Chapter 112
Transporting the Intensive Care Unit Patient 
The Airway in Transporting the ICU Patient
Certainly, having a stable airway in a mechanically ventilated patient is an advantage. However, whether the patient is ventilated via endotracheal or tracheotomy tube, ensuring that the tube is securely taped or attached and well positioned may be difficult. Transporting a patient inevitably requires several patient movements, on and off of stretchers, and even further shifting the patient several times if the transport is for additional testing. The security of the airway at all times is vital. A chest radiograph obtained immediately prior to transport gives the team confirmation of initial placement. Further confirmation of security/stability and placement should be performed after every movement. This comprises an assessment of the security and depth of the tube, as well as auscultation to ensure symmetric breath sounds ![]() (see Table 112.E1 for appropriate endotracheal tube sizes and depths). Adequate sedation during transport aims to prevent the patient from dislodging the tube or becoming agitated or combative (see Chapter 5). Continuous pulse oximetry should be maintained during transport to aid in assessment of the airway and adequate oxygenation during transport.
(see Table 112.E1 for appropriate endotracheal tube sizes and depths). Adequate sedation during transport aims to prevent the patient from dislodging the tube or becoming agitated or combative (see Chapter 5). Continuous pulse oximetry should be maintained during transport to aid in assessment of the airway and adequate oxygenation during transport.
Transporting the mechanically ventilated patient requires switching to a transport ventilator, the majority of which are conventional mechanical ventilators. The simplest transport device offers limited modes of support, whereas more complex devices offer a variety of ventilation modes, such as intermittent mandatory ventilation (IMV), assist control, or a combined assist/control mode with pressure or volume control (see Chapter 2). For patients on a conventional mechanical ventilator, a direct switch using the current ventilator settings can often be easily accomplished. However, switching from a more complex mode (e.g., high-frequency ventilation) to a transport ventilator may require a period of stabilization/transition (discussed later). An arterial blood gas (ABG) on the new ventilator at the current settings should be evaluated to address any ventilation needs prior to transport. For prolonged transports to other facilities, ABGs should be checked periodically, ideally every 1 to 2 hours if the patient appears clinically stable and more often if unstable. Ventilator adjustments should be performed gradually, avoiding sudden shifts, but providing the needed support. Any large ventilator changes to combat severe respiratory acidosis and hypercapnia should have blood gases monitored every 30 minutes until stable. Even appropriate blood gases after significant ventilator manipulation must be followed up, as overcorrection and subsequent hyperventilation may occur and be deleterious.
Blood Pressure Management in Transporting the ICU Patient
When patients are being picked up for transport at an outside facility by the accepting hospital’s team, all infusions are usually redone (recalculated, remixed, and placed on the transport team’s equipment) and set to run at the dose given by the primary care team. This process ensures consistency with the receiving institution’s concentrations and pumps, and it decreases the risk of medication errors by eliminating the need to employ unfamiliar rates or the inability to run certain setups on other pumps. Acute blood pressure shifts are frequent when transiently interrupting pressor infusions. It is essential to individually switch the infusions over to the transport set gradually and allow enough time to resolve hemodynamic changes, establish possibly new baselines, and adjust infusion rates.
TABLE 112.E1
Endotracheal Tube (ETT) Sizes and Depths
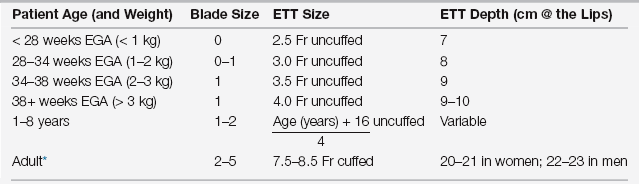
EGA, estimated gestational age.
∗Correct depth of tip of ETT for adults is 2.5 to 4.0 cm above main carina.

Full access? Get Clinical Tree


 ) mismatch, and minimize subsequent lung damage resulting from ventilator-induced trauma.
) mismatch, and minimize subsequent lung damage resulting from ventilator-induced trauma. mismatch and improves oxygenation and gas exchange, when combined with a high PEEP strategy to avoid dependent atelectasis. A short period of neuromuscular blockade has salutary effects on oxygenation, ventilation, and lung recruitment with a low risk for deleterious side effects. A low-tidal-volume ventilation strategy that enhances survival can usually be continued on transport.
mismatch and improves oxygenation and gas exchange, when combined with a high PEEP strategy to avoid dependent atelectasis. A short period of neuromuscular blockade has salutary effects on oxygenation, ventilation, and lung recruitment with a low risk for deleterious side effects. A low-tidal-volume ventilation strategy that enhances survival can usually be continued on transport.
