The Ethics of Withholding and Withdrawing Mechanical Ventilation: Introduction
To save the lives of critically ill patients, intensivists utilize sophisticated technologies to support vital organs until treatments reverse underlying medical conditions. Most patients recover from the acute event, a few die rapidly, and the remainder fail to improve and remain dependent on life-sustaining treatments. In this last group, the chance of recovery changes from one day to the next, and questions often arise about the appropriateness of continuing life support, especially mechanical ventilation.1
Over the last half century, health care professionals in intensive care units (ICUs) have been forced to make decisions for patients who remain dependent on mechanical ventilation with death in the short term as the only possible outcome.2 In these patients, continued treatment in the hope of cure is rarely the best option.3 Mechanical ventilation may be prolonged beyond the point of beneficence, robbing patients of their dignity and families of their right to honest prognostic information and an opportunity to prepare for bereavement. The best option here is a decision to forego life-sustaining treatment.
Because respiratory failure, shock, and coma are common reasons for ICU admission, mechanical ventilation is the most widely used life-sustaining treatment in the ICU.4 Thus, mechanical ventilation is also the most common target of a decision to forego life-sustaining treatment.5–10 Although most patients are successfully weaned off the ventilator, a few die while on the ventilator or immediately after weaning.11 Ideally, a decision to forego life-sustaining treatment, which consists of moving from curative care to comfort care, should be based on the patient’s wishes.12,13 When the issue of comfort care arises, however, fewer than 5% of patients are able to participate in decisions, and knowledge of their preferences is usually unavailable.14,15 Therefore, concern that curative care may be harmful is often voiced first by the ICU team, which then broaches the issue with the family or surrogate decision maker. Thus, barely a few years after the creation of ICUs, intensivists realized that, in addition to fighting death, their duties included the daunting task of accepting and managing death. This task requires (a) identifying situations in which all hope of recovery is lost and life-prolonging treatments become death-prolonging treatments, which should be withdrawn or withheld; (b) promptly initiating a continuous process of family care based on sensitive and straightforward information and communication; and (c) improving the ability to manage death, via epidemiologic studies of practices, interventional studies of end-of-life strategies, and continuing education aimed at honing the information and communication skills of all ICU professionals. Warding off death and restoring self-sufficiency have been the main goals of intensivists for decades; now, ICU professionals are becoming acutely aware that they must develop a professional approach to dying patients, learn what makes a “good death,” and provide dying patients and their families with support, reassurance, comfort, dignity, and freedom from guilt.
The literature on end of life in the ICU comprises epidemiologic studies (descriptive, deductive, or quantitative) and qualitative studies of theoretical concepts that allow subtle interpretations of structures, experiences, roles, interactions, and perspectives. This review provides an interpretation of published data on limiting mechanical ventilation and other life-supporting treatments in patients dying in the ICU. Its goal is to help readers understand and organize the decision-making process within an ICU team and to ensure that decisions are implemented so as to give the patient a “good death” and families bereavement support.
Fundamental Issues of Ethics
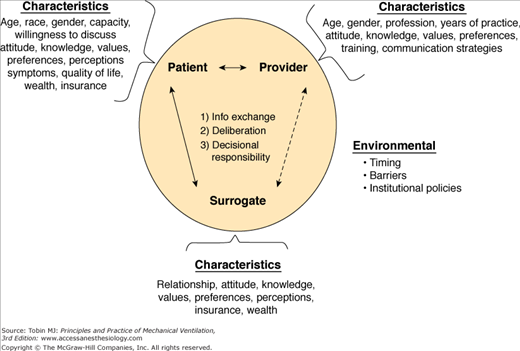
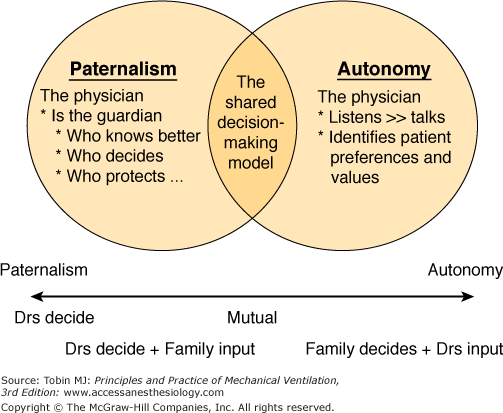
The field of bioethics, born in the late 1960s, rests on four fundamental ethical principles (beneficence, nonmaleficence, autonomy, and distributive justice) and describes a spectrum of patient–physician relationship styles ranging from paternalism to autonomy (Fig. 66-1).16 The four fundamental ethical principles guide decisions in the ICU management of dying patients and their families. Regarding beneficence and nonmaleficence, we discuss studies that address the specific needs and expectations of dying patients. We then briefly contrast paternalism and autonomy, and argue that the long-standing controversy opposing these two models should give way to emphasis on the shared decision-making model. We also discuss the double-effect principle accepted by the U.S. Supreme Court, Society of Critical Care Medicine recommendations, and international consensus in the support of the use of sedation and analgesia to relieve symptoms, provided death is not intended, although it may be foreseen.17–20 The unresolved debate regarding the relative merits of terminal extubation and terminal weaning for taking dying patients off the ventilator is mentioned. Regarding justice, we do our utmost to convince the reader that cost considerations are irrelevant to a decision to forego life-sustaining treatment.
