Immediate Management of Life-Threatening Problems
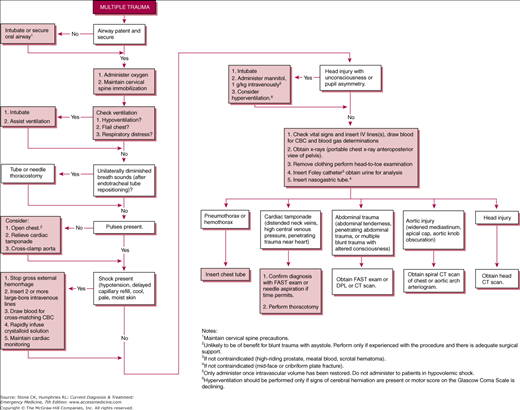
(See Figure 12–1.) The primary goal in providing care to the trauma patient is effective resuscitation while minimizing the time from injury to definitive care.
Trauma care begins at the scene of the incident. It is important for hospitals to have good working relationships with local fire departments and emergency medical services (EMSs) to ensure that proper care is provided early. Preparation efforts should be coordinated between the emergency departments and the local EMS systems including prehospital protocols related to the treatment and transport of trauma patients. Transport protocols should incorporate decision-making guidelines including information regarding transporting patients to the most appropriate facility and the proper use of air medical transport. Prehospital providers should be trained to detect specific injuries and know the mechanism of forces that could predict the possibility of severe injury (Table 12–1). Prehospital personnel should provide early notification to the emergency department for all major trauma patients to allow emergency department preparedness.
| Mechanism of Injury | Clinical Information |
|---|---|
| Falls > 20 ft | Systolic blood pressure < 90 mm Hg |
| Rollover motor vehicle collision Crash speed >40 mph | Respiratory rate <10/min or >29/min |
| Auto-pedestrian or auto-bicycle collision | Glasgow Coma Scale score <10 |
| Ejection of patient | Penetrating trauma other than distal extremity |
|
|
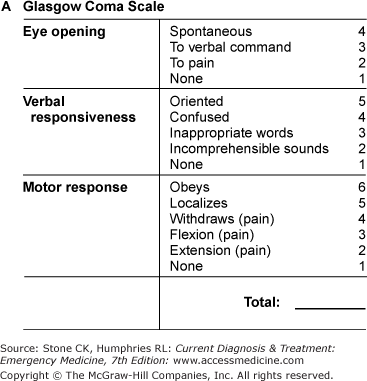
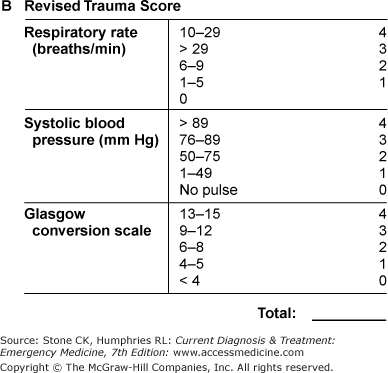
Injury-scoring systems, such as the Glasgow Coma Scale (GCS), Trauma Score, and Revised Trauma Score, may be used to help quantify the degree of injury (Figure 12–2).
Maintain a high index of suspicion with pediatric, geriatric, and obstetric patients. Their physiologic responses to major trauma differ from those of other patients, and their injuries are often missed or delayed in diagnosis. Early transfer to definitive care improves outcomes in these patient groups.
Emergency department response should include a stepwise notification system to alert local surgeons or trauma teams and ancillary services such as X-ray, computed tomography (CT) scan, laboratory, blood bank, and operating room personnel. Initial stabilization and resuscitation is done most effectively if a well-organized team approach is used. The key to an organized system is the designation of a person in charge to oversee the total care of the patient. The team leader should assign specific tasks to emergency department team members. It is important for everyone to understand their roles, know where equipment is located, adhere to universal precautions, and keep noise and extraneous conversation to a minimum. Constant reassessment of the patient and maintenance of a high index of suspicion for possible injuries are important in the evaluation and resuscitation of trauma patients.
