Chapter 41 The Traumatized Airway
I Defining the Problem
A The Clinical Challenge
2 Early Hospital Care of the Traumatized Patient
Trauma and burn patients frequently undergo surgery that is not related to their acute resuscitation but is required during the first few days of their hospital stay. Burn débridement and grafting, fracture fixation, complex wound revision and repair, and other procedures are often required hours or days after the patient has been stabilized and more acute, life-threatening problems have been controlled. Decision making in this setting is easier with respect to airway management because the decision to intubate is driven by the need for surgery and anesthetic management; however, careful preoperative assessment remains essential. In addition to the usual comorbidities that can make airway management difficult, trauma patients often have other complicating factors, such as direct airway injury, pulmonary injury with rapid oxyhemoglobin desaturation, persistently tenuous hemodynamic status, or cerebral injury with elevated intracranial pressure (ICP). Patients with significant total body surface area burns, crush injuries, or spinal cord injuries develop acetylcholine receptor upregulation, with its attendant risk of hyperkalemia if succinylcholine is administered.1 Although classic teaching posits that this vulnerability to succinylcholine-induced hyperkalemia begins on postinjury day 7, some effect is seen as early as day 3.2 This combination of considerations—specifically unresolved or unrecognized traumatic injuries, the potential for hyperkalemia, and the patient’s preexisting comorbidities—can make airway management in this intermediate-term window anything but routine. A careful approach, including detailed consideration of possible difficult airway management protocols and relevant comorbidities, is essential.
B The Decision to Intubate
Answers to three fundamental questions inform the decision to undertake emergency intubation:
1. Is there a failure to maintain or protect the airway?
2. Is there a failure of oxygenation or ventilation?
3. Is there a need for intubation based on the anticipated clinical course?
The gag reflex is much less reliable than phonation and swallowing, and it is absent in up to 25% of the normal adult population.3 The presence of a gag reflex does not equate to airway protection, nor does its absence indicate a need to intubate. The presence or absence of the gag reflex is better thought of as a neurologic evaluation (i.e., cranial nerves IX and X) rather than as part of an airway evaluation. The Glasgow Coma Scale is a better tool for predicting intubation.4
Most trauma patients can maintain and protect their airways and exhibit adequate or correctable oxygenation and ventilation. For them, it is the anticipated clinical course that guides the decision to intubate. This is the most sophisticated and most important of the decisions facing the airway manager or trauma captain. A patient may appear stable at the time of evaluation, but deterioration can be predicted as a natural course of the injuries. For example, the patient with burns from a closed-space fire with significant inhalation of superheated air (see Chapter 44) may present with a somewhat hoarse voice or a simple cough but has an otherwise patent airway. Failing to recognize the likelihood of progressive obstruction of the airway, which has been subjected to toxic and thermal insults, and to intervene in a timely fashion can lead to disaster. Although the patient may not meet the criteria for emergency intubation related to airway maintenance and protection, oxygenation, or ventilation, the likelihood of deterioration is alone sufficient to warrant airway intervention.5 It is the predictability of the deterioration that determines the decision to intubate. Alternatively, the upper airway can be examined by fiberoptic laryngoscopy, informing the airway manager of the stability or fragility of airway patency. Similarly, the patient with a crushed pelvis, open femur fracture, and hypotension is inevitably intubated, even though there is no immediate threat to airway patency or oxygenation. The need for advanced imaging, aggressive pain control, and operative repair of obvious injuries dictates that the patient be intubated early and in a more controlled fashion than trying to manage a chaotic intubation from behind the computed tomography (CT) scanner.
II Anatomy of the Airway: Trauma Considerations
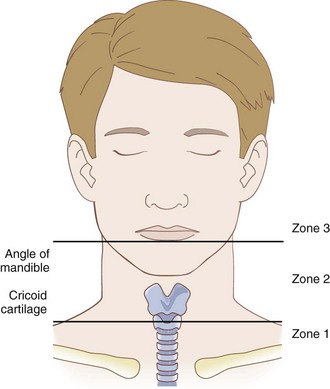
Although airway anatomy is discussed in Chapter 1, the following is a brief description of elements to consider in the trauma setting. The airway begins at the nares or lips and ends with the terminal bronchioles and alveoli of the lungs. The upper airway consists of the oral and nasal cavities and the pharynx, which provide a conduit for the movement of gases to the larynx, through the glottis, and into the trachea. The nasopharynx, oropharynx, and hypopharynx (Fig. 41-1) form a continuous space that conducts air from the outside world to the glottic aperture. The nasopharynx is protected anteriorly and laterally by the maxillary bones, the nasal bones, and nasal cartilage. Direct injury to the face, particularly from an impact with an object of high mass, high velocity, and low surface area (e.g., baseball bat), can collapse the maxillary structures into the nasopharynx and cause extensive hemorrhage, threatening the airway and complicating attempts to manage it. Similarly, the oropharynx is protected by the maxillary bones, alveolar ridges, and mandible but is subject to the same sort of intrusive injuries. Blows to the face producing Le Fort I, II, or III fractures (Fig. 41-2) can simultaneously threaten the airway and complicate airway management.
