Transverse sonoanatomy of the sacral (sacrum cornu (SC), sacrococcygeal ligament above sacral hiatus, coccyx) – the “frog eye sign.”
Longitudinal scan
The sagital sonogram of the sacrum shows the sacrococcygeal ligament, the base of the sacrum, and the sacral hiatus. In neonates and young infants the tapered end of the dural sac with cerebrospinal fluid (CSF), the cauda equine, and the anterior and posterior epidural space filled with fat may be visualized in the sacral canal. The dura mater is hyperechoic and forms the anterior and posterior border of the subarachnoid space (Figure 20.2).
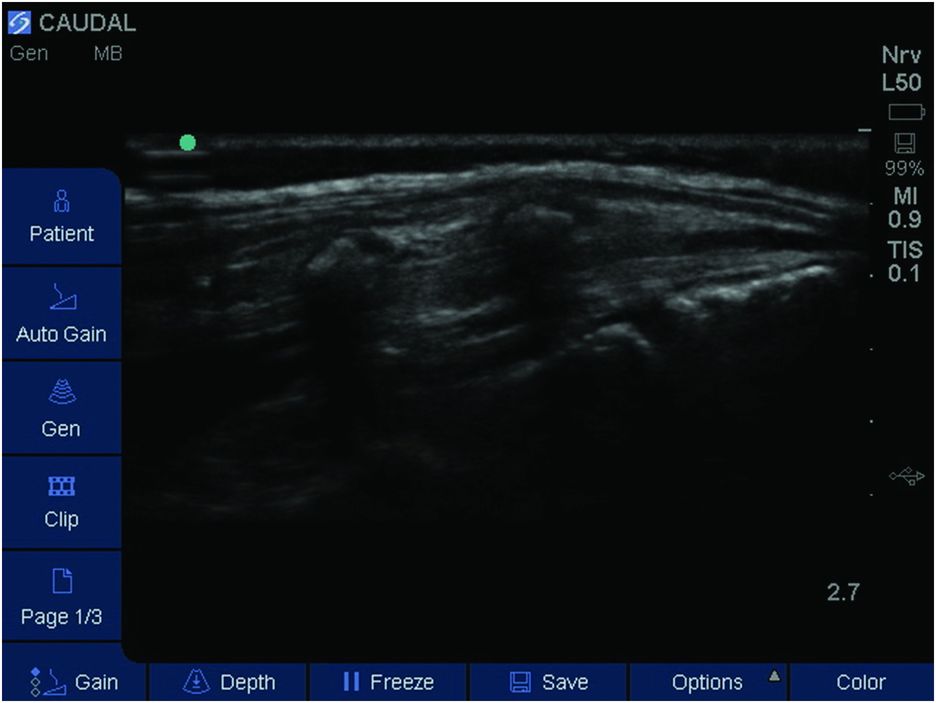
Sagittal sonoanatomy of the sacrum.
Landmarks
The patient is usually in the left lateral position with the knees drawn up to the chest. Flexing helps to palpate the sacral cornua better and brings the end of the dural sac cranially. Successful performance of a caudal epidural starts with the accurate identification of the sacral hiatus. The sacral hiatus lies at the third point of an equilateral triangle formed with the two posterior superior iliac spines (look for the dimples in the skin). The cornua are palpable on either side of the hiatus. Two cornua are easily palpable in infants and children, and the sacrococcygeal membrane is sometimes visible through the skin because of the absence of the sacral fat pad, which usually develops at puberty.
The probe is positioned directly over the sacral cornua in the transverse plane to obtain a transverse view of the sacral hiatus (Figure 20.3). The transducer can be rotated in the sagittal plane and placed between the two cornua to obtain a longitudinal view of the caudal space (Figure 20.4). When anatomic landmarks are difficult to identify, the placement of the probe at the level of coccyx with subsequent scanning toward the sacral canal will help clinician to localize relevant structures.

Patient position, probe placement, and in-plane needle technique.
