CHAPTER 43
Thoracic (T2-3) Ganglion Block
INTRODUCTION
The functional separation of the vagi (vagal nerves) and sympathetic trunks can be attributed to Estienne (1544),1 but it was Winslow who, in 1732,2 described the sympathetic trunk as the paravertebral chain. Many anatomists, including Michener and Auerbach, explored the sympathetic fibers and trunk. But as a functional component of the autonomic nervous system, the association had to wait until Langley and Dickerson in 1899.3
During the 20th century, many physicians (including Mandal,4 Kapppis,5 Brunn,6 Adriani,7 Loeser,8 Arnulf,9 Seabelund10) introduced their own variations on the best approach to the sympathetic trunk.5 However, they all involve variations of paravertebral techniques, the most recent being that described by Butler and Charlton in 2001.11
INDICATIONS
• The anterior approaches to the sympathetic trunk in the neck (stellate ganglion) are easily performed and are most commonly used; however, a posterior approach to the sympathetic trunk at the T2, T3 level provides the most reliable and consistent block of sympathetic activity to the upper extremity.12
• 20% of patients have sympathetic fibers that bypass the stellate ganglion called Kuntz fibers. These patients may not reliably achieve sympathetic blockade with a stellate ganglion block.
• Neurolytic techniques of the stellate ganglion have a significant risk of prolonged or permanent Horner syndrome, as well as damage to the phrenic and recurrent laryngeal nerves.
• The thoracic sympathetic block avoids these potential complications.
• The thoracic sympathetic block is indicated for all the same conditions as a stellate ganglion block.
INDICATIONS
Pain Syndromes
Common indications are as follows:
• Complex regional pain syndrome 1 and 2
• Herpes zoster (shingles)
• Postherpetic neuralgia (early)
• Postradiation arteritis
• Neuropathic pain associated with CNS pathology
• Paget disease
• Phantom limb pain
• Angina pectoris
The general indications for sympathetic block are shown in Table 43-1.
TABLE 43-1. Indications for Sympathetic Blocks
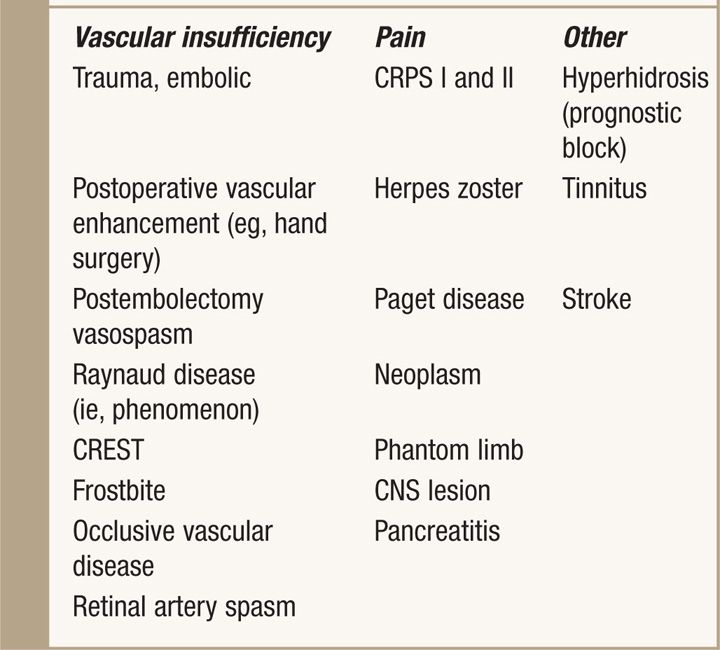
Vascular Insufficiency
Therapeutic applications for sympathetic block include:
• Raynaud disease
• Facial spasm
• Frost bite
• Microvascular pathology
• Embolic vascular disease
• Spasm of the ophthalmic artery
• Hyperhidrosis
• Buerger disease
• Stroke
• Vascular headaches
RELEVANT ANATOMY
The autonomic nervous system:
• The autonomic nervous system is divided into sympathetic and parasympathetic components, each made up of preganglionic and postganglionic neurons.
