Ultrasound-Guided Axillary Brachial Plexus Block
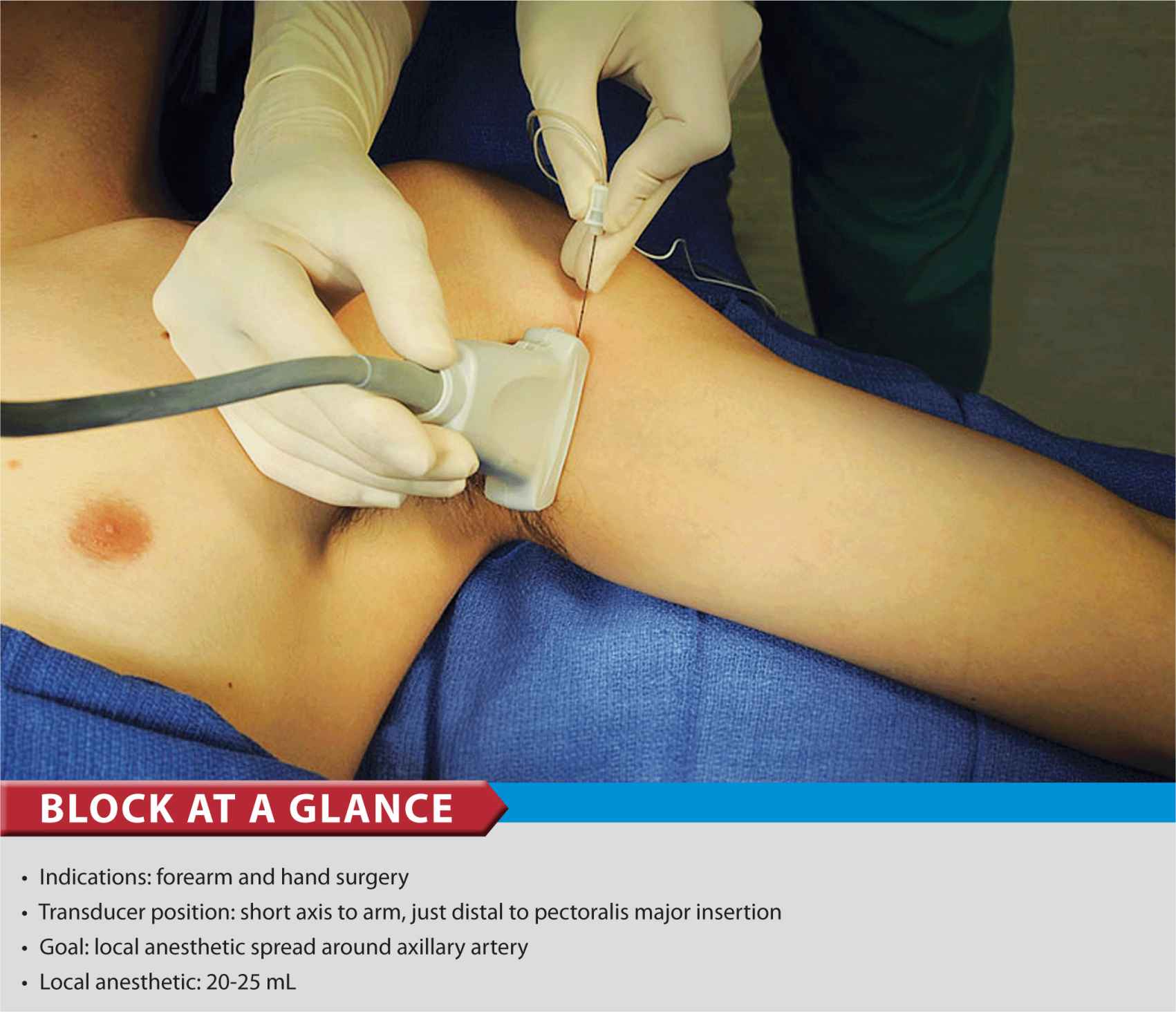
FIGURE 32-1. Transducer position and needle insertion in ultrasound-guided axillary brachial plexus block.
