Key Clinical Questions
How are stroke and transient ischemic attack differentiated?
Who is eligible for IV recombinant tissue plasminogen activator?
What is the best cerebral imaging modality?
What is the optimal blood pressure in hospitalized patients with stroke?
What is the best antiplatelet therapy for secondary prevention of transient ischemic attack and stroke?
Should every patient be started on a statin?
Introduction
Stroke is the third leading cause of death in the United States. There are more than 700,000 strokes in the United States each year, resulting in more than 160,000 deaths annually, with 4.8 million stroke survivors alive today. Although there was a 60% decline in stroke mortality between 1968 and 1996, the rate of decline began to slow in the 1990s and has plateaued in several regions of the country. The incidence of stroke may actually be increasing. From 1988 to 1997, the age-adjusted hospitalization rate for stroke grew by 19%, and total stroke hospitalizations increased by 39%. In 2004, the cost of stroke in the United States was estimated at $53.6 billion (direct and indirect costs), with a mean lifetime cost estimated at $140,048. Stroke is also a leading cause of functional impairments, with 20% of survivors requiring institutional care after 3 months, and 15% to 30% being permanently disabled. Utility analyses show that a major stroke is viewed by more than half of those at risk as being worse than death.
Causes of Stroke
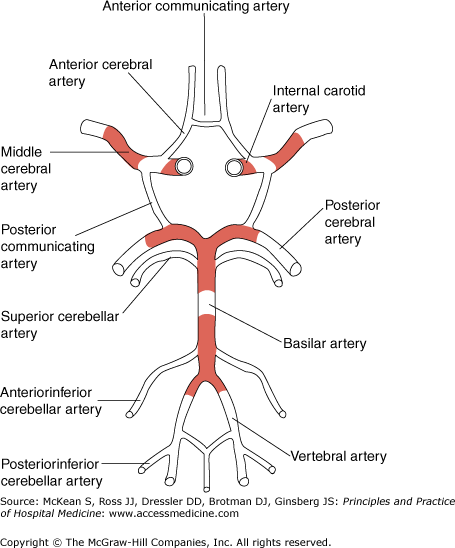
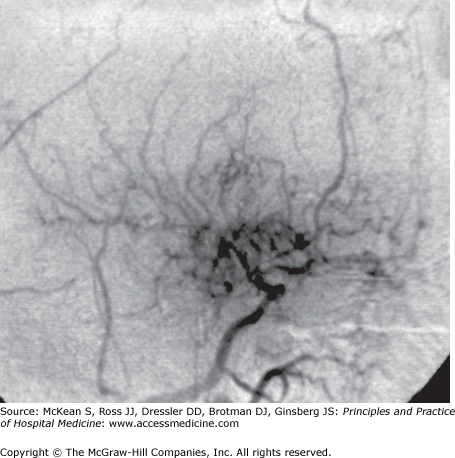
The most common cause of stroke is atherosclerosis of large and medium-size vessels of the neck and base of the brain (Figure 210-1). Risk factors for atherosclerosis include hypertension, diabetes, hyperlipidemia, cigarette smoking, and family history. Hypertension and diabetes also predispose to lacunae, which result from blockage of small perforating branches of the large cerebral arteries, with a predilection for the basal ganglia, thalamus, internal capsule, and pons. Patients with giant cell arteritis, systemic lupus erythematosus, and other vasculitides are at increased risk of stroke. Fibromuscular dysplasia is a cause of stroke in younger patients and is more common in women. Atrial fibrillation and valvular heart disease predispose to embolic stroke. Cocaine use predisposes to stroke for several reasons, including vasospasm, activating effects on platelets, and rupture of arteriovenous malformations and aneursyms in association with hypertension. IV drug users may develop embolic stroke from bacterial endocarditis. Stroke may also result from dissection of the carotid and/or vertebral arteries. Moyamoya syndrome results from bilateral narrowing of the distal internal carotids and adjacent anterior and middle cerebral arteries, with the development of fragile collateral vessels on angiography (Figure 210-2). It may be inherited as an autosomal recessive disorder or acquired in the setting of atherosclerosis, sickle cell disease, or basilar meningitis. Children present with ischemic stroke, whereas adults tend to develop intracranial hemorrhage. Hypercoagulability from genetic abnormalities in coagulation factors, leukemia, myeloproliferative disorders, antiphospholipid antibody syndrome, oral contraceptives, and sickle cell disease also predispose to stroke. Causes of stroke are summarized in Table 210-1.
Figure 210-2
Right carotid angiogram in moyamoya syndrome, lateral view. The middle cerebral artery and its branches are replaced by a diffuse capillary pattern that resembles a puff of smoke (moyamoya is Japanese and means “smoke” or “haze”). (Reproduced, with permission, from Greenberg DA, Aminoff MJ, Simon RP. Clinical Neurology. 5th ed. McGraw-Hill; 2002. Figure 9-7B.)
|
Clinical Presentation
Strokes and transient ischemic attacks (TIAs) present with the abrupt onset of neurologic deficits. In stroke, the duration of symptoms is longer than 24 hours. In TIA, symptoms resolve completely within 24 hours; in most patients with TIA, symptoms resolve within 30 minutes to 1 hour. However, if patients with clinical TIA have evidence of ischemia on magnetic resonance imaging (MRI) with diffusion-weighted sequences, the lesion is considered to be a stroke. The distinction between TIA and ischemic stroke has become less important in recent years, as measures for secondary prevention are similar in each group. Moreover, TIA is a robust short-term predictor of stroke: the 90-day stroke risk after TIA is as high as 10.5%, with the greatest risk in the first week.