The initial assessment consists of a rapid primary survey, initiation of resuscitative measures, followed by a secondary survey. The primary survey includes evaluation of the airway, breathing, and circulation and a brief neurologic examination. During the initial assessment, assess the patient for injuries or conditions that would indicate the patient’s care needs require a higher level of care at a trauma center. Early initiation of transfer to the most appropriate trauma facility reduces morbidly and mortality in critically ill or injuries patients. Delay in transfer of theses patients for local diagnostic work-up delays their arrival to definitive care facility and potentially increases morbidity and mortality. Problems identified in the primary assessment should be corrected immediately. Several tasks should occur simultaneously such as assessing the patient; initiating resuscitation; placing the patient on the cardiac monitor, pulse oximetry, and supplemental oxygen; and initiating intravenous lines. Rapid stabilization of airway, breathing, circulation, and neurologic status is paramount for patient survival.
Airway management and maintenance of adequate oxygenation are extremely important in the multiply injured patient (See also Chapter 10). Shock leads to an oxygen deficit, which increases the body’s demands and necessitates the need for supplementary oxygen. Cervical spine immobilization is considered part of airway management in trauma patients. To open the airway, a modified jaw thrust should be used with cervical spine control. An oropharyngeal or nasopharyngeal airway is useful to help maintain an airway. The nasopharyngeal tube may be used in semiconscious patients with an intact gag reflex. The oropharyngeal airway should be used only in unconscious patients without a gag reflex; otherwise, it may induce vomiting.
Obtain a definitive airway in any patient who is not breathing, has inadequate ventilation or oxygenation, has an unprotected airway without a gag reflex, or has a decreased level of consciousness with a GCS score less than 8. Emergency department providers should be knowledgeable about and skilled with a variety of surgical and nonsurgical methods of securing an airway. Patients with inadequate ventilation and oxygenation require bag-mask-ventilation until intubation is accomplished. Tracheal intubation may be accomplished by two methods: nasotracheal or orotracheal. Both methods require good cervical spine immobilization including manual stabilization of the neck. With adequate training and experience, rapid-sequence induction (RSI) intubation offers many advantages in the multiply injured trauma patient. RSI involves the use of paralytics to rapidly achieve muscle relaxation and sedatives to render the patient unconscious and unaware of laryngoscopy and intubation. Use of paralytics helps protect against a rise in intracranial pressure associated with laryngoscopy, and with good manual cervical spine stabilization there is less risk of additional cervical spine injury. The use of paralytics and sedation requires a good working knowledge of the medications’ indications, their side effects, and their contraindications, in order to minimize complications associated with the procedure. Being well trained in backup airway maneuvers, such as the laryngeal mask airway, lighted stylet, fiberoptic intubation, and surgical airway options, is imperative prior to initiating RSI in a patient. RSI is relatively contraindicated in patients who cannot be ventilated with a bag-valve-mask if intubation proves difficult or impossible. If orotracheal or nasotracheal intubation is unsuccessful, a surgical airway such as a cricothyrotomy should be performed.
Assess adequacy of ventilation by inspecting the chest wall for adequate expansion; looking for paradoxical rise of the chest, flail segments, and sucking wounds; and noting labored respirations or auxiliary muscle use. Auscultate the lungs for the presence of symmetrical breath sounds.
If breath sounds are unilaterally diminished and the patient is intubated, consider withdrawing the endotracheal tube 2–3 cm in case the tip is residing in a main-stem bronchus, and then recheck the breath sounds. Persistently, diminished breath sounds imply pneumothorax or hemothorax. If the patient is hypotensive, in shock, or laboring to breathe, perform a tube thoracostomy immediately. Should a delay exist before this can occur, decompress the chest with a 14-gauge angiocatheter or other catheter-clad needle inserted in the second intercostal space at the midclavicular line. A stable patient with diminished breath sounds may await a chest X-ray for confirmation prior to decompression with a needle or thoracostomy tube.
Treat a sucking chest wound by sealing the wound with an occlusive dressing (eg, petrolatum-impregnated dressing) at three points and then performing a tube thoracostomy (not through the chest wall defect). Adequacy of ventilation can be confirmed with arterial blood gas measurements.
Rapidly assess blood pressure and pulse. A narrowed pulse pressure suggests hypovolemic shock. Hypotension is suggestive of severe intravascular depletion. Rapidly evaluate the abdomen because it is frequently a source of significant hemorrhage in the multiply injured patient. Severe pelvic fracture or pelvic ring disruptions can be associated with massive intrapelvic hemorrhage. Give the patient crystalloid initially and then blood, if needed, to improve perfusion.