General Considerations
The axillary brachial plexus block offers several advantages over the other approaches to the brachial plexus. The technique is relatively simple to perform, and may be associated with a relatively lower risk of complications as compared with interscalene (e.g., spinal cord or vertebral artery puncture) or supraclavicular brachial plexus block (e.g., pneumothorax). In clinical scenarios in which access to the upper parts of the brachial plexus is difficult or impossible (e.g, local infection, burns, indwelling venous catheters), the ability to anesthetize the plexus at a more distal level may be important. The axillary brachial plexus block is also relatively simple to perform with ultrasound because of its superficial location. Although individual nerves can usually be identified in the vicinity of the axillary artery, this is not necessary because the deposition of local anesthetic around the axillary artery is sufficient for an effective block.
Ultrasound Anatomy
The structures of interest are superficial (1–3 cm), and the pulsating axillary artery can be identified usually within a centimeter of the skin surface on the anteromedial aspect of the proximal arm, Figure 32-2. The artery can be associated with one or more axillary veins, often located medially to the artery. Importantly, an undue pressure with the transducer during imaging may obliterate the veins, rendering veins invisible and prone to puncture with the needle if care is not taken to avoid it. Surrounding the axillary artery are three of the four principal branches of the brachial plexus: the median (superficial and lateral to the artery), the ulnar (superficial and medial to the artery), and the radial (posterior and lateral or medial to the artery) nerves (Figure 32-2). These are seen as round hyperechoic structures, and although the previously mentioned locations relative to the artery are frequently encountered, there is considerable anatomic variation from individual to individual,. Three muscles surround the neurovascular bundle: the biceps brachii (lateral and superficial), the wedge-shaped coracobrachialis (lateral and deep), and the triceps brachii (medial and posterior). The fourth principal nerve of the brachial plexus, the musculocutaneous nerve, is found in the fascial layers between biceps and coracobrachialis muscles, though its location is variable and can be seen within either muscle. It is usually seen as a hypoechoic flattened oval with a bright hyperechoic rim. Moving the transducer proximally and distally along the long axis of the arm, the musculocutaneous nerve will appear to move toward or away from the neurovascular bundle in the fascial plane between the two muscles. Refer to Chapter 1, Essential Regional Anesthesia Anatomy for additional information on the anatomy of the axillary brachial plexus and its branches.
FIGURE 32-2. Cross-sectional anatomy of the axillary fossa and the transducer position to image the brachial plexus. The brachial plexus (BP) is seen scattered around the axillary artery and enclosed in the adipose tissue compartment containing BP, axillary artery (AA), and axillary vein (AV). MCN, musculocutaneous nerve.
Distribution of Blockade
The axillary approach to brachial plexus blockade (including musculocutaneous nerve) results in anesthesia of the upper limb from the midarm down to and including the hand. The axillary nerve itself is not blocked because it departs from the posterior cord high up in the axilla. As a result, the skin over the deltoid muscle is not anesthetized. With nerve stimulator and landmark-based techniques, the blockade of the musculocutaneous is often unreliable, leading to a lack of blockade on the lateral side of the forearm and wrist. This problem is remedied easily with the ultrasound-guided approach because the musculocutaneous nerve is readily apparent and reliably anesthetized. When required, the medial skin of the upper arm (intercostobrachial nerve, T2) can be blocked by an additional subcutaneous injection just distal to the axilla, if required. For a more comprehensive review of the brachial plexus distribution, see Chapter 1.
Equipment
Equipment needed includes the following:
• Ultrasound machine with linear transducer (8–14 MHz), sterile sleeve, and gel
• Standard nerve block tray (described in the equipment section)
• Syringes with local anesthetic (20–25 mL)
• 4-cm, 22-gauge short-bevel insulated stimulating needle
• Peripheral nerve stimulator
• Sterile gloves
Landmarks and Patient Positioning
The axillary brachial plexus block requires access to the axilla. Therefore abduction of the arm 90° is an appropriate position that allows for transducer placement and needle advancement, as well as patient comfort (Figure 32-3). Care should be taken not to overabduct the arm because that may cause discomfort as well as produce tension on the brachial plexus, theoretically making it more vulnerable to needle or injection injury during the block procedure.