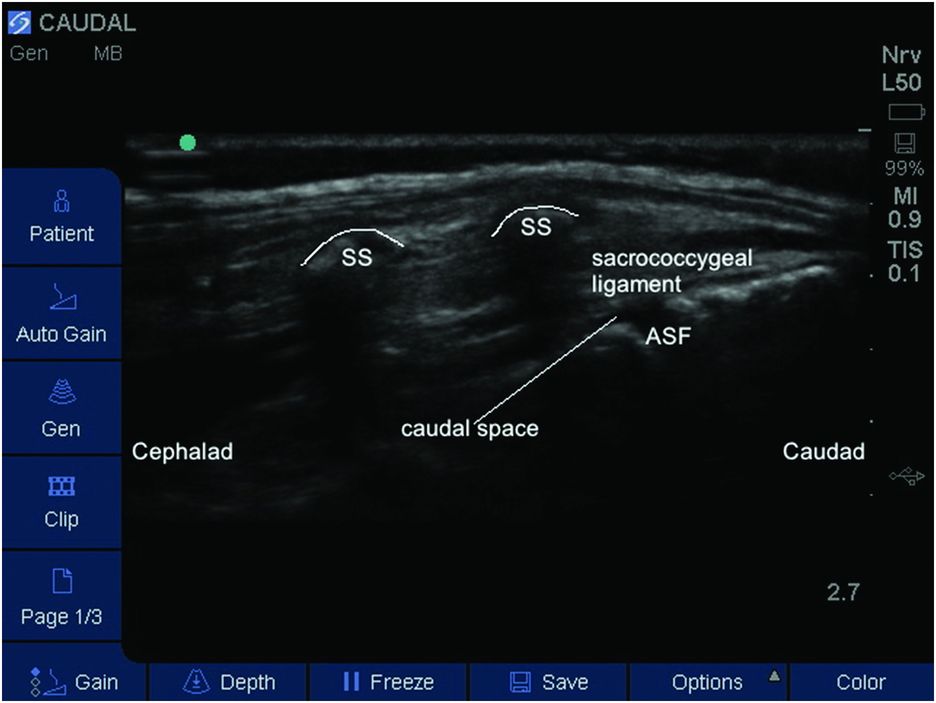
Labeled sagittal sonoanatomy for caudal block (sacrococcygeal ligament, sacral spine (SS), caudal space, anterior sacral foramina (ASF)).
Block performance
The child is placed in the lateral position and the landmarks for caudal puncture are identified (Figure 20.3).
Ultrasound imaging is performed using a high frequency linear array probe. The linear ultrasound probes with a 38-mm active surface area (or probes with 25-mm active surface area in smaller children), with high frequencies in the range 8–14 MHz, allow a good compromise between excellent resolution for superficial structures and good penetration depths. Caudal needles (22-gauge/35 mm or 20-gauge/50 mm) with a dull Crawford type bevel and precision-ground stylets in order to minimize tissue coring are recommended. Depth and gain settings are adjusted for optimal image quality.
The ultrasound probe covered with a sterile sheath is placed between the sacral cornua in sagittal plane and the needle is advanced under real-time guidance into the sacral canal through the sacrococcygeal ligament. With in-plane technique the entire length of the needle can be visualized, including the tip (Figure 20.5). The needle is advanced at an angle of approximately 20 degrees, so that it is parallel to the posterior surface of the sacrum and the risk of insertion into deeper structures is low. Once a “pop” is felt and/or the needle is visualized on the sonogram, the correct position of the needle in the caudal epidural space has to be confirmed. This is done by injecting a test bolus of saline (0.1–0.2 ml/kg) and observing in real-time the anterior displacement of posterior dura. The use of saline prevents wastage of LA with inadequate needle positioning, and if injected intravascularly or intrathecally does not put the patient at risk. Absence of dura displacement could be associated with intrathecal or intravascular positioning of the needle. The needle should be withdrawn and repositioned. After confirming the correct placement of the needle, the calculated dose of LA (Table 20.1) is injected in aliquots. The cephalad spread of the LA within the epidural space can be visualized by the use of color Doppler.