In a study by Singer et al,21 patients identified five domains of quality end-of-life care: adequate relief from pain and anxiety;22 avoiding inappropriate prolongation of dying; achieving a sense of control; relieving burden; and strengthening relationships with loved ones. When a patient is dying, intensivists must make it clear that they are dedicated to providing optimal care throughout the dying process;23 to treating the patient with respect and dignity; and to relieving pain caused by physical, emotional, social, and spiritual factors.24,25 Patients fear to be abandoned. They should be assured that the doctor is and will remain on their side, stopping useless interventions, and providing treatments that ensure comfort.26 Encouraging family and friends to be present at all times is another component of this effort to ensure beneficence; however, some family members may be unbearably distressed by having to spend long hours with their dying relative. The presence of a chaplain, chosen by the patient and family, and access to religious rites should be encouraged.27
After years of heated debate opposing autonomy and paternalism, a model in which decision making is shared with family members is gaining precedence (Fig. 66-2). This model upholds patient autonomy28 without forcing family members to be involved in decisions they do not want to make29 or are not ready to make.30 The shared decision-making model stands in sharp contrast to paternalism, in which the physician shields the patient, making decisions alone so as to protect the patient and family from the potentially harmful effects of making painful decisions.13 Because most ICU patients are unable to make decisions,31,32 sharing in a decision to forego life-sustaining treatment shifts to the family members.12 Attempting to wake ICU patients so that they can participate in decisions in the name of autonomy clashes violently with the principles of beneficence and nonmaleficence.33 Beneficence requires that family members be empowered to understand the patient’s situation,34 to identify and meet their expectations,35,36 and to gain awareness of possible anxiety or depression that might impair their decision-making capabilities.37 Under no circumstance should anxiety or depression in family members be used to justify benevolent paternalism; on the contrary, communication with families must receive close attention as a means of empowering families to share in decisions.12 Reports from Canada, Sweden, and the United States describe sharing discussions and decisions as rational38 and as crucial to family satisfaction.39–42 In addition, studies of family outcomes several weeks or months after the death of a patient in the ICU have highlighted major difficulties and profound inadequacies in information.27,43–45 Finally, nonmaleficence in this setting requires intensive communication with families if needed; a multidisciplinary approach can be used, or external ethical advice obtained, with the objective of empowering families to achieve their own goal (whether this is sharing in decisions or leaving decisions to the intensivists) and of convincing families that comfort care is preferable over aggressive interventions.46–48 When family members have not received optimal information, involving them in the decision-making process probably carries a risk of subsequent posttraumatic stress and abnormal grief reactions.30
The SUPPORT (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments) studies showed a high rate of unacceptable pain in dying patients.49,50 When withholding or withdrawing mechanical ventilation is in order, clinicians have the duty to emphasize comfort and to relieve pain and anxiety in their patients. Opioids and anxiolytics remain the reference treatment for these symptoms.17–20 Opioids may hasten death by inducing respiratory depression,51 but this risk is legally and ethically acceptable.19,52–54 In contrast, use of high-dose opioids to cause death by a person making the decision alone is not consonant with optimal end-of-life care. This is voluntary euthanasia and is illegal, even in The Netherlands, Belgium, and the states of Oregon and Washington, where patients can request and obtain the assistance of a physician to commit suicide.19,52 Because it is the physician’s intention that separates opioid use to relieve pain and anxiety from opioid use to hasten death, the line between the ethical and the unethical, the legal and the illegal, is subjective.18,55 Although some physicians may tend to use higher doses to ensure patient comfort, this practice cannot be likened to euthanasia.56 Nevertheless, eliminating ambiguity from end-of-life decisions can be extremely difficult.57