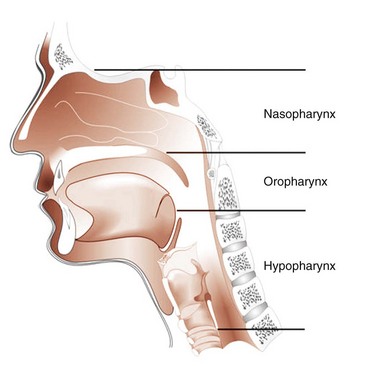
Figure 41-1 Airway anatomy.
(From Redden RJ: Anatomic considerations in anesthesia. In Hagberg CA, editor: Handbook of difficult airway management, Philadelphia, 2000, Churchill Livingstone, p 11.)
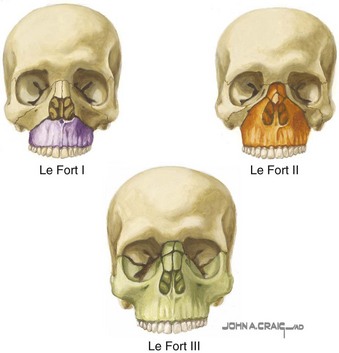
Figure 41-2 Le Fort classification.
(From the Netter Collection of Medical Illustrations: Website. Available at http://www.netterimages.com [accessed February 2012]. Copyright Elsevier Inc.; all rights reserved.)
The larynx and trachea are essentially subcutaneous structures in the anterior neck. The larynx is separated from the skin only by subcutaneous fat and the anterior cervical fascia. The thyroid notch, cricothyroid membrane, and cricoid cartilage can be easily palpated to provide the critical landmarks for surgical access to the airway (see Chapter 31). The airway is mobile in the neck but is fairly firmly anchored by the strap muscles and cervical fascia. Tracheal deviation as a result of pneumothorax or hemothorax may occur in patients who are severely compromised.6 Tracheal deviation is not helpful as a sign of pneumothorax because it usually occurs only when the pneumothorax is at an advanced state and easily identifiable by auscultation. Tracheal deviation can result from disruption of the neck anatomy caused by hemorrhage or extensive subcutaneous emphysema. It is also seen with chronic scarring, such as that related to previous radiotherapy. In any case, palpation of the trachea and larynx is a valuable exercise in the event that surgical airway management becomes necessary. It also can establish the position of the airway in the neck, even if orotracheal intubation is contemplated. Orotracheal intubation can be extraordinarily difficult or impossible when the trachea or larynx is displaced laterally.
