Traumatic Brain Injury
Meredith S. Tinti
Vicente H. Gracias
Peter D. Le Roux
Traumatic Brain Injury
Central nervous system (CNS) injury is the most common cause of death from injury. Two million people per year in the United States suffer traumatic brain injuries (TBIs), many as the result of motor vehicle crashes and falls. Approximately 50,000 deaths per year and 500,000 hospital admissions are attributable to head injury. Most of these victims are between the ages of 16 and 30 years and motor vehicle crashes are responsible for the majority of these injuries. The increasing use of seat belts and airbags has resulted in an estimated 20% to 25% reduction in traffic fatalities. However, the incidence of penetrating injury to the brain and spinal cord is increasing. As awareness of literature based methods for brain injury management grows, guidelines for TBI have been developed and have been shown to improve the outcome.
I. Anatomy and Physiology
The skull is particularly thin in the temporal region and thick in the occiput. The floor of the cranial cavity or the skull base is divided into three regions: Anterior (houses the frontal lobes), middle (contains the temporal lobes), and posterior cranial fossa (houses the lower brainstem and cerebellum).
The meninges cover the brain in three layers: Dura mater (fibrous membrane that adheres to the internal surface of the skull), arachnoid membrane, and pia mater (attached to the surface of the brain). Cerebrospinal fluid (CSF) circulates between the arachnoid membrane and pia mater in the subarachnoid space.
The brain is comprised of the cerebrum, cerebellum, and the brainstem.
The cerebrum is the largest and most well developed portion of the brain. It is responsible for language/communication, learning/memory, movement and sensory processing.
The cerebellum is located at the bottom of the brain. It is responsible for motor coordination and motor learning.
The brainstem consists of the posterior portion of the brain that adjoins the spinal cord. It consists of the midbrain, pons, and medulla. The reticular activating system (responsible for state of alertness) is within the midbrain and upper pons. The cardiorespiratory centers reside in the medulla.
The Monro–Kellie doctrine states that the total volume of intracranial contents must remain constant because of the rigid bony cranium. With an expanding mass lesion or cerebral edema, CSF and blood volume within the skull decrease to compensate and maintain intracranial pressure (ICP) within normal limits. This occurs until the point of decompensation on the pressure–volume curve is reached and then ICP dramatically increases.
Cerebral perfusion pressure (CPP) = Mean arterial pressure − ICP. Maintenance of cerebral perfusion is essential in the management of patients with severe closed head injury.
Normal cerebral blood flow (CBF) is approximately 50 mL/100 g brain/minute or 15% of cardiac output and this flow rate is tightly regulated to maintain the metabolic activity of the brain. CBF <20 mL/100 g brain/minute causes cerebral ischemia, and cell death occurs at approximately 5 mL/100 g brain/minute. CBF >65 mL/100 g brain/minute causes hyperemia of the brain and
raises ICP. CBF is determined by many factors, the most important of which is CPP.
Under normal circumstances, CPP is relatively constant due to the brain’s intact autoregulatory system. With TBI, this autoregulation can be lost and the practitioner must regulate the CPP, goal 60 to 70 mm Hg.
II. TBIs
Are categorized as mild (80%), moderate (10%), or severe (10%), depending on the level of neurologic dysfunction at the time of initial evaluation. Loss of consciousness (LOC) is an important indicator of TBI. Determination of the Glasgow Coma Scale (GCS) score as early as possible and then serially is essential. Classification of TBI is based on the GCS.
Mild head injury = GCS 13 to 15
Brief period of LOC or other signs of concussion (10% to 35% will have a lesion detected on CT)
Most prevalent type of brain injury
Diagnosis often missed at time of injury
Prognosis is excellent (although may have long lasting consequences)
Mortality rate 1%
Moderate head injury = GCS 9 to 12
Confused and may have focal neurologic deficits
Prognosis is good but 12% will progress to severe TBI
Mortality rate 5%
Severe head injury = GCS ≤8
Generally, the accepted definition of coma
Until recently, mortality was 40%. Mortality is still approximately 20%
Most survivors have significant disabilities
Early airway control is essential
Elevated ICP is a common cause of death and neurologic disability
Requires multi-modality treatment
III. Initial Evaluation and Treatment of Brain Injury
General
Patients suspected of having a head injury, particularly if confused or unresponsive, require emergency evaluation and treatment at a center with capabilities for immediate neurosurgical intervention. General objectives are rapid diagnosis and evacuation of intracranial mass lesions, expedient treatment of extracranial injuries, and avoidance of secondary brain injury.
Secondary brain injury is due to hypoxia or hypotension. Other secondary insults such as hyperglycemia, hypothermia, and anemia may also exacerbate outcome during the hospital course.
All patients with clinical signs of brain injury should be evaluated with CT. Those with findings on CT scan require admission to the hospital and serial neurologic examinations.
Severe brain injury is associated with cerebral ischemia. Therefore, a principal therapeutic goal is to enhance cerebral perfusion and oxygenation and avoid further ischemic injury to the brain.
ICU admission should be considered in all patients with moderate to severe TBI.
Changes in motor score portion of GCS are most prognostic.
Initial management of the unresponsive patient with brain injury—ABCs
Airway/Breathing—intubation with controlled ventilation
If possible, perform a focused neurologic examination, including assessment of GCS, pupillary response, and all four extremity movements, before intubation and pharmacologic paralysis.