The optimal method for taking dying patients off the ventilator remains actively debated. The controversy consists of advocates of terminal weaning, in which volumes, respiratory rate, and fractional inspired oxygen concentration (FIO2) are reduced gradually, versus proponents of terminal extubation with sedation,58 which restores the normal appearance of the patient but carries a risk of respiratory secretion accumulation with asphyxia and gasping.59,60 Terminal weaning is perceived as less active and therefore less distressing for health care professionals; furthermore, the family members are spared the ordeal of witnessing gasps, which they interpret as suffering.61 In addition, extubation may wrongly suggest to the family that the patient is better and no longer needs the ventilator.61 Opponents of extubation for ventilation withdrawal have pointed out that even patients who survive extubation remember the weaning period as a time of stress, discomfort, loss of hope, and extreme fear.62
Cost considerations63 have entered into the treatment-limitation debate on the grounds that using ineffective treatments in one patient may deprive another patient of lifesaving treatment or ICU admission, thereby violating the principle of distributive justice.64 Guidelines65 suggest that elderly patients and patients with chronic conditions (cancer, hematologic malignancies, or chronic obstructive pulmonary disease) should be denied ICU admission or should receive a decision to forego life-sustaining treatment earlier than other patients. Whether the principle of distributive justice applies to a decision to forego life-sustaining treatment is controversial, and the relevance of the cost/efficacy concept to ICU management has been challenged.66 Denying ICU admission to a seriously ill patient for cost-containment reasons makes little sense, because other resources will then be used for the patient elsewhere, sometimes for a longer period and to the detriment of patient comfort.67 Furthermore, patient-centered care allows the patient to die with dignity, free of pain and anxiety, while placing the family in optimal conditions for preparing the bereavement process.64,68,69 Interventional studies of intensive communication with families of patients dying in the ICU found cost savings related to conflict prevention70,71 that diminished the use of ineffective treatments.46–48,72
Terminology
Five mutually exclusive categories of a decision to forego life-sustaining treatment have been defined. The first category is the do-not-resuscitate order for cardiac arrest. The second category comprises a decision to forego life-sustaining treatment in patients who are in a chronic vegetative state. Third is the decision to withhold a potentially beneficial treatment (e.g., mechanical ventilation, catecholamine administration, or dialysis). Fourth is withdrawal of life-sustaining treatment. The fifth category involves active induction of death (administration of a treatment that results in death). Do-not-resuscitate orders are not relevant to the present chapter. We do not discuss patients in a chronic vegetative state, because they raise specific issues whose resolution relies on concepts that do not apply to other ICU patients. Neither do we deal with euthanasia (injection of a lethal substance), which has been used in the past but is no longer an acceptable component of end-of-life care in ICU patients. Euthanasia does not constitute care, virtually never involves a rational collegial decision-making process, leaves anxiety and pain unrelieved, and fails to respect the dignity of the patient and family. We believe that euthanasia should be banned from ICUs and all other places where medical care is delivered.
