Deppu Ushakumari and Ashish Sinha
1. Which of the following is not a characteristic feature of asthma?
A. Chronic inflammatory changes in the submucosa of the airways
B. Airway hyper responsiveness
C. Reversible expiratory airflow obstruction
D. Elastase deficiency in the airways
2. A 55-year-old male presented to you with a pulmonary function test report, which shows an increase of FEV1 percent predicted of more than 12%, and an increase in FEV1 of greater than 0.2 L in response to bronchodilators. Which characteristic of his respiratory illness is depicted here?
A. Bronchial asthma—acute bronchodilator responsiveness
B. Chronic obstructive pulmonary disease (COPD)—variability in airflow obstruction
C. COPD—acute bronchodilator responsiveness
D. All the above are correct
3. Which of the following techniques is associated with a lower complication rate related to bronchospasm in the asthmatic population?
A. Regional anesthesia
B. General anesthesia—laryngeal mask airway (LMA)
C. General anesthesia—endotracheal tube (ETT)
D. Combined general and neuraxial anesthesia
4. A 22-year-old patient with a history of moderate persistent asthma on medium-dose inhaled corticosteroids and long-acting inhaled β-agonist presents for an emergency appendectomy. On clinical examination, he is actively wheezing, but maintaining an oxygen saturation of 99% on room air. Which of the following statements about this clinical scenario is most appropriate?
A. Presence of wheezing on physical examination indicates that he is having a severe attack of asthma
B. Volatile anesthetics cause bronchodilation through catecholamine-independent mechanisms
C. Increased airway resistance that occurs intraoperatively is usually due to acute exacerbation of asthma
D. A laryngeal mask airway (LMA) is more stimulating to the airway than an endotracheal tube, and should be avoided in asthmatics
5. During the above case, the end-tidal sevoflurane concentration reads 3.5, but the anesthesia ventilator is alarming because of high peak airway pressures. Which of the following is the most likely cause?
A. Acute bronchospasm
B. Anaphylactic reaction to intravenous muscle relaxant that you just administered
C. Mechanical causes of obstruction
D. Inadequate depth of anesthesia
6. At the end of the above case, the surgeon requests you to extubate the patient fully awake because he found extensive intestinal adhesions and is afraid of retained gastric contents in the stomach. Which of the following will be your most likely plan of action?
A. Insert an orogastric tube, empty the stomach as much as you can, and proceed with a deep extubation to avoid bronchospasm
B. Administer intravenous lidocaine to decrease the likelihood of airway stimulation and wait till the patient is fully awake before extubation
C. Shut off the inhalational agent and use intravenous propofol to avoid transitioning through a rocky stage-2 wake up
D. Transition to a laryngeal mask airway (LMA) under sevoflurane anesthesia and let the patient wake up with an LMA
7. Which of the following is true regarding administering general anesthesia to a chronic obstructive pulmonary disease (COPD) patient?
A. Nitrous oxide + opioid technique is ideal
B. Use large tidal volumes
C. Use lower breathing rates to permit more exhalation time
D. Correct the hypercapnia intraoperatively to help extubate early
8. Anesthetic considerations for a patient with severe pulmonary hypertension include all the following, except
A. Right heart catheterization is the gold standard for diagnosis
B. Mortality in pregnant patients undergoing vaginal delivery is very small as opposed to cesarean section
C. Minimize tachycardia, hypoxemia, and hypercapnia during anesthetic management
D. Cardiac output from a failing right ventricle depends on filling pressure from venous return and pulmonary pressure
9. Which of the following is not a part of the “STOP BANG” screening questionnaire for obstructive sleep apnea (OSA)?
A. Snoring
B. Observed apnea
C. Exercise tolerance
D. High blood pressure
10. Risk factors associated with increased perioperative morbidity and mortality in thoracic surgery patients include all the following, except
