Box 8.1 Upper Limb Support and Splintage
Box 8.1 Upper Limb Support and Splintage- fractures, dislocations and other painful conditions of the shoulder and clavicle
- fractures and other injuries of the forearm, wrist and hand including support of plaster casts
- painful conditions of the elbow and support of casts on the elbow
- Wear the sling outside clothes
- Remove the sling at night and support the injured part on pillows
- Remember the importance of maintaining shoulder and hand mobility
THE SHOULDER AND UPPER ARM
Fracture of the Clavicle
The clavicle provides the only skeletal continuity between the upper limb and trunk. It is occasionally broken by direct trauma but usually breaks in the middle two-thirds as a result of transmitted violence from a fall on to the upper limb. Damage to adjacent neurovascular structures is very rare except with posterior sternoclavicular dislocation. In adults, fractures cause well-localised symptoms with obvious deformity and tenderness.
Children:
greenstick fractures are common after childhood falls. There may be little deformity and remarkably good movement of the arm and shoulder girdle. Alternatively, the child may refuse to use the whole arm on the affected side and thus mimic a pulled elbow (→ p. 117).
XR
An anteroposterior (AP) radiograph confirms the diagnosis.
TX
The weight of the arm should be supported in a broad arm sling. Figure-of-eight bandages, applied to achieve reduction, are usually more painful and do not succeed in their objective. Most displaced fractures settle to produce an acceptable cosmetic result. Prescribe appropriate analgesia and refer the patient to the next fracture clinic. Very painful, comminuted fractures may rarely require initial inpatient care, as do the occasionally occurring compound fractures.
Sternoclavicular Joint Disruption
This is rare and is the result of considerable indirect violence applied to the shoulder. Usually anterior dislocation with prominent bone is seen; posterior displacement is even rarer and may involve damage to major blood vessels, the trachea or the oesophagus.
XR
Radiological confirmation is difficult. A CT scan may be helpful.
TX
This can be a major injury with potentially serious consequences. Orthopaedic advice should be sought.
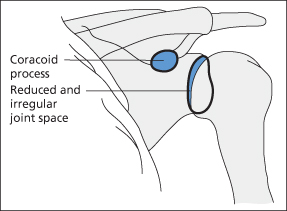
Acromioclavicular Joint Disruption
This is much more common than the sternoclavicular joint disruption. The outer end of the clavicle is elevated at its articulation with the acromion. The weak fibres of the acromioclavicular joint are readily ruptured. The joint’s normal stability is maintained by the conoid and trapezoid ligaments, binding the outer fifth of the clavicle down to the coracoid process of the scapula. It is the complete or partial rupture of these strong ligaments that results in an acromioclavicular dislocation or subluxation. Direct downward pressure will reduce the deformity rather painfully and only transiently. Shoulder movements are restricted because of pain.
XR
Radiographic confirmation, if required, is obtained by taking a wide-angled erect AP film to show both acromioclavicular joints with the patient holding weights in both hands. Slight subluxation may occur normally.
TX
The raised outer end of the clavicle is accepted as a minor disability by most patients. Reduction is very difficult to maintain by closed methods and internal fixation, although successful, may leave an ugly prominent scar. A sling and analgesia are provided until the pain has settled. The shoulder will remain weak for some months. Manual workers may notice a very slight but permanent loss of power in the affected limb.
Supraspinatus Tendinitis/Subacromial Bursitis
These two conditions are very difficult to separate. Both are caused by a combination of soft-tissue degeneration and a modest increase in activity. The patient presents with an injured shoulder often following an event such as lifting. Symptoms may occur suddenly or be more gradual in onset. Movements are restricted, particularly abduction and forward flexion. Classically, there is a painful arc from about 20° to 90° of abduction, but initially the pain may be intense and affect all movements. There may be specific tenderness in the supraspinatus fossa laterally.
XR
Radiographs sometimes show calcification within the tendon, near its attachment to the joint capsule.
