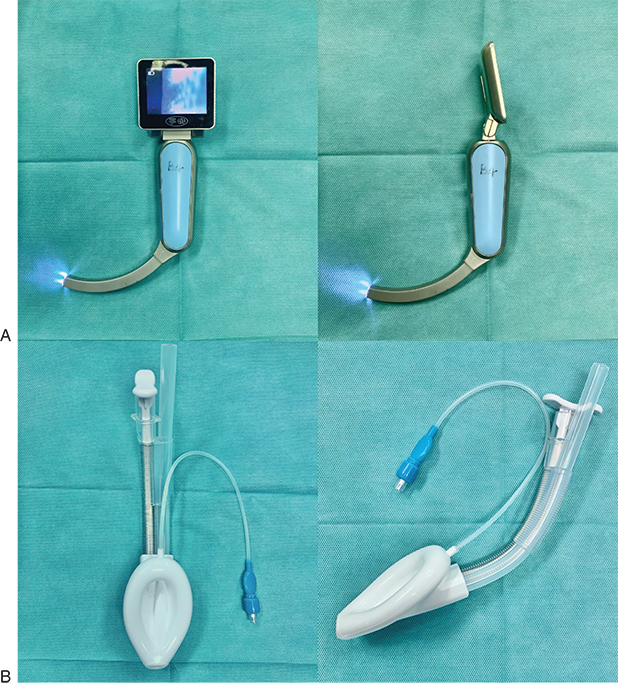
Jiaxi HE, Diego Gonzalez-RIVAS, Hui Liu, Qinglong Dong, Lixia Liang, Jianxing He, Shuben Li, Edmond Cohen An introduction of tubeless anesthesia for thoracic surgery in different aspects including airway management, pathophysiologic alteration, monitoring, types of anesthesia drugs, and potential complications. nonintubated; tubeless; thoracic surgery; spontaneous respiration; airway management; epidural anesthesia; paravertebral anesthesia Tubeless thoracic procedures are performed without an endotracheal tube while the patient is spontaneously breathing. Initially it was defined as an “awake” thoracic procedure, but the term was updated to “tubeless” because these procedures are performed with sedation and/or regional block of variable extent while maintaining spontaneous ventilation. For decades, the use of a double-lumen tube (DLT) and the insertion of chest tube drainage were considered mandatory for thoracoscopic pulmonary resection. Recently, an alternative minimally invasive tubeless approach to thoracic procedures is gaining popularity. The initial concern was that the iatrogenic surgical pneumothorax can be detrimental and not tolerated by a spontaneously breathing patient. In 2004 Pompeo et al.1 reported the resection of pulmonary nodules by conventional video-assisted thoracic surgery (VATS) under intravenous anesthesia without endotracheal intubation. In addition, under direct thoracoscopic vision, vagus nerve block and lidocaine sprayed on the surface of the lung are used to effectively abolish the cough reflex. Avoiding the positive pressure ventilation fulfills the goal of performing a less traumatic, safe operation with decreased postoperative pain and expeditious postoperative recovery. Airway management of thoracic surgery is crucial, and the challenge increases if the patients receive tubeless anesthesia. Previous studies show that airway-related emergencies occurred frequently during thoracic and tracheal surgeries.2,3 Therefore a thorough and meticulous airway management is indispensable, including preoperative evaluation, preparation, intraoperative monitoring, manipulation, and postoperative precaution. A detailed preoperative airway evaluation is crucial for tubeless anesthetic thoracic surgery. The anesthesiologist should review the patient medical history and symptoms and carefully evaluate any underlying respiratory diseases, which may put the patient at risk or jeopardize the procedure.4 In addition to the preoperative evaluation, pulmonary and cardiac function tests are indispensable in patients with hypersensitivity syndrome, asthma, chronic obstructive pulmonary disease (COPD) or a long-term smoking history. A bronchodilator challenge is recommended, depending on the patient medical history and his current medication. Furthermore, these underlying diseases should be evaluated preoperatively as a team approach in collaboration with the surgeon and the pulmonologists. The patients with poorly controlled respiratory diseases or pulmonary infection, including AECOPD (acute exacerbated COPD), should have a preoperative adequate antibiotics regime and surgery should be postponed until the therapy is completed. When tracheal or laryngeal surgeries are planned, characteristic signs and symptoms including stridor, hoarseness, and shortness of breath should raise a red flag as they usually indicate the presence of upper respiratory tract obstruction.5–8 A preoperative communication between anesthesiologists and surgeons is necessary for a smooth and safe procedure. Patients with a high body mass index (BMI) are not candidates for tubeless anesthesia because these patients have high oxygen consumption and carbon dioxide production owing to the high metabolic activity of body, tissue, and an increase in respiration work.9–11 An increased intraabdominal pressure decreases the compliance of the thoracic cavity and restricts lung expansion. Moreover, excessive adipose tissue in the pharyngolaryngeal area would cause upper airway obstruction and hypoventilation usually associated with sleep apnea. Most importantly, if indicated, they may be difficult to intubate in an emergency during the procedure. Therefore patients with a higher BMI should have an extensive evaluation and if the procedure is not urgent, they should be encouraged to lose weight.12–14 The criteria for patient selection for tubeless procedures are depicted in Box 37.1. Most importantly the patient should not have a difficult airway if the tubeless procedure needs to be converted to general anesthesia with an endotracheal tube. In case of emergency during the surgical procedure, a difficult airway cart should be immediately available. The cart should contain topical anesthetic medications, video laryngoscopy (Fig. 37.1A) and angulated video-bronchoscopy