A. Extent of lung resection
B. Age older than 70 years
C. Experience of the operating surgeon
D. Male sex
11. The following is not necessarily a part of prethoracotomy respiratory assessment
A. Pulmonary capillary wedge pressure >18 mm Hg
B. Predicted postoperative FEV1 >40%
C. VO2 max >15 mL/kg/min
D. Predicted postoperative diffusing capacity for carbon monoxide (DLCO) >40%
12. Which of the following is one of the benefits regarding cessation of smoking 12 to 24 hours prior to surgery?
A. Shift of oxyhemoglobin dissociation curve to the right
B. Improvement in mucociliary transport
C. Decrease in sputum production
D. Improved small-airway function
13. In surgical cases requiring lung isolation
A. Measurement of tracheal width from a posteroanterior chest radiograph is of no use in selecting the size of a double-lumen tube (DLT)
B. More frequent use of left-sided DLT is based on the anatomy of tracheobronchial tree
C. Uniform ventilation to all lobes is most likely achieved by a right-sided DLT because it has a ventilation slot in the bronchial tube
D. Fiber–optic confirmation of correct DLT placement is not required if you have good clinical confirmation
14. A 59-year-old lady is intubated with a 37 left-sided double-lumen tube (DLT) for wedge resection of left lower lobe nodule. After intubation, you inflate the bronchial cuff and ventilate the left lung through the bronchial lumen without any difficulty. Then you proceed to inflate the tracheal cuff and ventilate through the tracheal lumen. You notice a very high resistance to air flow. Which of the following events is most unlikely with the said clinical picture?
A. Left DLT too deep with the tracheal outlet into the left main-stem bronchus
B. Left DLT displaced with the bronchial cuff herniated at carina
C. Left DLT entered the right bronchus with the tracheal outlet in the right main stem
D. DLT too far out with the bronchial lumen sitting just above the carina
15. What would you do if you have the following situation with a bronchial blocker for left lung surgery?
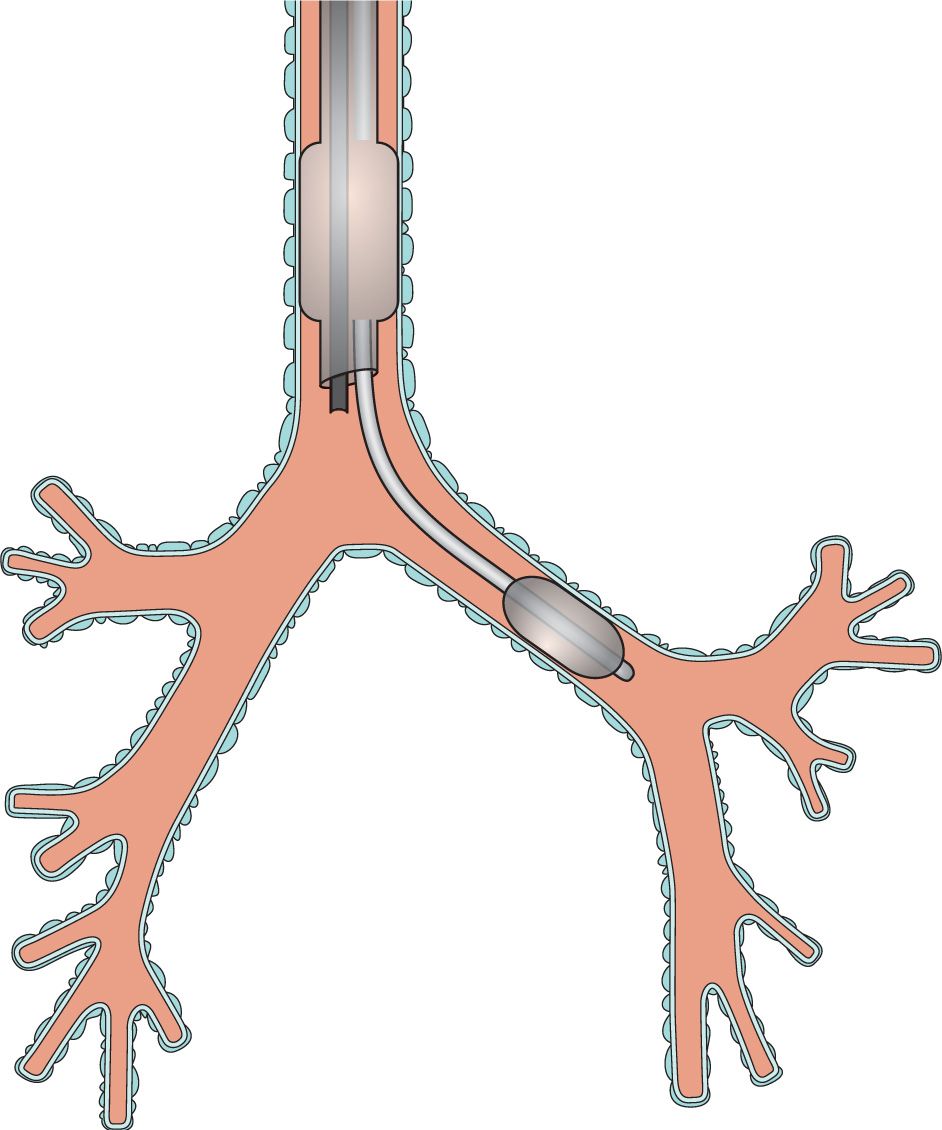
Figure 12-1.