TX
A sling and non-steroidal anti-inflammatory drugs (NSAIDS) should be prescribed. In severe cases, a short course of oral steroids can give dramatic relief. Patients should be reviewed within a week, when physiotherapy and orthopaedic referral may be considered. Surgical decompression may help in chronic cases.
Rotator Cuff Injury
The glenohumeral joint is stabilised by four muscles that surround it – the rotator cuff:
The rotator cuff muscles may be acutely injured or chronically inflamed or both. This causes pain with shoulder movements, sometimes of the painful arc type. There may be a tender area anteriorly. The tendons of all the rotator cuff muscles may rupture or degenerate in a similar manner to the supraspinatus tendon (→ above).
TX
Analgesia, together with rest in a sling, is required for a few days. Early physiotherapy is essential. The condition can be very slow to settle (up to 2 years), especially in older patients and in those with an acute onset.
Rupture of the Long Head of Biceps
This is caused by a combination of tendon degeneration and powerful elbow flexion. The patient presents with the sudden appearance of a painless lump reminiscent of Popeye’s biceps.
TX
This is usually symptomatic, but a specialist opinion should be sought at the next fracture clinic.
Dislocation of the Shoulder Joint
This may occur after trivial injury in a predisposed individual or follow major violence to the shoulder girdle and be associated with other bone and soft-tissue injuries.
A full examination is mandatory to exclude associated injuries and distal neurovascular complications.
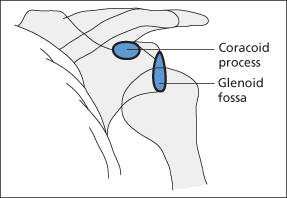
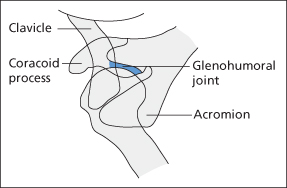
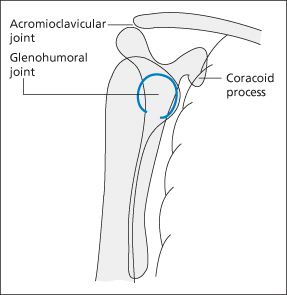
The dislocation is usually anterior and easily detected clinically and radiologically (→ Figure 8.1). Posterior dislocation is rarer and associated with the muscle contraction that occurs during fits and electric shocks. Inferior dislocation (“luxatio erecta”) is very rare – the patient presents with the arm erect. A fracture of the greater tuberosity or neck of the humerus may accompany a dislocation.
XR
Radiographs must be taken before reduction is attempted. Lateral radiographs are difficult to interpret; modified axial views are more useful. Figures 8.2 and 8.3 demonstrate the normal appearances of the shoulder joint on lateral and apical radiographs.
TX
The patient will need early parenteral analgesia. Reduction can be achieved without general anaesthetic by using one of a number of techniques to overcome muscle spasm. Prior analgesia helps but large amounts should not be necessary if the technique is good. The method of sedation will depend largely on the experience of the staff involved (→ p. 15). Many methods of reduction can be equally successful; a simple technique for anterior and posterior dislocations is described in Box 8.2.
 Box 8.2 Reduction of a Dislocated Shoulder
Box 8.2 Reduction of a Dislocated Shoulder- Explain the procedure to the patient
- Ensure that adequate sedation and analgesia are achieved and appropriate resuscitation facilities are available
- Gently hold the wrist on the dislocated side in both hands. Countertraction, if required, may be applied by a second person supporting the patient with a towel sling around the shoulder or by the operator’s (unshod) toes in the axilla. The latter (Hippocratic) method requires the operator to stand on a low stool
- Slowly (over a minute or two) abduct the arm out to 90°, keeping the elbow extended. As the arm is abducting, rotate it externally (i.e. so that the palm is facing upwards)
- Apply firm, constant traction along the patient’s abducted, rotated arm. The shoulder joint is approaching its most unstable position. Gentle, uninterrupted traction with reassurance to maintain muscle relaxation is the key to success. Do not use excessive force because it may damage the axillary neurovascular structures. By slightly varying the angle of pull and the axial rotation of the arm, the joint will usually relocate within about 5 min with minimal patient discomfort
Inferior dislocations usually reduce easily; the arm is gently brought down to a partially abducted position and then treated as an anterior dislocation.