• Their axons travel along the anterior roots of the spinal nerve as white rami communicantes that project to the paravertebral sympathetic chain and then cephalad to synapse with postganglionic fibers in sympathetic ganglia.
• The stellate ganglia consist of a fusion of the first and inferior cervical ganglia.
• The inferior cervical ganglion is large (15-7 mm), tending to lie anterolateral to the head of the first rib.
• C7 and T1 ganglion cells form the stellate ganglia in about 82% of cases.
Thoracic ganglia
• Cell bodies of preganglionic sympathetic axons arise from cell bodies in the intermediolateral horn of the spinal cord between T1 and T9.
• Fibers to the upper extremity synapse mainly in the T2 ganglia; but some also synapse in the T3 ganglia, stellate (C7, T1), and middle cervical ganglia.
• Preganglionic axons that supply the heart have their cell bodies in the intermediolateral column between T1 and T5.
• Their preganglionic white rami synapse with postganglionic cell bodies in the paravertebral sympathetic chain between T2 and T5, and the middle cervical and stellate ganglia.
• Gray rami fibers pass from these ganglia to the heart and great vessels.
• The right and left pulmonary plexuses include both vagal and sympathetic postganglionic fibers.
• The thoracic sympathetic trunks lie on the necks of the ribs just lateral to their costovertebral articular processes and anterior to the intercostal vessels and nerves.
• Between T11 and T12, the sympathetic ganglia and chain lay anterolaterally on the side of the vertebral bodies.
• The T2 ganglion is anterior to the medial portion of the neck of the rib, but ganglia between T3 and T6 are located anterior to the heads of their corresponding ribs.
• T7 through T10 ganglia are more laterally displaced to lie anterior to the costovertebral joints, while T11 and T12 ganglia are more anterior placed to lie on the vertebral bodies.
• Because the first 4 thoracic ganglia lie in front of the upper portion of the necks and heads of each rib compared to the lower thoracic ganglia, it is almost impossible to reach them by a paravertebral approach (Figure 43-1).
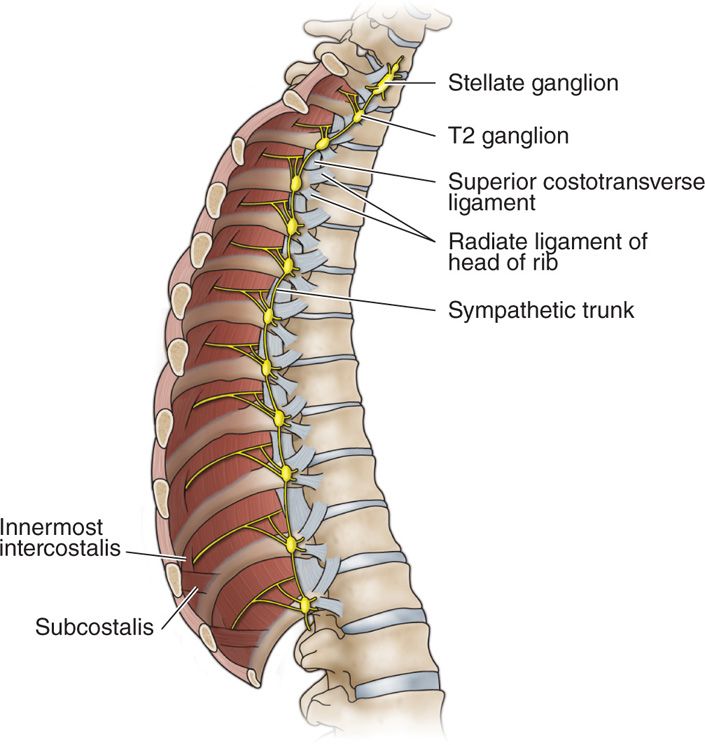
Figure 43-1. Sympathetic trunk on the right. Note that the positions of the first and second sympathetic ganglia are on the necks of their respective ribs whereas the third through eighth are on the heads of their ribs.
• Specific anatomy that has a bearing on radio frequency ablation (RFA) procedures is the anatomical disposition of the intercostal vessels. These lie posterior to the upper three ganglia. The lower thoracic ganglia lie inferior and in front of the intercostal vessels and nerves.