with all sizes of endotracheal tubes, including nasal Ring-Adair-Elwyn (RAE), oral RAE, microlaryngeal tube, flexometallic tubes and DLTs.7,14 Except for a patients with a difficult airway, laryngeal masks (see Fig. 37.1B) are used in most cases of tubeless procedures to secure the airway. After thoracotomy, topical anesthesia by spraying lidocaine on the surface of lung and hilum (see Fig. 37.2A), intercostal nerve block (see Fig. 37.2B), and vagal nerve block (see Fig. 37.2C) are highly recommended to decrease the irritation threshold to cough and tracheobronchial spasm.15 During the tubeless procedure, spontaneous respiration is maintained and therefore phrenic nerve block should be avoided.16,17 During the procedure the anesthesiologist should periodically use suction to remove mucus and sputum in the trachea and bronchus. In a patient where tracheostomy or bronchial resection is performed with a sleeve or reconstruction surgeries, close communication with the surgeon is crucial. When the tracheobronchial lumen is open, the oxygen concentration inside the trachea or bronchus is decreased and the blood or drainage may flow into the lumen to potentially cause an airway obstruction.18–21 Therefore increasing the oxygen supply and meticulous suctioning before opening the bronchial lumen are helpful to minimize these risks of hypoxemia and hypercarbia. Two phenomena occur when the patient is spontaneously breathing with an open chest that would need immediate treatment. Hypotension from mediastinal shift from vertical downward movement of the mediastinum and paradoxical breathing that causes movement of air from the nondependent lung into the dependent lung in inspiration and the opposite occurs during exhalation. This wasted ventilation results in hypoxemia and hypercarbia and can be treated by applying slight positive pressure with the face mask; this will usually immediately stabilize the patient. An overview of the intraoperative management, including the type of regional blocks, such as epidural, paravertebral, or intercostal block and vagal nerve block, the sedation and the airway management with laryngeal mask airway (LMA), high-flow nasal cannula, or nasal continuous positive airway pressure (CPAP), is depicted in Table 37.1. Table 37.1 BIS, Bispectral index; LMA, laryngeal mask airway. Courtesy of Edmond Cohen, MD. At the conclusion of the procedure, the laryngeal mask should be removed as soon as the patients regain their consciousness and the cough reflation gradually replaced by a facial mask or nasal tube instead. Saliva and secretions should be removed by gentle suction to clear the trachea and bronchus.22 Encouraging coughs and deep breaths are also important for rapid recovery.23 Coughs should not be encouraged after tracheal or laryngeal surgeries because of the risk of anastomotic dehiscence. (Box 37.2) The most important advantage of tubeless thoracic procedures is the avoidance of mechanical ventilation. There is no benefit to the lung when ventilated with positive pressure. Mechanical ventilation has a number of potential side effects, such as pressure-induced injury, lung overdistension from volutrauma, the release of a variety of proinflammatory mediators, atelectasis, and potential laryngeal or tracheal injuries. Avoidance of muscle relaxants will reduce the degree of atelectasis in the dependent zone of the lung from diaphragmatic dysfunction, will keep the ventilation/perfusion (V/Q) matching, eliminating the potential for residual neuromuscular blockade. That is particularly important in the thoracic patient who may have compromised lung mechanics, COPD, compromised chest wall mechanics from hyperinflation, or a patient with myasthenia gravis. In addition, airway irritation or sore throat from intubation and chest tube or urinary catheter insertion can be avoided, and may result in shorter hospital stay and improved patient satisfaction. Another major advantage of nonintubated VATS is to offer the potential for surgery to patients who may be considered too high risk for endotracheal general anesthesia. During the surgical procedure, patients are in the lateral decubitus position. The lung of operative hemithorax would collapse after thoracotomy. Although spontaneous respiration is maintained during tubeless procedures, the nerve block and topical anesthesia may decrease the respiration movement to some extent. This leads to decreased ventilation of well-perfused lung tissue, V/Q mismatch to results in hypoxemia, and hypercapnia.24,25 In the lateral decubitus position, the thoracic cavity on the nonoperative side is compressed by the patient’s mediastinal shift, which leads to restricted lung expansion that results in relative V/Q mismatch and hypoxemia. The transient hypoxemia or hypercapnia stimulates peripheral chemoreceptors and leads to increase