Fracture of the greater tuberosity may accompany a dislocated shoulder. It will usually relocate easily as the shoulder dislocation is reduced.
Patients with a dislocation and a co-existing fracture of the neck of the humerus need immediate orthopaedic referral as do patients with a dislocation that is more than 24 h old.
After reduction, the arm is immobilised in a sling and a body bandage is applied to prevent abduction and external rotation. Radiographs are then repeated to confirm reduction and the arm is again examined to exclude neurovascular damage. The patient is then referred to the next fracture clinic with instructions to keep the wrist and hand mobile. Physiotherapy and gradual mobilisation will be necessary at a later date, possibly followed by surgical repair of the lax shoulder joint capsule if there has been recurrent dislocation.
Brachial Plexus Injury
These injuries are caused by sudden traction on the arm (e.g. a window cleaner grasping the window ledge as the ladder slips) or by direct violence to the shoulder region (e.g. a motor cyclist struck from in front by an oncoming vehicle). They may also be seen in patients who have sustained prolonged pressure on the axilla while under the influence of alcohol. Proximal injuries may avulse the nerve roots from the spinal cord. Differing amounts of damage occur. There may be any of the following:
- Complete section – neuroptmesis
- Axonal damage – axonoptmesis
- Failure of transmission only – neuropraxia
- A combination of the above.
Neurological examination determines the areas involved. The presence of Horner’s syndrome indicates preganglionic damage. A histamine test on anaesthetised skin distinguishes lesions proximal (triple response) and distal (no response) to the dorsal root ganglion.
XR
Radiological examination should include the shoulder, cervical spine and thoracic outlet.
TX
Early specialist referral will be required. Axonal regeneration down intact sheaths occurs at a rate of about 1 mm/day (or 1 inch/month). Surgical repair is rarely attempted and then mainly for distal lesions. No regeneration or repair is possible if part of the plexus has been avulsed from the spinal cord.
Fracture of the Scapula
Fractures of the scapula are relatively uncommon and usually the result of direct trauma. Significant force is required to break the scapula and so accompanying injuries must be excluded. Any part of the bone may be fractured, including the body, spine, neck, acromion process and coracoid process. Local pain and tenderness are the main clinical features; shoulder movements may be relatively intact.
XR
Fractures of the scapula are often missed on radiographs. An oblique view of the shoulder (to show the scapula more clearly) may be requested in cases of doubt.
TX
Displacement of a fracture of the spine or blade is rarely significant and management is conservative. The patient should be given a broad arm sling and analgesia, and then referred to the next fracture clinic. The scapula has an excellent blood supply and usually heals very well.
Fracture of the Humoral Neck
This can occur at all ages, but is particularly common in elderly people. It is usually an isolated injury, caused by a low-speed impact. Displacement is common and may be gross, but is usually unimportant.
A full examination should be made to exclude other injury, particularly at the wrist. The axillary nerve may be damaged, causing deltoid paralysis and an area of anaesthesia over the outer aspect of the shoulder. The joint may sublux inferiorly because of this deltoid paralysis. The nerve will recover spontaneously over a period of a few weeks. Bruising is often very extensive and may extend down to the mid-forearm over the first few days. The patient should be warned that this rather frightening but harmless phenomenon might occur.
XR
An AP radiograph may be sufficient, but if shoulder dislocation is suspected an axial view will be required. In children, it is necessary to distinguish a greenstick fracture, with buckled cortex, from the normal epiphyseal line.
TX
A sling, analgesics and reassurance are all that are required initially. Fracture clinic referral is arranged; physiotherapy should follow.