A. Appropriate positioning for this surgery
B. Withdraw the bronchial blocker a couple of centimeters
C. Insert the bronchial blocker a few centimeters farther down
D. Remove the bronchial blocker and reinsert it into the left side
16. In which of the following situations is applying continuous positive-airway pressure (CPAP) to the nondependent lung most ideal for improving oxygenation?
A. Bronchopleural fistula
B. Open lobectomy
C. Massive pulmonary hemorrhage
D. Sleeve resection
17. Which of the following statements is false regarding ventilation/perfusion relationship in a lateral decubitus position during spontaneous ventilation?
A. The ventilation/perfusion matching is preserved
B. Contraction of dependent hemi diaphragm is more efficient
C. Dependent lung is on a more favorable part of the compliance curve
D. The lower lung receives less ventilation and more perfusion than the upper lung
18. In an open pneumothorax, the major effect of mediastinal shift is to
A. Decrease the contribution of dependent lung to the tidal volume
B. Move air to and fro between the dependent and the nondependent lung
C. Decrease the perfusion to the dependent lung
D. Compress the big veins and decrease cardiac preload
19. Factors known to inhibit hypoxic pulmonary vasoconstriction (HPV) and thus worsen the alveolar–arterial oxygen gradient include all of the following, except
A. Hypocapnia
B. Nitroglycerin
C. Hypercapnia
D. Pulmonary infection
20. A 64-year-old female is undergoing a left video-assisted thoracoscopy for a suspicious pulmonary nodule. Immediately after positioning the patient laterally, which of the following alarms indicates a malposition of the double-lumen tube (DLT)?
A. High CO2 alarm
B. Low O2 alarm
C. Low tidal volume alarm
D. Unable to drive bellows alarm
21. A bronchial blocker is useful in all of the following clinical situations, except
A. Patient to be left intubated post operatively
B. Anatomical abnormality precluding the placement of a double-lumen tube (DLT)
C. Tamponading bronchial bleeding in adult patients
D. To attain better collapse of the nondependent lung
22. Which of the following statements about lung resection surgery is false?
A. Mortality rate for pneumonectomy is 5% to 7%
B. Mortality rate for lobectomy is 2% to 3%
C. Mortality is higher for left-sided pneumonectomy
D. Most postoperative deaths result from cardiac issues
23. Regarding lung resection surgery, which of the following statements is false?
A. Perioperative arrhythmias are common
B. Supraventricular tachycardias (SVTs) are thought to result from surgical manipulation or distension of the right atrium
C. Incidence of arrhythmia decreases with age due to the ageing of cardiac conduction system
D. Postoperative hypoxemia and acidosis due to atelectasis and shallow breathing are common
24. Which of the following has the least effect on hypoxic pulmonary vasoconstriction (HPV)?
A. Nitrous oxide |
|
B. Desflurane | end tidal 5.5% |
C. Sevoflurane | end tidal 2.5% |
D. Isoflurane | end tidal 1.5% |
25. Which of the following statements is not true regarding “lower lung syndrome”?
A. It is caused by excessive fluid administration in a lateral decubitus position
B. It increases intrapulmonary shunting
C. It is gravity-dependent transudation of fluid into the dependent lung
D. It is due to volutrauma caused during one-lung ventilation
26. The first step recommended to improve oxygenation if a patient is exhibiting drop in oxygen saturation during one-lung ventilation is
A. Apply continuous positive-airway pressure (CPAP) to the collapsed lung
B. Apply positive end–expiratory pressure (PEEP) to the dependent lung
C. Periodic inflation of the collapsed lung
D. Continuous inflation of oxygen into collapsed lung
27. During apneic oxygenation,
A. Adequate oxygenation can be maintained only for short periods of time
B. Arterial PCO2 rises 3 to 4 mm Hg in the first minute
C. Arterial PCO2 rises 1 to 2 mm Hg each subsequent minute after the first minute
D. Progressive respiratory acidosis limits the use of this technique to 10 to 20 minutes in most patients
28. A 68-year-old male patient with a lung nodule underwent a right upper lobectomy. On postoperative day 4, the patient develops a sudden large air leak from the chest tube associated with increasing pneumothorax and partial lung collapse. The most likely cause is
A. Bronchopleural fistula on the right from necrosis of suture line
B. Bronchopleural fistula on the right from inadequate surgical closure of the bronchial stump
C. Atelectasis causing shifting of the mediastinum to the left
D. A normal finding
29. An 80-year-old female underwent a left lower lobectomy. In the ICU on postoperative day 2, she develops hemoptysis. The vital signs are stable, but on the chest X-ray a homogenous density is seen in the left lower lung area. After subsequent bronchoscopy, the left upper lobar orifice is closed. The most likely diagnosis is
A. Acute herniation of the heart into the left lower lobe area
B. It is a normal finding and the homogenous opacity is due to accumulation of fluid in the left lower lobe area
C. Torsion of the left upper lobe as the left upper lobe expanded to occupy the left hemithorax
D. Reexpansion edema of the left upper lobe
30. A 45-year-old recent immigrant from Vietnam is admitted to the emergency department with massive hemoptysis (>600 mL in the last 24 hours). You are called to evaluate the patient for a possible bronchial artery embolization or a rigid bronchoscopy. In your discussion with the patient, which of the following statements is not appropriate about his clinical condition?