respiratory rate and tidal volume. The increase in ventilation and perfusion to the nonoperative lung because of gravity and hypoxic pulmonary vasoconstriction (HPV) will improve the V/Q mismatch. To satisfy the oxygen consumption and improve the hypoxemia, incrementing oxygen supply is indicated. Because carbon dioxide has higher diffusion efficiency than oxygen, hypercapnia is uncommon during uncomplicated cases without airway obstruction or impaired diffusion.65–68 Often, to enhance the quality of the lung collapse, the surgeon would insufflate carbon dioxide (CO2) into the operative open chest, which may induce hypotension and hypercarbia. Close communication with the surgeon to adjust the insufflation pressure is essential. The longer the operation time, the higher the risk from CO2 insufflation would be, especially in complicated open airway cases including sleeve resection, tracheal, or carinal resection and reconstruction. In spontaneously breathing patient, once the tidal volume and respiratory rate increase, which are induced by hypoxemia, CO2 rebreathing would occur. However, hypercapnia is seldomly seen in these cases because of an increased tidal volume.29,30 Furthermore, connecting the laryngeal mask to the ventilator or increasing the oxygen supply would decrease the negative side effects from CO2 insufflation. Compared with the general anesthesia, tubeless anesthesia procedure requires intense and careful monitoring. Standard monitors, which include electrocardiogram, noninvasive arterial blood pressure, respiratory rate, pulse oximetry and end-tidal carbon dioxide (EtCO2), are measured through the laryngeal mask or nasal cannula. A bispectral index (BIS) is also required to monitor the depth of sedation. Two peripheral intravenous lines should be placed during tubeless thoracic surgery.31–33 Because it is tubeless anesthesia, a urinary catheter, and in selected cases invasive blood pressure measurement are not placed routinely unless there are strong indications for their placement. Therefore anesthesiologists should carefully record the volume of fluid infusion and monitor the noninvasive blood pressure and heart rate to maintain a stable hemodynamic status. The anesthesiologists should be aware of the vital signs, including anesthesia induction, pharyngeal mask placement, skin incision, and thoracotomy.34 This recommendation is derived from one of the largest series of tubeless patients from the Tor Vergata Hospital in Rome, Italy, that has formed the “Awake Thoracic Surgery Research Group” dedicated to performing thoracic operations in awake nonintubated patients. It reported that more than 1000 various tubeless thoracic procedures have been performed successfully, with a low conversion rate. Some of the procedures were performed Uniportal-tubeless.35 The target of tubeless anesthesia is always “less is more.” It means the surgeons, and anesthesiologists, goal is to achieve more with less procedure or drugs. The idea of the tubeless technique is that less procedure brings less invasiveness and less pain. Limiting drug usage leads to faster recovery. However, three major parts of anesthetic medications are necessary in any thoracic operation. Surgery may be an unpleasant experience with mental stress to the patients, with detrimental effects on their pathophysiology which may lead to alterations in vital signs.36 Intraoperative awareness is a significant problem, may induce panic attack, have postoperative consequences, and jeopardize the safety of surgery. Therefore sedation and amnesia are most important during the thoracic surgeries, especially prolonged operations, including lobectomy, sleeve lobectomy, or tracheal surgeries. Adequate sedation would offer a stable condition for surgeons to complete the surgeries in a stress-free environment for patients. During sedation, BIS monitoring is recommended and should be maintained between 40 and 60, for balanced respiration and hemodynamic stability. Before induction of anesthesia, midazolam and atropine are administered.37 Subsequently, target-controlled infusion (TCI) of propofol is given aiming to maintain BIS around 60.38,39 Inhaled anesthetics are not recommended during tubeless procedures, because it would be difficult to precisely control the depth of anesthesia under spontaneous respiration. The rate of the propofol infusion should be titrated to the patient BIS and vital signs.33
Tubeless Thoracic Procedures
Abstract
Keywords
Preoperative Evaluation
Intraoperative Management

Regional Blockade
Sedation
Airway Management
Advantages of Tubeless Thoracic Procedures
Ventilation/Perfusion With the Patient Breathing Spontaneously Withan Open Chest
Risk of Carbon Dioxide Insufflation
Monitoring
Anesthesia Sedation
Sedation and Amnesia

Full access? Get Clinical Tree


Tubeless Thoracic Procedures