Epidemiology of the Decision to Forego Life-Sustaining Treatment in the Intensive Care Unit: Geographic, Cultural, and Religious Variations
In most countries, most deaths in the ICU are preceded by a decision to forego life-sustaining treatment.6,7,9,40,56,73–81 In addition, the incidence of decisions to forego life-sustaining treatment may be increasing over time.82,83 In patients discharged alive from the ICU, a decision to forego life-sustaining treatment taken in the ICU influences hospital survival.84 In practice, withholding mechanical ventilation precedes or occurs concomitantly with withdrawal of all other life-sustaining treatments.10,73 Withholding and withdrawal occur within 3 days after ICU admission, and the patient usually dies within the next 24 hours.85 There is widespread agreement that there is no ethical difference between withholding and withdrawal,86 although withdrawal has been described as more difficult for intensivists74 and is not used in some countries.73
Wide variation exists regarding the incidence of decisions to forego life-sustaining treatment (Table 66-1).87 These variations across countries and cultures have been identified in studies comparing practices,88,89 studies of responses to ethical scenarios,74,90 and descriptive studies.7,9,10,73,75,78,82,91–105 The Ethicus study described the variable practices to forego life-sustaining treatments in thirty-seven ICUs in seventeen European countries (Table 66-2). In southern Europe, the proportion of deaths after unsuccessful resuscitation was greater than in the rest of Europe. In northern Europe, the time from a decision to forego life-sustaining treatment to death was shorter.73 These data confirm the considerable variability in approaches to bioethical issues in Europe.88,106
| References | WH/WD in Dying Patients (%) | Involvement of Families in Discussions and Decisions (%) | |
|---|---|---|---|
| United States | 6, 11, 75, 78, 82, 102 | >90 | 90 |
| Canada | 94 | 80 | 90 |
| Europe | 73 | 76 | — |
| Israel | 79 | 91 (no WD) | 28 |
| England | 102 | 85 | >90 |
| France | 7, 9, 30 | 50 | 50 |
| Hong Kong | 126 | 23 to 61 | 95 |
| Spain | 76 | 34 | 41 |
| Italy | 98 | 8 | 58 |
| Australia | 101, 105 | 70 to 81 | — |
| India | 103 | 49 | 100 |
| Unsuccessful CPR | Brain Death | WH | WD | Active Shortening of the Dying Process | |
|---|---|---|---|---|---|
| Northern Europe | 154 (10.2%) | 48 (3.2%) | 575 (38.2%) | 714 (47.4) | 14 (0.9%) |
| Central Europe | 217 (17.9%) | 92 (7.6%) | 412 (34.1%) | 409 (33.8%) | 79 (6.5%) |
| Southern Europe | 461 (30.1%) | 190 (12.4%) | 607 (39.6%) | 275 (17.9%) | 1 (0.1%) |
| Whole of Europe | 832 (19.6%) | 330 (7.8%) | 1594 (37.5%) 1 | 1398 (32.9%) | 94 (2.2%) |
| Hospital mortality | 100% | 100% | 89% | 89% | 100% |
| Total | 832 (19.6%) | 330 (7.8%) | 1594 (37.5%) | 1398 (32.9%) | 94 (2.2%) |
Additionally, the role given to the patient’s and family’s opinion in the decision to forego life-sustaining treatment also varies widely, although compassion and respect for the patient are universally recognized as crucial.12,13 Some differences may be explained by the fact that in the late 1980s the United States adopted a model based on patient autonomy and self-determination,96,107 whereas other countries kept a paternalistic model in which the physician alone determines the appropriate level of treatment intensity.7,9,74,90,91,108,109 Evidence, however, suggests that variability exists within a given country, with some physicians in traditionally paternalistic countries involving patients and families in the life support decision making process, and vice versa.75,78,82,94
Religious beliefs of both patients and providers are reported to influence the attitudes of intensivists towards life support decisions.88,110,111 The Ethicus study identified variations across religions with Jewish, Greek Orthodox, and Moslem physicians more likely to withhold therapy, and Catholic and Protestant physicians more likely to withdraw therapy. Time to first therapy limitation also varied from 1.6 days for Protestant physicians to 7.6 days for Greek Orthodox physicians.73,112
Variable ICU admission rates and policies may influence the variable incidence of decisions to forego life-sustaining treatment. The SUPPORT study group found that half the patients with chronic diseases were in the ICU within the 3 days preceding death and that one-third of patients spent at least 10 days in the ICU during the hospitalization that preceded death.50 In 1995, 20% of deaths in the United States or Canada occurred in the ICU.113,114 In other countries, ICU admission policies are more restrictive,102,115–117 so that comparisons are inherently biased. Predictors of increased end-of-life ICU utilization include age, number of comorbidities, hospital type, number of available hospital beds, and lack of outpatient to inpatient continuity of care.118–120 The high incidence of in-hospital and in-ICU deaths, which has emerged over recent decades in industrialized countries, must be considered under the harsh light of data showing poorer quality end-of-life care in hospitals and ICUs as compared to home hospice care,121,122 in addition to minimal gains in survival.123 Important differences also exist among race. In the United States, black and Hispanic patients are more likely to die in an ICU124 and incur 30% to 50% more health care expenditures in the 6 months preceding death than white patients,125 even after control for variables such as geography and socioeconomic status. Additionally, there is limited evidence that white patients who prefer intensive end-of-life care are more likely to receive it than are black patients with the same preference.111
Legal Decisions to Date
The courts recognize that withholding or withdrawing life-sustaining treatment and giving palliative care are legal. In the United States, the ethical principle informing laws that allow decisions to forego life-sustaining treatment is autonomy, manifesting as informed consent from the patient or family, who can also refuse treatment withholding or withdrawal.14,19,52,126 Among European countries, The Netherlands was the first to allow euthanasia and physician-assisted suicide.106 Belgium followed suit in 2002.127,128 Nevertheless, in neither country does the law deal specifically with patients receiving life support in the ICU.129 In France, the Senate has passed a law authorizing physicians to let patients die if they are kept alive only through artificial means, treatment is futile, and death is imminent.130