Frozen Shoulder
Adhesive capsulitis of the shoulder joint is most commonly seen in older patients. It may be spontaneous or follow the disuse associated with any type of upper limb injury. Early mobilisation after injury will help to prevent its development (e.g. for patients with Colles’ fractures remove the sling every few hours so that the arm can be moved behind the back and the neck). Patients with established disease and no recent history of trauma may present to the ED. Cervical and thoracic outlet problems must be excluded. The patient often complains of pain at the deltoid insertion but is actually tender over the anterior capsule. Abduction and internal rotation are particularly restricted.
XR
Radiographs may show an area of calcification in the shoulder joint capsule.
TX
This condition may be very slow (up to 2 years) to resolve spontaneously. The other shoulder may be affected just as the first is recovering. Physiotherapy is the mainstay of treatment. Steroid injection – particularly into calcified areas of the capsule – and NSAIDs may be helpful. Manipulation under anaesthesia may sometimes be needed.
Thoracic Outlet Obstruction
The neurovascular outflow from the thorax and spine to the upper limb is constrained by a narrow-based triangle above the first rib. The lower parts of the brachial plexus and the subclavian artery may be compressed here if the shoulders are depressed by heavy backpacks or unaccustomed lifting. Symptoms are more likely if the brachial plexus is post-fixed (i.e. arises from the spinal cord more caudally than usual) or if there is a cervical rib. A tumour at the apex of the lung can spread upwards to involve the lower part of the brachial plexus.
The patient complains of a gradual onset of diffuse shoulder girdle pain, made worse by carrying shopping bags, etc. Symptoms can be reproduced by pulling down on the arm with the patient standing. The radial pulse may be obliterated if the arm is abducted to 90° and the patient turns his or her head to the opposite side. There may be weakness of the small muscles of the hand and paraesthesia in the hand extending up the inner border of the arm.
XR
Radiographs are taken of the cervical spine, thoracic inlet and chest.
TX
Always seek advice about management. If more sinister causes have been excluded, slow recovery usually occurs if traction on the shoulder can be avoided. Physiotherapy may help. Resection of the first rib may be necessary in severe cases.
Referred Pain at the Shoulder
Diaphragmatic irritation may produce shoulder-tip pain. Causes include cholecystitis, splenic injury, subphrenic abscess and pleurisy. Cardiac pain may present initially with a generalised ache in the shoulder joint.
Fracture of the Humoral Shaft
This fracture is unstable and painful and thus requires immediate splintage. The mechanism of injury and the possibility of damage elsewhere should always be considered. If little force was involved, pathological fracture is a possibility. The radial nerve is often damaged, but rarely divided, as it winds around the humoral shaft in the spiral groove; ensure ability to extend the wrist and fingers. The radial pulse should also be checked because brachial artery injury may sometimes occur.
XR
Radiographs should include the shoulder and elbow joints.
TX
Provide support and analgesia. Orthopaedic referral is indicated. Internal fixation is usually undertaken but external splintage with a U-slab of plaster and a collar and cuff is an alternative.
THE ELBOW
The elbow may be injured by a direct blow or by transmitted forces. In children, the constantly changing epiphyses make the interpretation of radiographs rather difficult (→ Box 8.3 and Figure 8.5).
 Box 8.3 Elbow Radiographs in Children
Box 8.3 Elbow Radiographs in Children| C | 2: capitellum – present by age 2 years |
| R | 4: radial head – appears at 3–5 years of age |
| I | 6: internal or medial epicondyle – present by age 6 years |
| T | 8: trochlea – appears at age 7–9 years |
| O | 10: olecranon – appears at age 9–11 years |
| E | 12: external or lateral epicondyle – present by age 11–14 years |
- The epiphyses of the capitellum, trochlea and lateral epicondyle become one centre in the early teenage years
- All the epiphyses fuse in teenage, usually a year or two later in boys than in girls
- Comparative views of the other elbow, taken at the same angle, are occasionally helpful but should not be requested unless absolutely necessary (and then usually after discussion with a radiologist)

Full access? Get Clinical Tree