A. Operative mortality exceeds 20%
B. It can be done as a semi-elective procedure, and there is no need to do it emergently
C. The most common cause of death is asphyxia secondary to blood in the airway
D. Medical management has a lower mortality rate than operative management
31. An 81-year-old chronic smoker, with a history of 60 pack year smoking, is admitted with progressive dyspnea and a huge right-sided pulmonary cyst. The cyst is compressing her remaining right lung, and she is brought to the OR for an emergency pulmonary cystectomy. Which of the following is right regarding anesthetic management of this patient?
A. The greatest risk of rupture of the cavity is during preoxygenation just prior to induction
B. These cavities allow to and fro movement of air and have a very low chance to progressively enlarge
C. Maintenance of spontaneous ventilation is desirable until a double-lumen tube (DLT) is in place
D. Assisted ventilation is not necessary immediately after induction and can be harmful
32. A 66-year-old patient with a history of severe tracheal stenosis is presenting for a tracheal resection. The most unlikely clinical finding is
A. Progressive dyspnea
B. Wheezing evident on exertion
C. Dyspnea worse on sitting up and leaning forward
D. Patient may have a history of blunt/penetrating tracheal trauma
33. In the anesthetic management of the above patient, which of the following statements is correct?
A. Flow–volume loops aid the clinician in evaluating the severity of the lesion
B. Right radial artery blood pressure monitoring is preferred over the left side for lower tracheal resection
C. Slow-inhalation induction is not advisable and a rapid-sequence induction should be used
D. Early extubation is not advisable at the end of the procedure for risk of rupturing the suture lines
34. Complications associated with mediastinoscopy include all the following, except
A. Vagally mediated reflex bradycardia
B. Cerebral ischemia
C. Pneumothorax
D. Thoracic duct injury
35. Anesthetic considerations for bronchoalveolar lavage include all the following, except
A. It is performed for patients who make excess quantities of surfactant and fail to clear it
B. It is performed under general anesthesia with lung isolation
C. It is usually performed in the supine position
D. It involves positioning the patient in a lateral position to aid active suctioning of the lavage fluid
36. Considerations for lung transplantation include all the following, except
A. Cor pulmonale does not necessarily require combined heart–lung transplantation
B. Patients with diminished left-ventricular function can be transplanted as long as they have normal right-ventricular function