• The anterior primary rami of the segmental (spinal) nerves that form the intercostal and collateral intercostal nerves lie posterior and inferior to the ganglia except the upper T2-T4 ganglia to which their immediate posterior relation is the posterior primary ramus of the segment above.
• As the parietal pleura reflects from the ribs, it is separated from the ganglia by a small amount of adipose tissue.
BASIC CONCERNS AND CONTRAINDICATIONS
Many techniques have been described, but because of the risk of pneumothorax, the posterior approach is generally restricted to patients in whom fascial barriers or anatomic anomalies may prevent diffusion of local anesthetic from its anterior deposition at C6/C7 to the upper thoracic sympathetic trunk or when precise neurolytic procedures are planned.
Preoperative Considerations
When obtaining informed consent, the potential benefits, risks and complications, or any prolonged side effects, should also be clearly explained, but within the context of the expected response and its value to the patient and physician. It is essential to have IV access prior to the procedure. It may also be necessary to provide some form of sedation, depending on the circumstances and disposition of the patient, who may be a child.
Fluoroscopic Views
Anteroposterior to oblique views, and then cephalocaudal tilt for oblique approach: Follow two radiologic landmarks, specifically the tubercle of the costotransverse articulation and the costovertebral articulation (“head of the rib”) to achieve a comparatively straightforward approach to thoracic ganglia, in particular T2 and T3 (Figure 43-2). This procedure was described by Stanton-Hicks in 2001.12 The approach can be performed at any level of the sympathetic trunk with minimal risk of pneumothorax, in contrast with the incidence of pneumothorax associated with most paraspinous techniques.
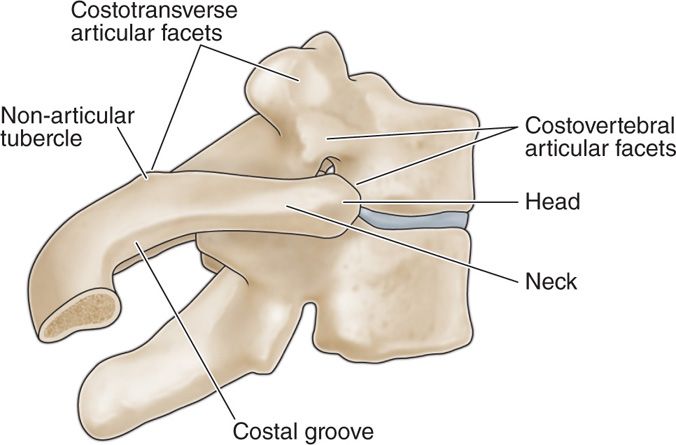
Figure 43-2. Articular facets on the transverse process and vertebral body for the corresponding rib are shown. Radiologic landmarks for the oblique technique require identification of the nonarticular eminence and head of the same rib. (Reprinted with permission of the Cleveland Clinic.)
Advantages of this approach are provided by the local anatomy itself:
• The parietal pleura forms a triangular space with the neck of the rib from which it reflects medially and anteriorly as it passes away from the angle of the rib.
• The prevalence of pneumothorax is less than 1% and generally occurs when bony landmarks are radiologically indistinct because of osteoporosis or other inflammatory processes.
• Almost all approaches to the sympathetic ganglia require either a direct posterior or slight oblique direction using a bony landmark such as a transverse process.
• Remember that these approaches were earlier undertaken without supportive imaging and required strict adherence to their bony landmarks for safe completion.
Equipment
• 10-cm 21-gauge spinal needle
• Image intensifier (C-arm x-ray machine)
• Telethermometer-infrared or thermistor
Medications
• Bupivacaine 0.75%
• Lidocaine 2.0%
TECHNIQUE FOR PARASANOUS APPROACH
Patient Preparation
The reason for performing a sympathetic block should be clearly explained to the patient. The expected duration and choice of local anesthetic will help the patient understand what they will be asked to observe during the course of the block. While sympathetic blocks may be diagnostic, prognostic, or therapeutic, the patient should be clearly informed of the purpose for the particular procedure they are to undergo.