III Specific Clinical Considerations in Trauma
A Direct Airway Trauma
1 Penetrating Neck Trauma
Penetrating neck injuries range in scope from stab or other puncture wounds to major lacerations due to both low-velocity (e.g., BBs, pellets) and high-velocity (e.g., crossbows, firearms) projectile injury. The consequences of these various mechanisms can vary drastically. The overall mortality rate due to penetrating neck injuries is 2% to 6%, with a significantly lower mortality rate for low-velocity injuries.7–9 The patient with a stab wound to the neck usually has identifiable anatomy and can undergo a planned airway evaluation and early intubation under controlled circumstances. Patients with high-velocity injuries often have significant vascular and hollow-structure injuries, and anatomic distortion can make airway management challenging.10 These injuries mandate urgent airway management, but the approach is confounded by the myriad injuries caused by the missile.11
For the purposes of classification of penetrating injury, the neck is divided into three zones (Fig. 41-3). Zone 1 extends from the clavicles inferiorly to the level of the cricoid cartilage. Zone 2 extends from the cricoid cartilage to a line drawn through the angles of the mandible, and zone 3 is the area above the angles of the mandible. This classification is most useful for low-velocity penetration, such as from a stab or long-distance birdshot, but it has also been applied to high-velocity injuries, such as rifle wounds.10 These zones were designated because of their unique anatomic characteristics.12 Zone 1 is dominated by the major vascular structures at the root of the neck, specifically the carotid arteries, internal jugular veins, subclavian arteries and veins, and innominate arteries and veins. The airway at this level is relatively inaccessible except by tracheotomy. Zone 1 injuries are relatively uncommon (<10% of penetrating neck injuries) but are often associated with major vascular injuries or injuries to the dome of the lung.13 Patients with zone 1 injuries often require emergency airway management because of direct airway compromise by hemorrhage or the anticipated clinical course predicted by the profound shock that typically develops. There is little literature to guide the selection of airway management techniques for zone 1 penetrating injuries. Most information is limited to small case series of subsets of larger series that are dominated by zone 2 injuries. The approach to airway management is dictated more by the nature of the threat to the airway than by the location of the inciting wound. The overall approach to airway management in penetrating neck injuries is outlined subsequently.
Zone 2 is the most common location for penetrating neck injuries, accounting for most reported cases.14 Zone 2 injuries require emergency airway intervention in approximately one third of the cases, with a large proportion of the remainder undergoing subsequent intubation related to evaluation or surgical repair. The area of concern in zone 2 extends from the anterior margins of the paravertebral muscles bilaterally. In this area, major vascular structures (e.g., common carotid arteries, internal jugular veins) and their associated sympathetic ganglia and the hypopharynx, esophagus, larynx, and trachea are all at risk. The most common cause of airway compromise in zone 2 injuries is external distortion by hemorrhage related to vascular injuries or direct injuries to the airway.15
The best approach is to consider two specific issues. The first is whether there is evidence of a direct injury to an air-containing structure in the neck. Subcutaneous air indicates injury to an air-filled structure in the neck,16 such as the airway (including the hypopharynx or pharynx) or the esophagus. In severe cases, particularly patients with injury to both vascular and air-filled structures, airway obstruction can occur rapidly, requiring emergency cricothyrotomy.17 In less threatening cases, it is virtually impossible to tell whether the esophagus or airway is involved, and early direct or fiberoptic examination of the airway is indicated. Sedation and topical anesthesia allows the operator to determine the severity and location of any airway injury. Preparation with a small to moderate-size endotracheal tube (ETT) (e.g., 6.0- to 7.0-mm inside diameter) mounted on the scope before initiating endoscopy facilitates prompt intubation if the injury is found to be significant. If the scope has been placed successfully distal to the injury, the patient can be gently intubated over the flexible fiberoptic bronchoscope (FFB), because it is best to secure the airway distal to the injury. This at least ensures that the patient is safe until he or she can be transported to the OR for further evaluation by an otolaryngologist or general surgeon. Although tracheostomy is often necessary, in these cases, temporary oral endotracheal intubation over an FFB ensures airway control and minimizes the subsequent leakage of air into the tissues, facilitating later repair.16 If no airway injury is identified and there is no evidence of increase in the subcutaneous emphysema in the neck during spontaneous or assisted ventilation, the injury can be presumed to be esophageal.18 If, however, circumstances change and subcutaneous emphysema begins to increase, even slightly, intubation is recommended since development of large amounts of subcutaneous emphysema can distort airway anatomy such that subsequent intubation or surgical airway management becomes difficult or impossible. As with all penetrating neck injuries, early intubation, even in patients who do not appear to immediately require it, is the most prudent course.
The second issue is whether there is evidence of significant vascular injury to the neck. All penetrating neck wounds have some external bleeding, although it can be surprisingly modest. The issue with respect to airway management is whether injury has occurred to any of the major vascular structures in the neck (e.g., carotid arteries, jugular veins). A hematoma of any size, external hemorrhage, or any evidence of displacement of the airway structures can serve as evidence of direct vascular injury. As soon as it has been established that direct vascular injury has occurred, active airway management should be undertaken.19,20 Most of these patients present early in the course of their injuries, when anatomy is preserved and orotracheal intubation is likely to be relatively easy to achieve. Waiting to determine whether the hematoma is expanding is perilous, because most of the hemorrhage into the neck occurs into the deep tissue planes, distorting and displacing the airway without external evidence until a crisis occurs. The time-honored dictum that hematomas of the neck should be observed to see whether they are expanding is not rational, and any evidence of direct vascular injury to the neck is sufficient justification for intubation. Early intubation can proceed using a rapid-sequence intubation (RSI) technique if a careful examination for difficult airway attributes fails to identify problems and there is a sound rescue strategy planned in the event of intubation failure.21 Early intervention allows the operator to intubate in a controlled fashion rather than scrambling to secure an emergency airway later in the patient’s course, when airway obstruction is imminent or has already occurred.