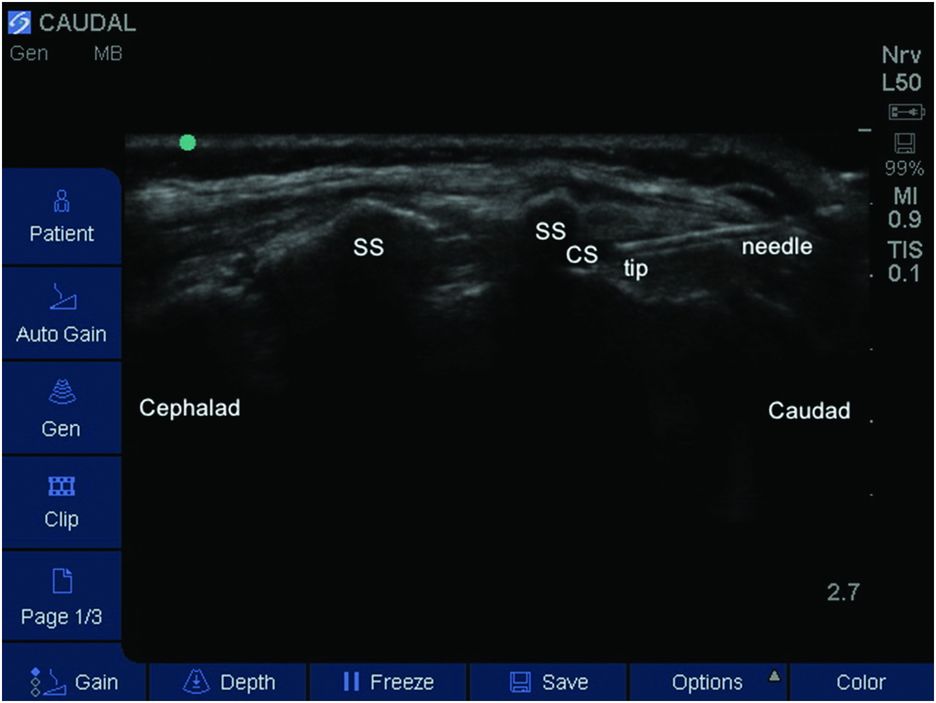
Ultrasound-guided caudal block with needle in situ. CS, caudal space; SS, sacral spine.
| Site of incision | Volume (ml/kg) |
|---|---|
| S1 (ankle, knee surgery) | 0.50 |
| L1 (hip surgery, hernia repair) | 0.75 |
| T10 (abdominal subumbilical surgery) | 1.00 |
With the out-of-plane approach, the sacral hiatus is firstly scanned at the sacral cornua in a transverse plane (Figure 20.1). With the ultrasound image of hiatus in the middle of ultrasound screen, the puncture site is positioned caudad adjacent to the midpoint of the transducer. Once a “pop” is felt and/or the needle is visualized in the hiatus a test dose saline is injected. Correct position of the needle in the caudal epidural space is confirmed by a localized turbulence or a dilation of the hiatus (displacing the sacrococcygeal ligament upward) during injection. The LA is injected slowly under ultrasound visualization. With transverse ultrasound scanning, the spread observed from the needle is rather wide and it may be difficult to ensure accurate location of the tip.
A successful block is defined as no motor or hemodynamic response (increase in mean arterial pressure or heart rate of more than 15% compared with baseline values) to skin incision and to subsequent surgical procedure.
A single shot caudal block provides relatively brief analgesia (4–8 h). Adjuvants are used to prolong the duration of analgesia. A dose of 33–50 μg/kg of preservative-free morphine in the caudal epidural solution improves the quality and duration of analgesia (12–24 h), but can be associated with itching, nausea, urinary retention, and respiratory depression. High doses (>33 μg/kg) require admission to a high dependency unit for respiratory monitoring (Krane et al., 1989).
The addition of clonidine (an α2-adrenergic agonist) 1–3 μg/kg, can provide prolonged analgesia (lasting for up to 12 h) without causing significant side effects. Doses greater than 2 μg/kg can be associated with increased sedation, bradycardia, hypotension, or respiratory depression. Clonidine should be avoided in young infants, as post-operative apnea can occur (Galante, 2005).
The addition of ketamine (a NMDA-receptor antagonist) to LA nearly triples the duration of analgesia. A dose of 0.5 mg/kg is considered safe (Semple et al., 1996). Preservative-free S-ketamine is available in some countries. Despite not being associated with significant side effects, there are still concerns regarding possible neurotoxicity (Vranken et al., 2006; Johr and Berger, 2012).
Technique failure is usually related to a suboptimal positioning of the probe or, in older patients, to increased sacrum ossification leading to inadequate view of the needle and anatomic landmarks.

Full access? Get Clinical Tree