• With the help of good imaging techniques, the needle must pass through the superior costotransverse ligament and is then advanced from 7 to 10 mm, at which point it lies within the thoracic cavity (Figure 43-3A, B).
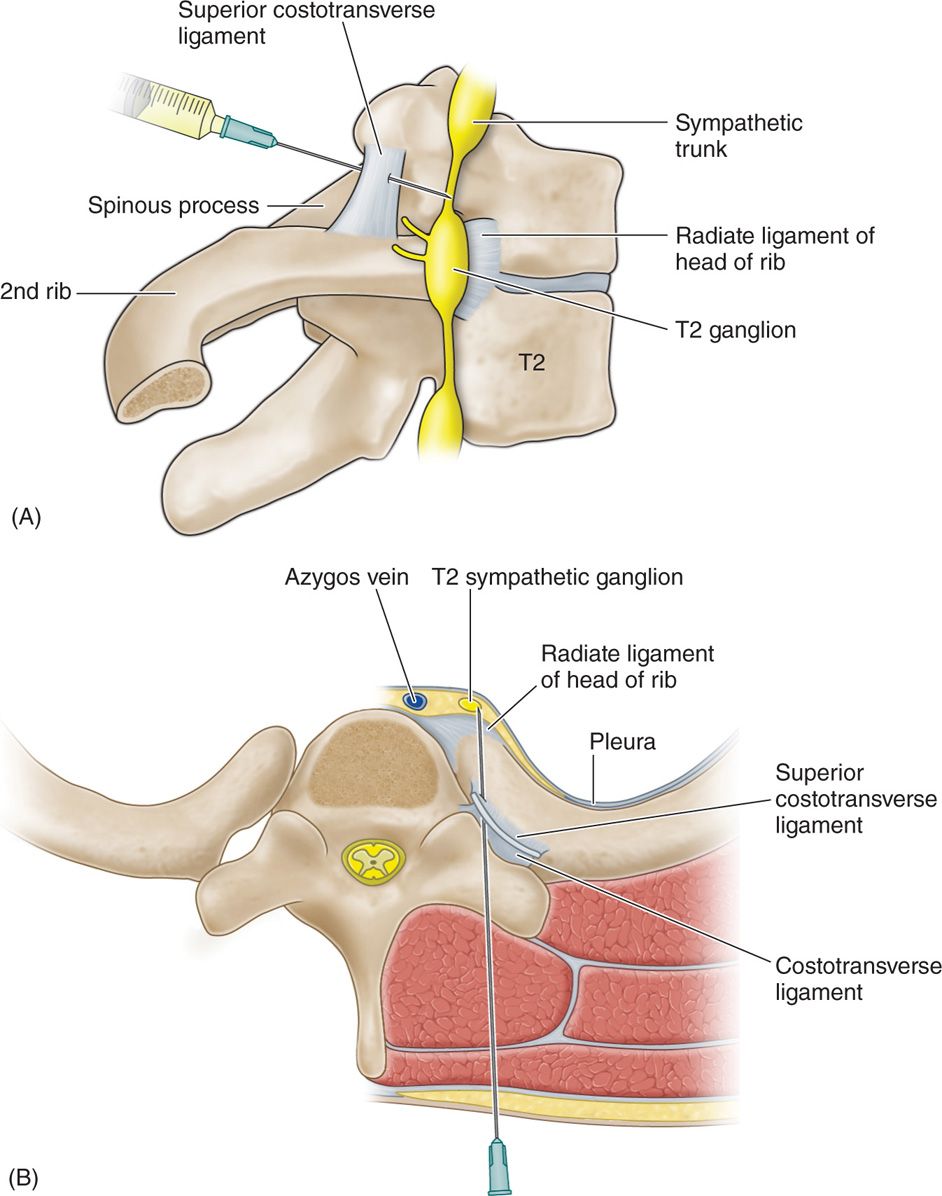
Figure 43-3. (A, B) The paraspinous approach to the sympathetic trunk. As the needle passes through the costotransverse ligament it will travel a further 1.5 cm before reaching the sympathetic trunk. (Note that a needle inserted at T3 will pass above the sympathetic ganglion, being “hidden” by the head of the rib. (Reproduced with permission of the Cleveland Clinic.)