If spontaneous cardiac activity is not detected by palpation of the carotid artery, begin cardiopulmonary resuscitation immediately. If the patient has penetrating chest trauma and arrives by EMS with Cardiopulmonary Resuscitation (CPR) in progress, assess the patient for signs of life. If there are no signs of life and no cardiac electrical activity present, no further resuscitative effort should be made. If there are signs of life and the patient has been pulseless for less than 15 minutes, consider emergency thoracotomy. Only experienced physicians trained in emergency thoracotomy should perform this procedure. If the patient has been pulseless longer than the abovementioned time limits or arrives with CPR in progress from blunt trauma, regardless of the cardiac rhythm, thoracotomy is not indicated and has not been shown to improve survival. Initiate closed chest compressions with volume resuscitation with crystalloids and cardiac drugs per advanced cardiac life support guidelines (Chapter 9).
Stop obvious external hemorrhage using direct pressure with sterile dressings. Scalp wounds, even small ones, can produce significant blood loss if not controlled. Sometimes direct pressure and dressings are not sufficient. For uncontrolled scalp wound hemorrhage, the wound should be closed with sutures, staples, or, if available, Raney scalp clips, preferably using sterile technique. If a nonsterile technique is used, the wound should be reopened and inspected carefully, cleansed, and then definitively closed using sterile technique when the patient stabilizes. Bleeding vessels should not be clamped indiscriminately. Rarely will compression be insufficient to control an exsanguinating arterial hemorrhage from an extremity. A blood pressure cuff inflated proximal to the wound can serve as an effective tourniquet temporarily until surgical control of the bleeding can be achieved. Recent studies indicate tourniquet use in uncontrolled extremity injuries, particularly if placed before shock is clinically evident, can be life saving with little limb complications.
(See also Chapter 11) Shock is defined as inadequate tissue perfusion and is further classified as mild, moderate, or severe, based primarily on clinical criteria. Cool, pale skin; diaphoresis; delayed capillary refill (>2s); tachycardia; and mental status changes are reliable indicators of shock. Hypotension and oliguria are presumed to be due to shock until proved otherwise. Do not assume that perfusion is adequate on the basis of a supine pulse and blood pressure alone, because these signs may not change until late in shock. This is particularly true in young healthy adults—who are the most common victims of multiple trauma. Patients taking β-blockers (or other medications that blunt the normal response to adrenergic stimulation) may not exhibit tachycardia despite profound shock.
Shock in the traumatized patient is due to hypovolemia from hemorrhage in the majority of the cases. Cardiac tamponade and tension pneumothorax are conditions that can cause shock, which must be excluded rapidly in the assessment of hypotensive trauma patients. Spinal cord or brain injury may contribute or (rarely) may cause shock without concurrent volume loss. In a trauma patient, shock should be treated as hypovolemic shock with volume infusions until other causes of shock are found.
A quick neurologic examination may be accomplished by using the GCS (see Figure 12–2). The GCS allows for quick assessment of the patient’s level of responsiveness to determine if he or she is awake and alert; responds to verbal stimuli with eye opening or following of commands; responds to painful stimuli (eg, sternal rub, muscle, or tendon squeeze) by appropriate movement, localization, or posturing; or is unresponsive.
Assess the patient’s pupils for symmetry, size, and reactivity. An asymmetrically enlarged pupil in an unresponsive patient may imply transtentorial herniation, which should be treated with endotracheal intubation along with the other interventions to reduce intracranial pressure such as short-term hyperventilation and administration of mannitol (Chapter 22).
Evaluation and treatment must proceed rapidly and simultaneously. During the primary survey, correct any identified problems immediately. Place the patient on a cardiac monitor, including pulse oximetry with supplemental oxygen administered. Initiate intravenous lines and order initial laboratory studies. Place a Foley catheter after examination of the perineal area and rectal examination. Do not insert a urethral catheter if there is obvious injury to the external genitalia, obvious urethral bleeding, scrotal hematoma, a malpositioned or high-riding prostate on rectal examination, or difficulty in passing the catheter. Monitoring of urine output is important in evaluating the patient’s response to resuscitative efforts. Urinary output below 0.5 cc/kg/h indicates significant hypovolemia.
Insert multiple large-bore (≥16 gauge) catheters in a patient with profound shock. Initiate at least two intravenous lines. Consider a large-bore central line to administer large amounts of fluids rapidly or to monitor central venous pressure in patients with poor peripheral venous access in profound shock, in the elderly, and in patients with significant comorbid disease. If peripheral IV is not easily obtainable, proximal humerus intraosseous line should be started. Studies have shown that intraosseous lines are fast to place and can be used for volume resuscitation or medication administration when peripheral IV is difficult.