The third option is to proceed directly with a planned surgical cricothyrotomy. This requires that the airway be identifiable with clear landmarks to permit a surgical approach. Local anesthetic infiltration and direct transcricothyroid puncture for instillation of local anesthesia into the airway are likely to make the procedure easier to perform (see Chapter 31).
In all cases of penetrating neck trauma, early consultation with an otolaryngologist or general surgeon is essential. Initially innocuous injuries may lead to catastrophic consequences for the patient if not identified and managed early.22 Early airway intervention permits controlled resuscitation and prevents major morbidities related to penetrating neck injury, such as airway compromise with resultant hypoxia or anoxia.
2 Blunt Neck Trauma
1. Identification of swelling, hemorrhage, or subcutaneous emphysema
2. Evaluation for tenderness (if possible) of the neck, particularly the airway structures
3. Evaluation of the anatomy of the upper airway for direct airway injury and for the anatomic landmarks that are important if a surgical airway must be placed (see Chapter 31).
Because subcutaneous emphysema may be occult, it requires careful palpation. Extensive ecchymosis suggests blunt vascular injury with free hemorrhage (which is usually venous) or formation of a pseudoaneurysm. Extensive ecchymosis or extensive swelling strongly suggests impending airway compromise, and urgent airway intervention is advisable.23 Infrequently, direct blunt neck trauma can cause laryngeal fracture or tracheal transsection. The latter is often rapidly fatal, but patients may arrive in the trauma resuscitation area alive because of incomplete transsection.24 In these cases, there is usually subcutaneous air, often accompanied by swelling, and pain elicited by palpation of the anterior airway. Although a trial of BMV may be tempting, it is likely to exacerbate the subcutaneous emphysema and accelerate the patient’s deterioration. When such an injury is identified, the best approach is prompt transfer to the OR for surgical exploration of the anterior neck and establishment of the airway by tracheostomy distal to the transsection. Often, however, airway management must be undertaken before the surgery, and careful awake fiberoptic intubation over a small FFB after inhalational induction may be the least of all evils. If the airway must be secured in the ED, for example, before transportation to a level I trauma center, the same approach is used, substituting intravenous sedation and topical anesthesia for inhalational anesthesia because the latter is not available in the ED.
Airway management is complicated by the fact that patients with blunt anterior neck trauma must be presumed to have a C-spine injury. Up to 50% of patients with blunt airway injury have a C-spine injury,25 which is discussed here in the context of airway management.
In clothesline injuries, in which the neck is struck, usually transversely, by a fence wire or similar object, the central neck area may be significantly but deceptively disrupted from the impact.17 Although these injuries can be dramatic and often require immediate airway management, the airway itself is often intact, signified by identification of intact structures and the absence of air bubbling or gurgling during negative-pressure or positive-pressure ventilation. Early intubation from above, preferably over an FFB, is best in these cases. If the airway has been breached, and gurgling or subcutaneous air is evident in the tissues of the neck, positive-pressure BMV is not likely to be successful in oxygenating the patient, and attempts at BMV may result in insufflation of large amounts of air into the soft tissues of the neck, further compromising the airway and the attempts at securing it. The best approach in these cases is to attempt to secure the airway over an FFB using sedation and topical anesthesia, with a plan to progress directly to a cricothyrotomy or emergency tracheostomy, if fiberoptic intubation is unsuccessful.
3 Maxillofacial Trauma
Maxillary fractures usually occur in one of the classically described Le Fort patterns. Although the precise location of the Le Fort fracture pattern is sometimes difficult to remember, the Le Fort I, II, and III fractures can be thought of as follows (see Fig. 41-2). The Le Fort I fracture represents separation of the roof of the mouth from the face, with the fracture extending through the alveolar ridge to the base of the nose and separating the alveolar ridge and hard palate from the rest of the face. The Le Fort II fracture is separation of the central face from the rest of the face and cranium. The fractures extend from the base of the nasal bones through the medial orbits down through the maxilla to the posterior molars, effectively creating a free-floating central face fragment. The Le Fort III fracture is separation of the face from the skull. This fracture extends from the base of the nasal bones through the orbits to the lateral orbital rims and then through the zygomatic arch and down through the pterygoid plate.