• As described above, the relationship is such that the needle should contact the upper portion of the ganglion at T2 and T3.
• This approach is suitable for a local anesthetic block, but will also allow a radiofrequency lesion if a curve-tipped RF needle such as the Finch needle (Radionics Instruments, Inc, Burlington, MA) is used.
• This technique applies in particular to radiofrequency lesions. Even with a curved needle, unless the exposed tip is parallel to the ganglion surface, the generated heat will be insufficient to achieve a satisfactory lesion.
• However, it should be noted that the lower thoracic ganglia cannot be reached by this approach.
• Most techniques designed to access the sympathetic trunk within the thoracic region carry a risk of pneumothorax.
• Nevertheless, a good understanding of the anatomy, strict adherence to the technique, and good imagining techniques with fluoroscopy or CT scan can minimize the incidence of pneumothorax.
INTERCOSTAL OBLIQUE APPROACH TO THE THORACIC SYMPATHETIC GANGLIA
A thorough knowledge of the thoracic costovertebral anatomy is necessary. This approach relies on two radiologic landmarks:
• The tubercle of the rib (costotransverse articulation)
• The head of the rib
Ribs and Their Articulations
• As can be seen in Figure 43-2, the principal parts of the ribs are the head, neck, tubercle (articular eminence and nonarticular eminence), and curved body of the shaft.
• The costal groove contains intercostal vessels and nerves. The costal articulations should be noted.
• These, together with the tubercle and head of the rib, comprise the radiological landmarks that are required by this technique.
• It should be observed that a line drawn from the tubercle to the head of each rib is almost parallel with the neck of the corresponding rib; that is, the line is drawn from the inferior surface of the tubercle to the antero-inferior surface of the costovertebral transverse articulation (head of rib), and will pass under the neck of the rib. This line will lie adjacent and lateral to the parietal pleura (see Figure 43-3B).
Positioning the Patient
• The patient must first be placed prone on a radiolucent table with a chest roll that allows the scapula to move laterally with the arm either supported on an arm-board, or allowed to hang dependant.
• Patients undergoing this procedure should be lightly sedated.
• Verbal contact with the patient must be maintained at all times.
• Temperature probes (thermistors) should be placed on corresponding thumb pads for continuous monitoring.
Technical Steps
Once the patient is in position, and sterile preparation and draping have been carried out, the image intensifier (x-ray C-arm) is then placed at a right angle to the spine, and over the center of the vertebra and costovertebral articulation representing the target ganglion. The view should be a true anteroposterior (AP) projection (Figure 43-4A-C). The C-arm is then rotated to an oblique position determined by the superimposition of the costotransverse nonarticular tubercle and the costovertebral articulation (head of the rib) (Figure 43-5B).
