediately medial to the carotid artery, the inferior thyroid artery or the recurrent laryngeal nerve can be located (Fig. 45.1). The longus colli muscle is usually seen posterior to the thyroid gland on the anterolateral surface of the C6 vertebral body. On the left side of the neck, the esophagus is positioned just anterior to the longus colli muscle. Thus, insertion of a block needle in the usual trajectory would result in traversing the thyroid gland and esophagus. Although displacement of the carotid artery and thyroid by a pediatric-type curved transducer creates a passage for needle placement (Fig. 45.2), this approach requires application of pressure that may be very unpleasant and does not eliminate the chance for vascular and visceral damage.
Full access? Get Clinical Tree