Consider blood specimens for hematocrit or complete blood count (CBC), electrolyte measurements, renal function tests, and coagulation (prothrombin and partial thromboplastin times). Obtain a urine sample for gross blood. Obtain a pregnancy test from female patients of child-bearing age. If abdominal trauma is present, consider laboratory studies for liver enzymes and lipase. If severe shock is evident or suspected, type and crossmatch for four units of packed red blood cells, and obtain an arterial blood gas and serum lactate. Base deficit and or lactate can be useful in determining the presence and severity of shock. Serial measurement of these can be useful in monitoring the response to therapy. Trauma patients have high rates of alcohol and drug use, and a blood alcohol level or urine drug screen may be useful in evaluating patients with altered mental status.
If clinical evidence of shock is present, initiate intravenous infusion of crystalloid solution. Give up to 2 L of crystalloid solution to support intravascular volume before giving blood. Give crossmatched or type-specific blood, if available, to a patient in persistent shock unresponsive to crystalloids. If typed and crossmatched blood is not available, then give type O blood. Reserve type O-negative blood for females younger than 50 years; all others should receive type O-positive.
During the acute phase of evaluation and resuscitation, the most valuable X-rays are those of the chest and pelvis. These X-rays assist in the evaluation of potential injuries associated with a large amount of blood loss. Although spine X-rays are important, the spine can be protected from further injury by adhering strictly to spinal immobilization precautions during the initial evaluation and resuscitation.
Large hemorrhages can also be found in the abdominal cavity. The abdomen can be rapidly evaluated in the unstable trauma patient by using bedside emergency ultrasound and performing a FAST (focused assessment with sonography for trauma—see Chapter 6) exam to look for free fluid. In stable trauma patients, a contrasted CT scan of the abdomen and pelvis provides useful information regarding the extent of specific organ injuries. Because ultrasound and CT scan are poor in evaluating bowel injuries, maintain a high index of suspicion so that this type of injury is not overlooked, especially in pediatric patients.
Frequently reassess a multiply injured trauma patient for evidence of new or ongoing signs of shock. In the multiply injured patient, hemorrhage is the most common cause of shock. Even so, it is important to conscientiously assess the patient for other underlying causes of shock. Early surgical consult is important for any trauma patient with signs of shock. Splint fractures, administer antibiotics and tetanus toxoid when needed, and keep patients warm. Pay close attention to the prevention of further injury. Avoiding infection, hypothermia, coagulopathy, and ongoing blood loss is important for minimizing possible mortality and morbidity.
- Evidence of external blood loss
- Injuries with associated internal blood loss
- Tachycardia
- Decreased level of consciousness
- Decreased urine output
- Delayed capillary refill
- Hypotension (late sign)
Defined as inadequate tissue perfusion due to decreased cardiac output secondary to blood loss. Hemorrhagic shock accounts for the overwhelming majority of trauma patients in shock. Clinical signs are due to compensatory mechanisms. For example, excess sympathetic nervous system stimulation causes tachycardia and peripheral vasoconstriction, whereas decreased peripheral and renal blood flow result in decreased urine output, pallor, delayed capillary refill, and weak peripheral pulses.
Identify and control external hemorrhage during the primary survey. Logroll trauma patients to examine their backs. A single hematocrit may provide a baseline but is not helpful in detecting acute occult hemorrhage. Serial hematocrits over several hours are useful in determining continued blood loss, because a single initial value may be deceivingly normal.
Major sources of occult blood loss are as follows:
Each hemithorax may contain 1–2 L of blood, primarily as a result of a pulmonary laceration or laceration of intercostal vessels or internal mammary artery due to either penetrating or blunt trauma. Suspect hemothorax in cases of shock associated with decreased or absent breath sounds or when dullness to percussion is present on the affected side. A supine chest X-ray may only show haziness over the hemithorax.
Assume intra-abdominal hemorrhage in patients in shock with a normal chest X-ray and no external sources of bleeding. Abdominal distention is a late and unreliable sign. Kehr’s sign is referred pain to left shoulder due to diaphragmatic irritation associated with hemoperitoneum and splenic injuries. Cullen’s sign (periumbilical ecchymosis) is a late finding in intra-abdominal hemorrhage. Use a FAST exam to examine unstable patients. Stable patients should undergo CT scan of the abdomen.

Full access? Get Clinical Tree