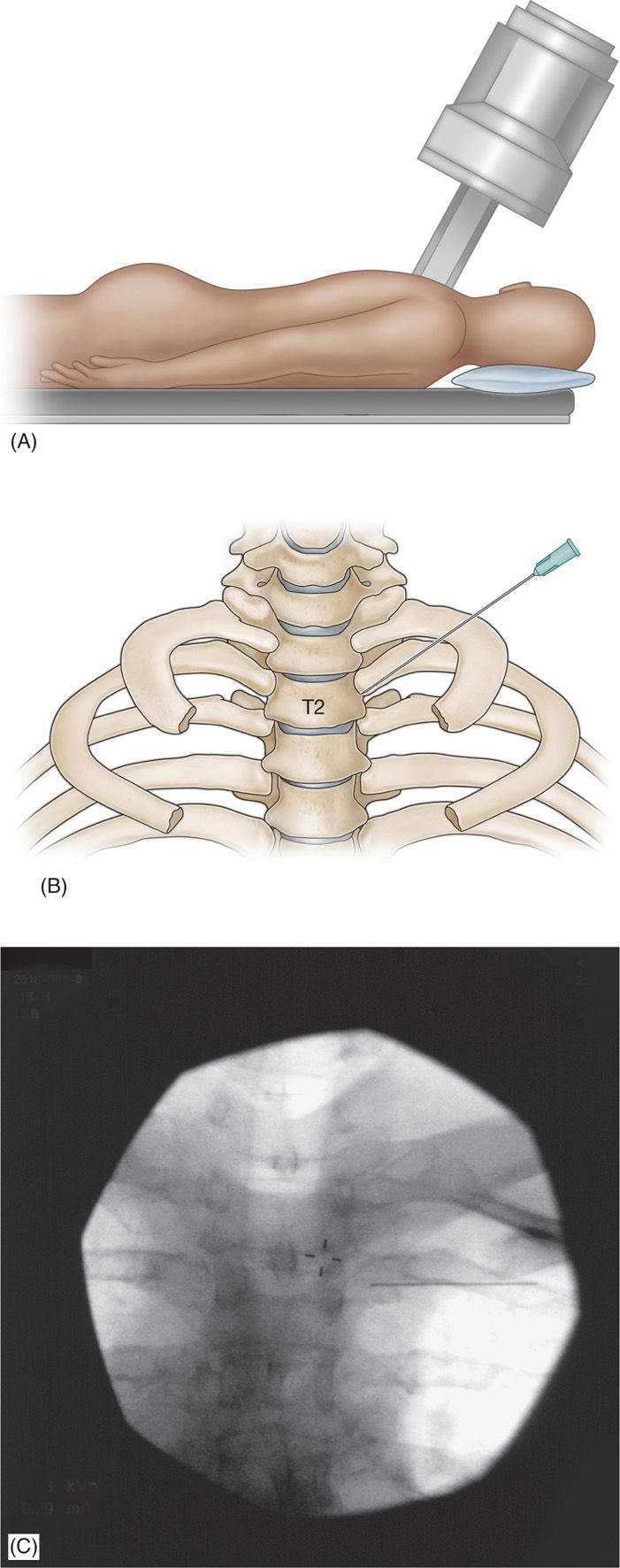
Figure 43-4. (A) Position of fluoroscopy arm (C-arm)—anteroposterior with cephalad tilt. (B) True anteroposterior projection showing the angle taken by the needle when the oblique technique is used. (C) X-ray showing needle position in PA projection.
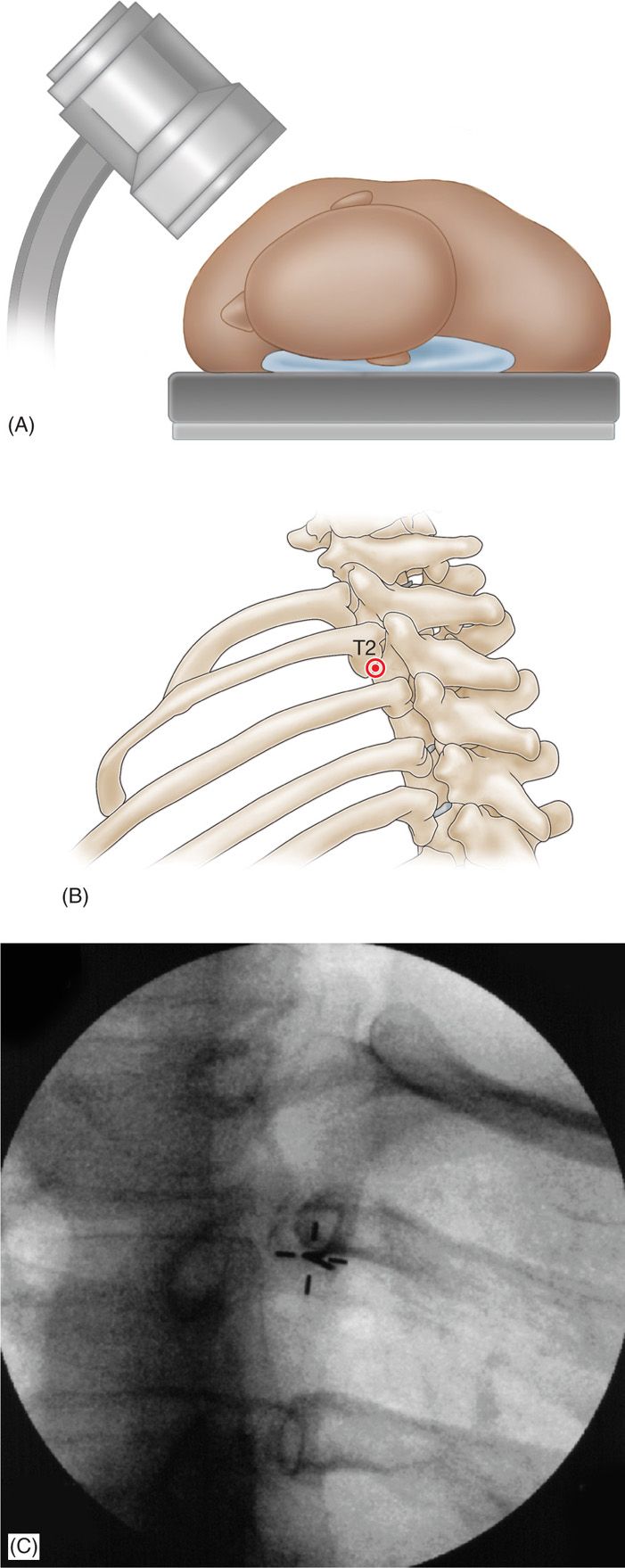
Figure 43-5. (A) “Gunsight” view of needle and target under the superimposed costotransverse and costovertebral articulations. (B) X-ray view (gunsight view) of needle in oblique transverse projection. (C) Depicting needle and target seen in oblique transverse projection.
• A C-arm with a laser sighting device will facilitate the procedure because the index can be placed precisely at the antero-inferior edge of the costovertebral articulation.
• This placement of the index simplifies the initial position taken and increases accuracy as the needle is advanced.
• Without such a device, the needle is inserted so that when seen “end-on” it appears as a dot (gun-sight side view) at the inferior surface of the superimposed tubercle and antero-inferior margin of the costovertebral articulation (Figure 43-5A-C).
• Great care should be taken to ensure this alignment, for it will allow accurate and safe needle passage to the target ganglion.
• The needle is advanced carefully, taking 1 or 2 AP views with the C-arm during insertion until it contacts the inferior outer edge of the rib.
• After passing underneath the rib, it is advanced in the thoracic cavity until it impacts the costovertebral articulation.