Avoid routine hyperventilation. Hyperventilation causes cerebral vasoconstriction and can worsen cerebral ischemia. Hyperventilation is indicated only in the setting of abrupt neurologic deterioration with suspected herniation and is used as a short-term rescue therapy.
Circulation—venous access
Restore intravascular volume, blood pressure, and perfusion.
Avoid hypotonic and dextrose-containing solutions.
Disability—immobilization and serial neurologic examinations
Immobilize the patient with full spine precautions and cervical spine (C-spine) collar. Assume that all patients with TBI have a spine injury until proven otherwise.
Repeat neurologic examination and assessment of GCS. Documentation of the GCS in patients who are intubated or “tubed” should be noted by a T (i.e., GCS 11T) and in patients who are intubated and pharmacologically paralyzed, with TP (i.e., GCS 3TP). This allows meaningful interpretation of the GCS score.
Add pharmacologic agents if agitated or combative
Short-acting agents are recommended.
Analgesia: Fentanyl or morphine
Sedation: Propofol, avoid long-acting benzodiazepines
Paralytics: Vecuronium bromide, cisatracurium, or succinylcholine
Monitoring—monitor and record blood pressure and O2 saturation continuously.
Laboratory evaluation—check arterial blood gasses (ABGs), blood glucose, electrolytes, prothrombin time (PT), partial thromboplastin time (PTT), hematocrit, and platelet count. With active therapy for elevated ICP, serum sodium levels and osmolality should be tracked frequently.
Radiologic diagnosis of brain injury. Rapid acquisition of a computed tomographic (CT) of the head and complete C-spine (if time permits) should be obtained for all classifications of brain injury. On the basis of time, distance, and local capabilities, transfer may be necessary. Rapid referral to a center capable of immediate neurosurgical intervention may be required. Do not delay transport to definitive care to obtain a CT of the head. Early diagnosis and evacuation of cranial mass lesions are critical.
Secondary management of brain injury
The avoidance of secondary brain injury is essential. Secondary brain injury is produced by hypoxia and hypotension. A single episode of hypotension (systolic blood pressure <90 mm Hg) in the adult will worsen prognosis and can increase mortality up to 50%.
The GCS obtained in the emergency department may be a more reliable assessment of the severity of brain injury than the GCS obtained in the field.
The GCS cannot be assessed by simple observation and requires stimulation of the patient. In cases of asymmetry in either eye opening or motor scores, the best score is used.
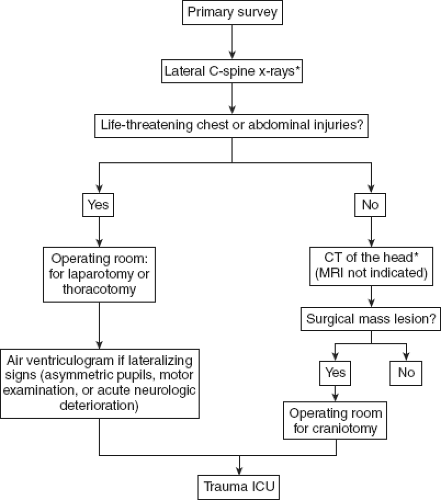
Should emergent operative intervention be required and CT capabilities not available, a lateral C-spine x-ray study should be obtained to evaluate for gross injury or malalignment of the C-spine (Fig. 23-1). If available, and time permits, rapid C-spine CT should be used to detect fractures as well.
IV. Treatment of Severe TBI
Intensive care management of patients with severe TBI (GCS ≤ 8). The goal is to prevent secondary brain injury by limiting focal cerebral ischemia, preventing cerebral hypoxia, and maintaining adequate cerebral perfusion. This can be accomplished only by the continuous monitoring of several physiologic parameters and the judicious use of therapies to lower elevated ICP.
Physiologic monitoring
Arterial blood pressure. Noninvasive monitoring can be used, but an arterial catheter is preferred.
Heart rate, electrocardiogram (ECG), temperature, and pulse oximetry.
Central venous pressure or pulmonary artery catheter monitoring
Fluid balance (intake and output).
Laboratory evaluation. ABGs every 4 to 6 hours initially; electrolytes, glucose, and serum osmolality (if receiving mannitol) every 6 hours; hemoglobin/hematocrit, PT, PTT, platelets every 12 hours.
ICP monitoring.
Brain tissue O2 and/or cerebral microdialysis (if available)
Jugular venous O2 saturation or O2 content (if available)
Initial treatment
Blood pressure. Mean arterial blood pressure >80 mm Hg. No role for antihypertensive medications in TBI before brain CT and ICP monitoring performed. If mass effect, treat elevated ICP rather than elevated BP.
Oxygenation/Ventilation. Keep pO2 >60 torr. Aim for arterial oxygen saturation 100%. Hyperventilation ONLY with impending herniation. Target normocapnia (pCO2 34 to 40 torr).
Volume status. Keep central venous pressure 8 to 15 cm H2O and hematocrit ≤32%.
Glycemic control/Tonicity. Avoid dextrose-containing intravenous solutions for first 24 hours; avoid free water for extent of active therapy unless diabetes insipidus is present. Tight glucose control; avoid hyperglycemia.
Full access? Get Clinical Tree