Terminal Nerve Blocks
A. Axillary Block
Ralf E. Gebhard
axillary block is completed by a subcutaneous infiltration at the medial aspect of the upper arm at a high humeral level to block intercostobrachial nerve fibers.
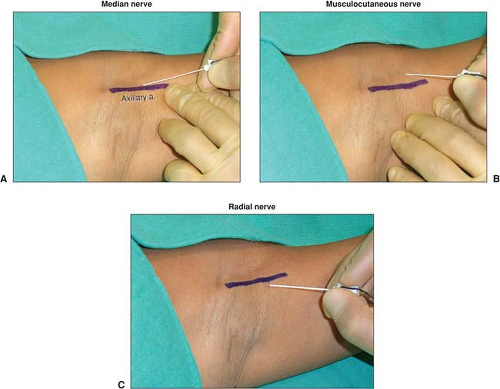 Figure 8-1. A. Indicating an Axillary artery response, B. Indicating a Musculocutaneous nerve response and C. Indicating a Radial nerve response. |
A separate stimulation and injection of the ulnar nerve has been shown to be unnecessary for a complete axillary block. if an ulnar nerve response (adduction of the thumb and the little finger) is encountered during the performance of an axillary block, 5 to 10 mL of local anesthetic can be injected after the response is maintained below 0.5 mA.
If one of the nerves is not completely blocked with this approach, the block can be easily completed by an injection at the midhumeral or elbow level after stimulating the nerve in question.
The radial nerve is probably the most difficult nerve to stimulate and block when performing an axillary block. Injecting after eliciting a distal twitch (wrist or finger extension) has been demonstrated to yield a higher success rate than accepting a proximal twitch (forearm extension).
Distal digital pressure has been shown not to promote proximal local anesthetic spread and is therefore not necessary.
Axillary blocks significantly reduce the incidence of complex regional pain syndrome after Dupuytren’s contracture surgery, when compared with general anesthesia or intravenous regional anesthesia with lidocaine.
Suggested Readings
Horlocker TT, Kufner RP, Bishop AT, et al. The risk of persistent paresthesia is not increased with repeated axillary block. Anaesth Analg 1999;88:382–387.
Koscielniak-Nielsen ZJ, Rotboll Nielsen P, Sorenson T, et al. Low dose axillary block by targeted injections of the terminal nerves. Can J Anaesth 1999;46:658–664.
Reubben SS, Pristas R, Dixon D, et al. The incidence of complex regional pain syndrome after fasciectomy for Dupuytren’s contracture: a prospective observational study of four anesthetic techniques. Anesth Analg 2006;102:499–503.
Schroeder LE, Horlocker TT, Schroeder DE. The efficacy of axillary block for surgical procedures about the elbow. Anesth Analg 1996;83:747–751.
Sia S, Bartoli M. Selective ulnar nerve stimulation is not essential for axillary plexus block using a multiple stimulation technique. Reg Anesth Pain Med 2001;26:12–16.
Sia S, Lepri A, Magherini M, et al. A comparison of proximal and distal radial nerve motor responses in axillary block using triple stimulation. Reg Anesth Pain Med 2005;30:458–463.
Sia S, Lepri A, Ponzecchi P. Axillary brachial plexus block using peripheral nerve stimulator: a comparison between double- and triple-injection techniques. Reg Anesth Pain Med 2001;26:499–503.
B. High Humeral Block
Louis-Jean Dupre
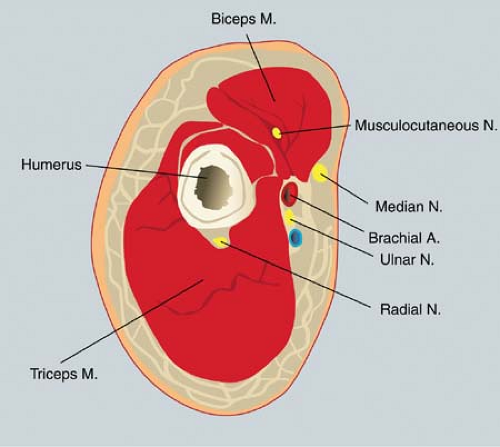 Figure 8-2. At the level of the brachial canal, the median, ulnar, radial, and musculocutaneous nerves are dispersed around the brachial artery. |
is increased to 5 mA, and the needle is redirected in search of the ulnar nerve (Fig. 8-3B). The stimulation of the ulnar nerve induces a contraction of the flexor carpi ulnaris (flexion of the little finger and opposition of the little finger and thumb). Once this response is obtained, the position of the needle is adjusted to maintain the same motor response with a current of 0.3 to 0.5 mA. Then, 8 mL of local anesthetic is injected slowly. Next, the needle is withdrawn to the skin, the current is increased to 5 mA, and the needle is redirected in search of the radial nerve (Fig. 8-3C). The stimulation of the radial nerve induces a contraction of the extensor muscles, including the extensor radialis (extension of the fingers and especially the thumb). Once this response is obtained, the position of the needle is adjusted to maintain the same motor response with a current of 0.3 to 0.5 mA. Then, 8 mL of local anesthetic is injected slowly. To block the musculocutaneous nerve, the needle is withdrawn to the skin and reintroduced in a superior and posterior direction toward the coracobrachialis muscle. The stimulation of the musculocutaneous nerve (Fig. 8-3D) induces contraction of the biceps muscle (flexion of the forearm). Once this response is obtained, the position of the needle is adjusted to maintain the same motor response with a current of 0.3 to 0.5 mA (Fig. 8-4). Then, 5 mL of local anesthetic is injected slowly. After disconnection of the nerve stimulator, 3 mL of local anesthetic is injected subcutaneously medially and laterally to the brachial artery to block the medial cutaneous nerve of the arm and the medial cutaneous nerve of the forearm.

Full access? Get Clinical Tree