Stroke may be produced by thrombosis, embolism, and hemorrhage. In embolic stroke, lesions are characteristically maximal at onset, whereas the symptoms of thrombotic stroke evolve over minutes to hours. In subarachnoid hemorrhage, patients may present with the sudden onset of “the worst headache of my life” or with a sudden extreme pressure sensation in the head or neck. For parenchymal hemorrhages, symptoms occur suddenly and progress over 30 minutes to 1 hour. Many conditions may mimic ischemic or hemorrhagic stroke (Table 210-2). It is important to determine anterior versus posterior circulation stroke to tailor imaging and intervention. In addition, posterior circulation strokes are more likely to produce complications related to altered consciousness. Large cerebellar strokes pose a risk of herniation and may require emergent neurosurgical decompression, especially if > 3 cm in size or if there is evidence of edema or hemorrhagic transformation. Recognition of progressive brainstem and cerebellar symptoms due to thrombosis of the basilar artery may allow for early intervention to prevent the devastating morbidity from infarct due to complete occlusion.
|
Lesions in the arterior cerebral artery are uncommon. Patients present with paralysis and sensory loss of the contralateral leg. Patients may have urinary urgency and incontinence from the failure to inhibit reflex bladder contractions.
The middle cerebral artery (MCA), the largest branch of the internal carotid artery, is the vessel most commonly affected in ischemic stroke. The clinical picture depends on the location of the damage (ie, whether all cortical branches are affected vs individual cortical branches) and whether the dominant or nondominant hemisphere is affected. Strokes affecting the superior division of the MCA lead to hemiparesis affecting the contralateral face, hand, and arm but sparing the leg, with accompanying sensory deficits; if the dominant hemisphere is involved, expressive (Broca) aphasia may develop, with loss of speech production but preserved speech comprehension. Inferior division MCA strokes may lead to contralateral homonymous hemianopia, hemineglect, loss of graphesthesia and stereognosis, and apraxias. Involvement of the dominant hemisphere also produces Wernicke, or receptive, aphasia, with speech consisting of fluent but meaningless babble. Lesions at the bifurcation of the MCA may lead to deficits in both superior and inferior vascular territories. Leg weakness may also ensue if the occlusion is proximal to the lenticulostriate branches of the MCA.
Internal carotid artery occlusion may be asymptomatic if collateral circulation is adequate, or it may produce strokes similar to middle cerebral artery syndromes if collateral circulation is poor. About 15% of cases of incipient carotid occlusion are heralded by episodes of transient monocular blindness (amaurosis fugax).
|
Posterior cerebral artery strokes produce contralateral homonymous hemianopia. If the vascular lesion is near the origin of the posterior cerebral artery in the midbrain, vertical gaze palsy, oculomotor (III) nerve palsy, and internuclear ophthalmoplegia may occur. If the dominant hemisphere is affected, patients may also have anomia, alexia without agraphia, or visual agnosia.
Strokes involving the vertebrobasilar circulation may lead to a variety of symptoms from brainstem ischemia, such as ipsilateral cranial nerve palsies with contralateral hemiplegia, ipsilateral cerebellar ataxia, nystagmus, vertigo, vomiting, dysphagia, dysarthria, Horner syndrome, and hiccup.
Horner syndrome is characterized by
Horner syndrome may result from sympathetic damage at any of the following locations:
Horner syndrome may thus result from either anterior or posterior (vertebrobasilar) cerebrovascular disease. If accompanied by vertigo and ataxia, it suggests cerebellar or medullary stroke from a vertebral artery lesion. |
Lacunar infarcts occur from degenerative changes in small penetrating arteries deep in the brain from hypertension. They are often clinically silent. When symptomatic, they may have an acute or subacute onset and may produce distinctive syndromes, such as pure motor hemiparesis (the most common type of lacunar infarct), pure sensory loss, dysarthria/clumsy hand syndrome, and ataxic hemiparesis, with incoordination out of proportion to motor weakness.
|
Assessment
Areas of special interest on general examination include vital signs (hypertension, irregular pulse); funduscopic examination, which may reveal retinal emboli (Hollenhorst crystals) in carotid disease; presence of carotid pulses or bruits; temporal arteries, which may be nodular, thickened, or pulseless in giant cell arteritis; and the cardiac examination, for evidence of atrial fibrillation, cardiomegaly, and valvular disease. Blood cultures should be obtained in febrile patients to exclude endocarditis.
The neurologic examination attempts to identify the site of the lesion and the likely culprit vessel. Certain findings are helpful in localizing a stroke to either the anterior circulation (the internal carotid artery and its major branches, the anterior cerebral, middle cerebral, and anterior choroidal arteries) or the posterior circulation (the vertebral arteries and basilar artery, their cerebellar branches, and their termination in the posterior cerebral arteries). The presence of aphasia indicates a lesion in the anterior circulation, rather than posterior, and makes lacunar infarction unlikely. Hemianopia also makes lacunar infarct unlikely. Although hemianopia may be present in either anterior or posterior circulation lesions, isolated hemianopia indicates a posterior cerebral artery lesion. Ocular palsies, nystagmus, and internuclear ophthalmoplegia indicate a posterior circulation lesion affecting the brainstem. Hemiparesis can be produced by a wide variety of lesions. However, hemiparesis of the face, hand, and arm, with relative sparing of the leg, suggests an MCA lesion. Hemiparesis that affects the face, hand, arm, and leg equally suggests a lesion in the internal carotid, stem of the MCA, a lacuna in the internal capsule or basal ganglia, or a brainstem stroke. Crossed hemiparesis (affecting the face and contralateral side of the body) suggests a brainstem lesion, as does a crossed sensory deficit. An isolated hemisensory deficit is likely due to a lacunar infarct.
The neurologic examination is discussed in detail in Chapter 207.