FIGURE 32-3. Patient position and insertion of the needle for ultrasound-guided (in plane) axillary brachial plexus block. All needle redirections except occasionally for the musculocutaneous nerve are done through the same needle insertion site. Seldom, another insertion of the needle is made to block the musculocutaneous nerve.
The pectoralis major muscle is palpated as it inserts onto the humerus, and the transducer is placed on the skin immediately distal to that point perpendicular to the axis of the arm. The starting point should result in part of the transducer overlying both the biceps and the triceps muscles (i.e., on the medial aspect of the arm). Sliding the transducer across the axilla will bring the axillary artery and brachial plexus into view, if not readily apparent.
Technique
With the patient in the proper position, the skin is disinfected and the transducer is positioned in the short axis orientation to identify the axillary artery (Figure 32-4A about 1 to 3 cm from the skin surface. Once the artery is identified, an attempt is made to identify the hyperechoic median, ulnar, and radial nerves (Figure 32-4B). However, these may not be always well seen on an ultrasound image. Frequently present, a reverberation artifact deep to the artery is often misinterpreted for the radial nerve. Pre-scanning should also reveal the position of the musculocutaneous nerve, in the plane between the coracobrachialis and biceps muscles (a slight proximal-distal movement of the transducer is often required to bring this nerve into view) (Figure 32-5).

FIGURE 32-4. (A,B) Median (MN), ulnar (UN), and radial (RN) nerves are seen scattered around the axillary artery with the tissue sheath (white-appearing tissue fasciae around the artery) containing nerves and axillary vessels. The musculocutaneous nerve (MCN) is seen between the biceps and coracobrachialis (CBM) away from the rest of the brachial plexus. AA, axillary artery.
FIGURE 32-5. Musculocutaneous nerve (MCN) is seen approximately 3 cm from the axillary neurovascular bundle (around AA). MCN in this image is positioned between the biceps and coracobrachialis muscles (CBM). MCN must be blocked with a separate injection of local anesthetic for a complete axillary brachial plexus block.
The needle is inserted in-plane from the cephalad aspect (Figures 32-1 and 32-3) and directed toward the posterior aspect of the axillary artery (Figure 32-6).
FIGURE 32-6. Needle insertions for axillary brachial plexus block. Axillary brachial block can be accomplished by two to four separate injections (1–4) to accomplish a block of the entire brachial plexus. MCN, musculocutaneous nerve; RN, radial nerve; MN, median nerve; UN, ulnar nerve.
As nerves and vessels are positioned together in the neurovascular bundle by adjacent musculature, advancement of the needle through the axilla may require careful hydrodissection with a small amount of local anesthetic or other injectate. This technique involves the injection of 0.5 to 2 mL, which “peels apart” the plane in which the needle tip is continuously inserted. The needle is then advanced a few millimeters and more injectate is administered.
Local anesthetic should be deposited posterior to the artery first, to avoid displacing the structures of interest deeper and obscuring the nerves, which is often the case if the median or ulnar nerves are injected first. Once 5 to 10 mL is administered, the needle is withdrawn almost to the level of the skin, redirected toward the median and ulnar nerves, and a further 10 to 15 mL is injected in these areas to complete the circle around the artery. The described sequence of injection is demonstrated in Figure 32-7.
FIGURE 32-7. An image demonstrating the ideal distribution patterns of local anesthetic spread after three separate injections (1–3) to surround the axillary artery with local anesthetic and block the radial nerve (RN), median nerve (MN), and ulnar nerve (UN). Musculocutaneous nerve (MCN) is blocked with a separate injection (4) because it is often outside the axillary neurovascular tissue sheath. AA, axillary artery.
Finally, the needle is once again withdrawn to the biceps and redirected toward the musculocutaneous nerve. Once adjacent to the nerve (stimulation will result in elbow flexion), 5 to 7 mL of local anesthetic is deposited.
In an adult patient, 20 to 25 mL of local anesthetic is usually adequate for successful blockade. Complete spread around the artery is necessary for success but infrequently seen with a single injection. Two to three redirections and injections are usually necessary for reliable blockade, as well as a separate injection to block the musculocutaneous nerve. The block dynamics and perioperative management are similar to those described in Chapter 15.

Full access? Get Clinical Tree