After the advances in mechanical ventilation achieved in the 1970s and 1980s, the notion that mechanical ventilation should at times be withheld or withdrawn was deeply disturbing to many intensivists. By the 1980s, however, intensivists could no longer deny that life-sustaining treatment merely prolongs the dying process in some patients.22,86,107
The confusion that exists between ethical concepts and legal concepts is frequently disconcerting to intensivists. From both the ethical and legal points of view, a decision to forego life-sustaining treatment is acceptable only when it constitutes an expression of the patient’s personal autonomy, that is, when it is made with the informed consent of a competent patient or, when the patient is incompetent, based on knowledge of the patient’s wishes. All adults have the right to accept or refuse treatment and to define their preferences and values.28,33,131,132 This right does not end when an ICU patient becomes mentally incompetent, and it can be exercised by the patient’s surrogate decision maker.14,52 In 1990, the U.S. Supreme Court upheld the withdrawal of life-sustaining treatment at a patient’s request;131 more recently, it stated that decisions to forego life-sustaining treatment in ICUs did not constitute physician-assisted suicide or euthanasia.133 These rulings apply to all fifty states, in theory at least. Furthermore, the Supreme Court has ruled that physicians cannot use futility as a basis for making a decision to forego life-sustaining treatment of their own accord. Nevertheless, the Supreme Court issued detailed recommendations on palliative care, acknowledging that sedatives and analgesics may be given, when needed, to alleviate the symptoms of a dying patient, even when this is expected—but not intended—to hasten death (the doctrine of double effect).19
The information above relates to the law. Physicians must comply with the laws of their country. A medical decision, however, may be legal yet unethical. We believe that the confusion between ethical principles and legal obligations that exists in the minds of many physicians can distort the decision-making process. When decisions to forego life-sustaining treatment are entirely based on standardized criteria, which comply with the law but ignore the specific factors characterizing each individual patient,134 they may produce deleterious effects, ranging from loss of opportunity to treat to administration of useless treatments. Furthermore, the confusion between ethical and legal obligations may hinder openness in communicating decisions; for instance, physicians may be reluctant to record the nature and implementation of a decision to forego life-sustaining treatment in the patient’s medical record.135
When decisions to forego life-sustaining treatment are made, fewer than 5% of patients are able to participate in the discussions or decisions.136 In addition, patient preferences are usually not known.20 Consequently, intensivists have turned to families as the primary partners for initiating a decision to forego life-sustaining treatment. The patient may be represented by a surrogate decision maker holding a durable power of attorney for health care; if the patient has not designated a surrogate, the intensivists discuss decisions with family members. The person representing the patient is asked for advice in some countries130,137 and for decision-making input in others.19,138 Whether the information on patient wishes used to make a decision to forego life-sustaining treatment in patients receiving mechanical ventilation should be obtained from family members has been challenged. Many families do not understand what is at stake;139 have no knowledge of the patient’s wishes;140 want, but do not have, written instructions from the patient;141 have opinions that disagree with patient wishes;142 and, most importantly, suffer a burden of stress and anxiety that may impair their decision-making capacities.37
Advance directives have been suggested as a means of allowing patients to remain in control of their care, even when they have lost their decision-making capacity, as is the case for intubated patients in the ICU.143 Unfortunately, a complex set of reasons144 impairs the effectiveness of advance directives in ensuring that patient wishes are honored145 and that treatments given in the ICU or wards are changed in accordance with patient instructions.68,146 In addition, patients may change their minds over time, so that advance directives may no longer reflect their wishes at the time decisions to forego life-sustaining treatment are made.68,144–147 Interestingly, a 1990 survey among members of the American Thoracic Society found that one-third of respondents provided care that contradicted the wishes of patients and surrogates, and that more than 80% unilaterally made and implemented a decision to forego life-sustaining treatment, at times over the objections of patients and surrogates.92 Finally, the SUPPORT investigators found that 10% of older inpatients with serious illnesses received care they did not want49 and that advance directives or families’ wishes were often disregarded.50 Having a specifically trained nurse talk to the patients, families, physicians, and other hospital staff members failed to improve compliance with patients’ wishes.50
The Decision-Making Procedure: High Complexity, High Stakes
Evaluating the prognosis is the key issue: When continuing mechanical ventilation and other aggressive interventions that may ensure recovery from the acute life-threatening event that prompted ICU admission, full care must be provided, without which the patient may suffer a loss of chance. Therefore, intensivists must be able to identify those patients whose chances of recovery are virtually nonexistent. For these patients, aggressive care, far from inducing benefits, prolongs the dying process, puts the patient’s dignity in jeopardy, and hinders the bereavement process for family members. Clearly, the stakes are extraordinarily high for all concerned with the decision, who must achieve a consensus about what to do and how to do it.