• A lateral projection will show the needle tip to be just anterior to the costovertebral articulation and above the vertebral foramen (Figure 43-6A, B).
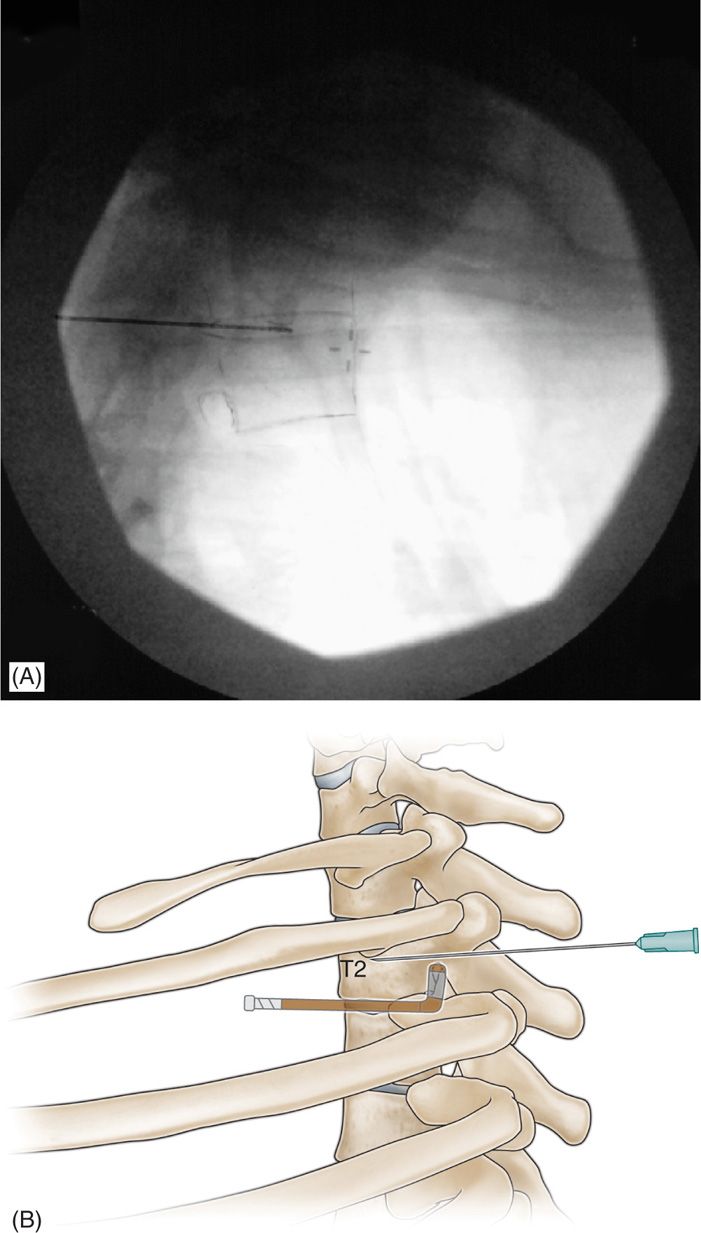
Figure 43-6. (A) Lateral projection of the fluoroscopy arm (C-arm) showing correct needle position at costovertebral articulation and so-called “hockey stick” that identifies the landmarks, foramen, costovertebral articulation and disc. (B) Anatomy of the final needle position seen from a lateral view.
• The image seen in this view can be likened to a “hockey stick,” where the handle of the hockey stick is the disc and the blade is the vertebral foramen.
• A small amount (0.1 mL) of water-soluble contrast should outline part of the capsule of the costovertebral articulation in the lateral view and in an AP projection, it will appear to follow the undersurface of the rib (neck) at an angle of 5 to 7 degrees.
• If a curved (Finch) RFA needle is used, it should be passed through a 16-gauge intravenous cannula that is first introduced to the rib.
• The RFA needle is then rotated until it passes under the rib, at which time it is rotated back again so that the convex surface of the distal curve of the needle faces the parietal pleura.
• As with a regular 10-cm 21-gauge needle, the RFA needle is introduced in the same manner described above until it reaches the costovertebral articulation.
• To achieve a sympathetic block, a small amount of 0.75% bupivacaine or ropivacaine (0.25-0.5 mL) is injected at T2 or T3 depending on the indication.