An uncommon but disastrous presentation of maxillofacial injury occurs when an attempted suicide fails because the gun (usually a shotgun) is oriented in such a way as to have the mass of the shot pass upward through the face rather than on a posterior trajectory through the brainstem. This often happens when the patient places a rifle or shotgun under the chin and then tries to reach downward for the trigger. This movement naturally leads to extension of the neck, and the trajectory of the missile is altered, causing it to pass upward through the face (Fig. 41-4). Although such injuries occur with massive facial distortion, airway management can range from easy to virtually impossible. Destruction of the mandible, tongue, palate, and nasopharynx often makes orotracheal intubation impossible, and hemorrhage is usually extensive. Primary surgical airway management is usually the method of choice. However, the injury can be predominantly anterior, sparing the airway, and the mandible and tongue can be displaced forward, permitting adequate oral access for orotracheal intubation. Nonetheless, efficient suctioning is usually required because the hemorrhage can be significant.
B Cervical Spine Injury
Unstable injury to the C-spine presents a particular hazard with respect to airway management because of the potential to cause or exacerbate spinal cord injury. C-spine injury usually occurs when there is high-energy transfer, such as in a motor vehicle collision, but it can occur with relatively minor trauma in patients with significant degenerative disease of the C-spine, such as rheumatoid arthritis or osteopenia. Motor vehicle collisions are the greatest cause of spinal injury, accounting for about 50% of these injuries, followed by falls, athletic injury, and interpersonal violence.26
In the trauma resuscitation room, all patients who have been subjected to significant blunt trauma should be assumed to have a C-spine injury until it has been excluded. Penetrating trauma can also cause spinal injury, but creation of an unstable spinal injury without concomitant spinal cord injury is exceedingly rare. With penetrating injury, it is usually apparent whether spinal injury has occurred because the patient sustained a neurologic disability. Barring this finding, C-spine immobilization in a patient with isolated penetrating trauma is typically unnecessary and may even be harmful.27–29
One of the significant challenges related to airway management in patients with blunt trauma is the inability to determine definitively whether the patient has a C-spine injury before intubation is required. Fortunately, most patients with a C-spine injury do not require intubation during the acute phase of resuscitation. However, those who have the most severe trauma are likely to require intubation, and this is the same population who is at highest risk for spinal injury.30 It has been estimated that 2% to 14% of all patients with serious blunt trauma have a significant C-spine injury.31,32
The decision about whether to obtain portable C-spine imaging before intubation must take into account two radiographic principles. First, a single, portable, lateral, cross-table radiograph is highly insensitive for significant C-spine injury. At least 25% of lateral C-spine radiographs fail to visualize the cervical-thoracic junction (C7-T1).33 Even if the lateral radiograph is adequate, it should be considered no more than 80% sensitive for C-spine injury.34 A complete three-view C-spine series fails to identify about 15% of significant C-spine injuries, and it is difficult to obtain adequately for patients in cervical collars.35 In consideration of this information, no plain radiograph should be interpreted as indicating that the C-spine is free of injury and that movement can be undertaken with impunity during intubation.
Second, the severe limitations of portable C-spine radiographs question their value before intubation. Current guidelines recommend the use of CT for C-spine evaluation of patients with trauma.36 Given the limitations of portable cross-table plain radiographs of the spine and the danger of remote imaging before airway management, it is prudent to presume a C-spine injury and intubate with in-line C-spine stabilization without imaging.
Intubation should be performed with the anterior portion of the cervical collar open because it may limit laryngoscopy. Leaving the collar intact has not been shown to reduce significant C-spine movement during intubation, and is not a substitute for manual in-line stabilization.37–39 Although cricothyrotomy can be performed through the openings in most cervical collars, it is often technically challenging, and it is preferable to remove the anterior one half of the collar before undertaking surgical airway management. The debate regarding nasotracheal intubation versus various awake intubation techniques versus RSI in the trauma patient is discussed in “Principles of Airway Management in the Trauma Patient.”

Full access? Get Clinical Tree