Because decisions to forego life-sustaining treatment force patients, families, and health care professionals to stand very close to the line that separates killing from allowing patients to die, they carry a destructive power that must be acknowledged and kept under control. To this end, intensivists have worked on developing decision-making procedures that maximize objectivity, legitimacy, serenity, and agreement among all those involved. Two main factors govern a decision to forego life-sustaining treatment: the imminence of death and the patient’s wishes regarding life support. The first factor was investigated by pursuing two avenues concomitantly: one consisted in defining futility, a concept based on clinical experience, and the other in developing mortality-prediction tools based on physiologic disturbances or organ failures. These efforts were intended to assist in objectively identifying situations that warrant a decision to forego life-sustaining treatment; however, they failed to reduce the complexity of the decision-making process. The second factor, patient wishes, faced a major obstacle: The inability of most patients to express their wishes at the time a decision to forego life-sustaining treatment is considered.10,20,73 To ensure that patient wishes would nevertheless be honored, three approaches were suggested: advance directives, formal designation of a surrogate decision maker holding a durable power of attorney, and family participation in decisions.
Predicting mortality has relied chiefly on severity scores developed in the United States and Europe148–151 to characterize patients (based on age, chronic morbidities, recruitment type, and severity of each organ involvement) and to constitute homogeneous patient groups (i.e., groups with a similar risk of hospital death). These scores have proved useful for measuring the performance of ICUs (via determination of the standardized mortality ratio [SMR]) and for establishing homogeneous patient groups for inclusion in therapeutic trials. Their poor calibration and discrimination, however, make them unhelpful for predicting the risk of death in the individual patient. Furthermore, because these scores are determined at a single point in time (ICU admission) and developed in a given population, they fail to reflect changes in organ failures over time152,153 or advances made in the management of a specific condition.154 Therefore, mortality-prediction scores are of no assistance in deciding when treatment withholding or withdrawal is appropriate.
Futility is a concept that was widely used to determine that a decision to forego life-sustaining treatment was appropriate. The patient-benefit-centered view defines futility as use of interventions that are unlikely to benefit the patient.155 We prefer the definition suggested by Schneiderman et al in 1990: “When physicians conclude (either through personal experience, experiences shared with colleagues, or consideration of published empiric data) that in the last 100 cases a medical treatment has been useless, they should regard that treatment as futile,” and “if the likelihood of functional recovery after a proposed course of therapy is less than 1%, then physicians may assert the prerogative to withdraw therapy without the consent of the patient or surrogate decision maker.”156
The concept of futility has been fiercely criticized. Its opponents argue that the definition of futility is neither clear nor reproducible, the concept is clearly intended to increase the power of the physician while undermining patient autonomy, treatment data do not necessarily apply to an individual patient, the 1% cutoff is not supported by scientific evidence, and the use of futility allows physicians to make decisions unilaterally.157,158 The futility debate ultimately condenses into a conflict in which patients or families and physicians disagree about the patient’s right to receive a treatment that is highly unlikely to succeed. The futility concept fails to acknowledge the huge amount of excellent work done by ICU professionals to involve families in the decision-making process and to recognize the emotional and social problems raised by family participation in decision making.29,30 Rather than speak of the physician’s right to withhold or withdraw treatment, we should speak of the physician’s duty to prepare the ICU team and the family for a clearly identifiable shift from curative care to care aimed at optimizing patient comfort and dignity while alleviating distress in the family members.159 ICU teams must move beyond the futility debate toward a position firmly rooted in a care, an ethic that gives a meaningful role to all staff members (physicians, nurses, and other health care professionals) in organizing the decision-making process with the patients and families, while interfacing with health care institutions, third-party payers, and, the general public.160

Full access? Get Clinical Tree