C. Patients with Eisenmenger syndrome require combined heart–lung transplantation
D. Organ selection is based on size and ABO compatibility
37. After a double-lung transplantation
A. Loss of lymphatic drainage predisposes to pulmonary edema
B. Respiratory pattern changes to a slow deep respiration
C. Cough reflex is abolished above the carina
D. Hypoxic pulmonary vasoconstriction is abolished
38. Anesthetic considerations for esophageal surgery include
A. Very low risk of pulmonary aspiration
B. Mandatory pulmonary artery catheter monitoring
C. Diaphragmatic retractors interfering with cardiac function
D. Always performed with a double-lumen tube (DLT)
39. Lung-volume-reduction surgery (LVRS)
A. Has been demonstrated to have very good efficacy by the National Emphysema Treatment Trial (NETT)
B. Necessitates limiting of peak inspiratory pressure to 30 cm H2O following intubation
C. A prolonged inspiratory time is recommended for facilitating exposure of the surgical segments
D. Patients have a better outcome if kept intubated at the end of the surgery
40. Which of the following flow–volume loops will be expected in a child with variable extrathoracic obstruction?
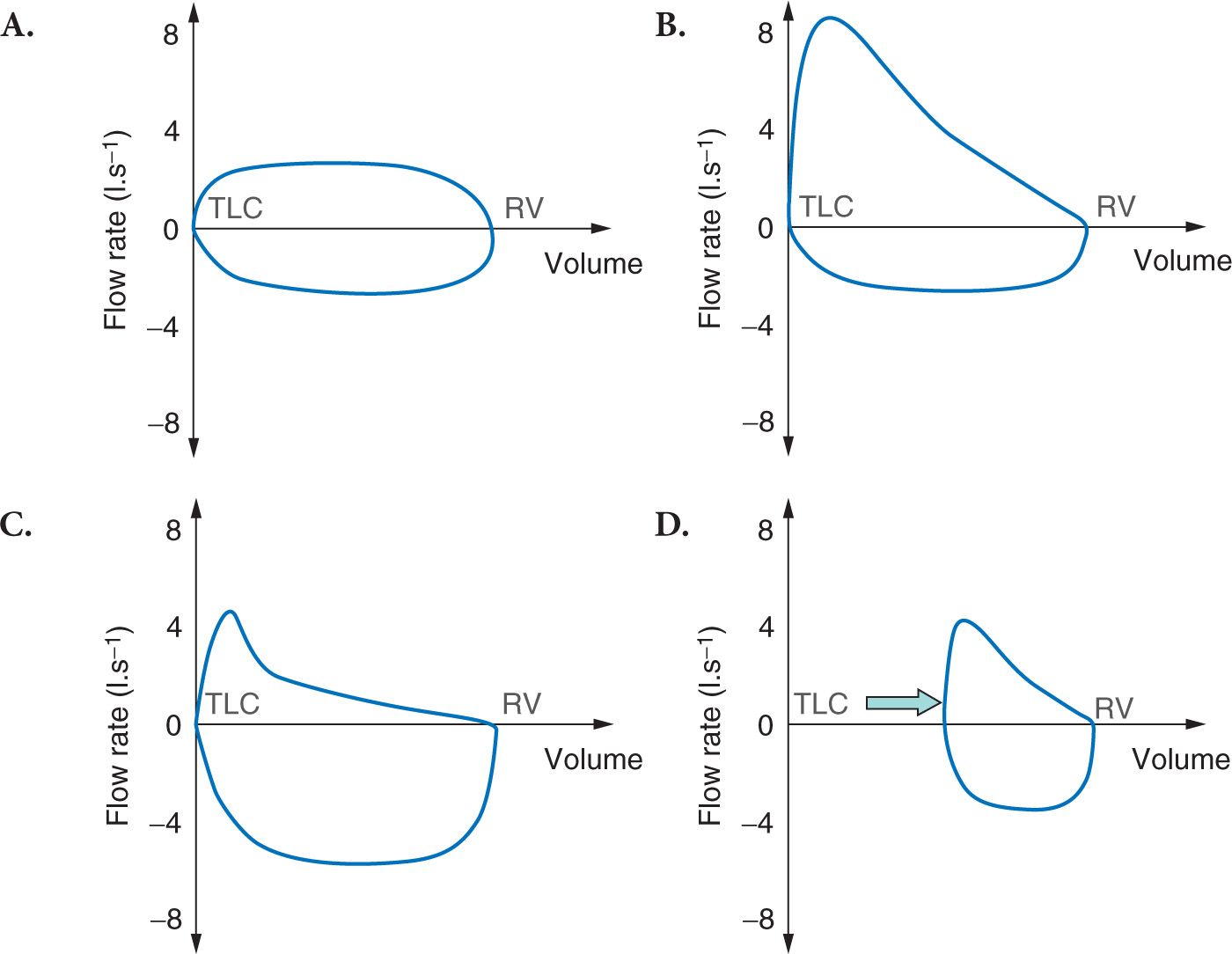
Figure 12-2.
41. A 12-year-old boy with suspected lymphoma presents to you for a lymph node biopsy. When you go to visit the patient, you notice that he has venous engorgement and edema of the head, neck, and arms. He refuses to lie down, and is tachycardiac and tachypneic. The preferred management for this boy would be
A. Safest thing will be to secure the airway immediately by using rapid-sequence induction
B. Preferably biopsy the lymph node under local anesthesia so that the patient can be sent for radiotherapy immediately after a tissue diagnosis
C. Empiric treatment with steroids and surgery under general anesthesia only after the airway compromise is alleviated
D. Get a chest X-ray and rule out mediastinal compression prior to any active management

Full access? Get Clinical Tree