• Alternatively 0.25 to 0.5 mL of 2% lidocaine will achieve complete interruption of sympathetic fibers to the upper extremity.
Neurolytic Procedure
• Neurolysis using 10% to 16% phenol in a volume of 0.25 to 0.5 mL will achieve a prolonged block of each ganglion and in addition, those sympathetic fibers that are destined for the upper extremity.
• RFA of individual ganglia can be undertaken after first ensuring that no motor or sensory stimulation occurs.
• Motor stimulation should be undertaken at 2 Hz and 1.5 V and sensory stimulation at 50 Hz and 0.8 V.
• In the absence of sensory and/or motor effects, RFA can be carried out at a temperature of 80°C for 80 seconds.
• This can be repeated with rotation of the needle through 180 degrees.
Postprocedure Follow-Up
• Determine duration of procedural effect—whether it helped or not.
• May need a chest x-ray if there is any possibility of pneumothorax.
• Assess the sympatholysis to plan the further management.
Potential Complications and Pitfalls
• Procedure related general complications like infection, bleeding
• Pneumothorax—patient should be monitored for late onset of pneumothorax
• Epidural and/or intrathecal injection, and neurological deficit
• Intercostal neuritis, very rare
CLINICAL PEARL
• The oblique intercostal approach is a technique used in lieu of stellate ganglion block that is more reliable in achieving complete interruption of sympathetic elements to the upper extremity.

Full access? Get Clinical Tree







