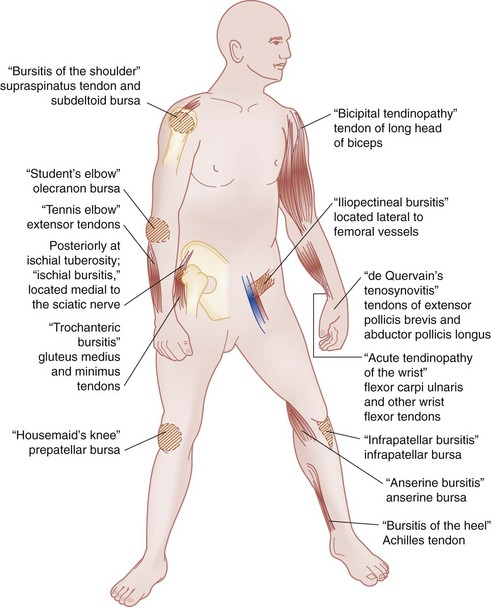
Chapter 117 Emergency physicians may see a wide variety of patients with tendinopathies due to overuse and injury given the increased participation of people in athletics and fitness.1 Approximately half of all sports participants will be injured at some time, and of these injuries, up to half will involve a tendinopathy. Tendinopathies have been implicated in approximately 40% of tennis injuries, and between 37 and 79% of participants in running will suffer an injury, with most of these injuries related to overuse.1,2 In the workplace, the incidence of work-related musculoskeletal disorders is higher in occupations that involve repetitive motion, localized contact stress, awkward positions, vibrations, and forceful exertion. Ergonomic and medical intervention programs may reduce the incidence of work-related injuries.3 Complicating the acute pain and functional limitations, tendinopathies often become chronic and can be disabling. Patients may have symptoms for extended periods despite appropriate therapy. The management of tendinopathy focuses on identification of the cause of discomfort; elimination of sources of primary tendinopathy; institution of treatment modalities, such as analgesic medication, protection, relative rest, application of ice, compression, and elevation as necessary; modification of behavior to minimize or to eliminate sources of continuing irritation; and, importantly, referral for appropriate follow-up care and early rehabilitation.4,5 Tendons are collagenous structures that connect muscle to bone. They transmit the forces originating in the muscle to the bone, which enables joint motion. The diagnosis of tendinitis, a commonly used term implying an “inflammation of the tendon,” has long been attached to many overuse injuries. Many practitioners now advocate use of the term tendinosis as a more accurate reflection of the pathologic process, given that histologic findings consistent with inflammation are not clearly evident in pathoanatomic studies. Although it has been noted that reliable, well-conducted epidemiologic studies have not been performed for most tendinopathies, the histopathologic substratum, in many cases, is degenerative.1 The term tendinopathy is used throughout this chapter to refer to the impaired tendon, as it encompasses the variety of pathologic processes. Mechanical overload and repetitive microtrauma to the musculotendinous unit are thought to be the major precipitating causes of most tendinopathies. This is a result of extrinsic and intrinsic factors that modify the pathophysiologic state. Intrinsic factors, such as age, gender, malalignment, joint laxity, muscle weakness, and imbalance, can result in excessively high or frequent mechanical loads during normal activity. Extrinsic factors, such as ergonomics, abnormal movements, excessive duration of activity, and increased frequency or intensity of activity, can also contribute to the development of a tendinopathy. Many injuries have a multifactorial origin.6 An increased incidence of tendinopathy and tendon rupture, particularly of the Achilles tendon, is reported in patients taking fluoroquinolone antibiotics, particularly in individuals receiving steroid treatment or those with renal disease.7 The pathophysiologic mechanism of tendon healing has mainly been described in the literature in the context of acute injury (e.g., rupture), and correlation to the healing process in tendinopathies remains unclear. Acutely injured tendons go through several stages in the healing process, and it may take 6 to 12 weeks for structural organization and collagen cross-linking to return the tendon to its preinjured strength.8 As the healing process ensues, unrestricted activity is generally avoided. However, atrophy associated with immobilization should also be avoided because the strength in healing tendons and ligaments increases faster when controlled forces are applied. Consequently, flexibility forces, eccentric strength training, and a measured return to resistive exercises have been suggested as long as pain is not produced. Most patients with overuse tendinopathies fully recover within 3 to 6 months.9 In summary, a prescription for good follow-up with proper rehabilitation is important in caring for the patient with tendinopathy. Some areas with common presentations of tendinopathies are diagrammed in Figure 117-1. The history of the patient presenting with a tendinopathy can be variable, although certain clinical aspects are characteristic. A recent history of repetitive stress may be obtained by inquiring about changes in sports or other recreational activities, work activities, or changes in the workplace. Many patients initially report no such changes, but when they are prompted to consider activities during several weeks or months (including sports equipment used, workplace ergonomic features, protective boots, or other features), a potential inciting change or activity may be elicited. On occasion, no cause is identified for an inciting mechanical overload. A history of fluoroquinolone therapy, infectious disease, or other systemic illness should also be obtained as initial presentations of rheumatologic disorders or infections, such as those from Mycobacterium, have been described.7,10–12 Pain is the most common symptom of the patient who presents with tendinopathy. Increasing discomfort, nonradiating, at the site of the affected tendon is a general symptom.4 The discomfort is frequently described as more severe subsequent to periods of rest. Unlike the discomfort of morning stiffness associated with arthritis, the pain of tendinopathy may resolve after initial movement, only to be manifested as a throbbing pain after completion of exercise. The patient may have had prior similar episodes. Continued episodes may be accompanied by an increased severity in pain. Consequently, it may be helpful to know whether a diagnosis was made (and how) and which treatment rendered (if any) was successful. In the evaluation of the patient with a tendinopathy, a thorough, directed musculoskeletal examination yields important information. Inspection searching for signs of edema, effusion, erythema, atrophy, deformity, symmetry, or trauma can be helpful. Palpation of the tendon, noting warmth or evidence of crepitation on movement, is important. Evidence of tenderness over the tendon, especially localized, reproducing the patient’s pain should be elicited.4 Underlying bone tenderness (and consideration of other differential diagnoses, including avulsion fracture and osteomyelitis) should be assessed as well. Motor function, particularly passive and active range of motion (and symptoms elicited during the examination), strength (and evidence of weakness or pain), and joint involvement and stability should be noted. In narrowing the diagnosis, it is important to determine whether the source of pain is articular (within the joint capsule) or periarticular (around the joint capsule). In general, arthritis produces generalized joint pain, warmth, swelling, and tenderness. The discomfort of arthritis increases with both passive and active motion of the joint. In contrast, the pain of a tendinopathy tends to be more localized.4 Tenderness and swelling do not occur uniformly across the joint, and pain may be produced only with certain movements, most commonly with resisted active contraction or passive stretching of the affected muscles or tendons. Shoulder.: Tendinopathies of the shoulder joint include impingement syndrome, which includes subacromial bursitis or rotator cuff tendinopathy, bicipital tendinopathy, calcific tendinopathy, and adhesive capsulitis. Impingement Syndrome and Rotator Cuff Tendinopathies.: The shoulder joint is predisposed to soft tissue injury because of its extensive range of motion and unique anatomic structure. Although it is inherently unstable, the muscles of the rotator cuff (supraspinatus, infraspinatus, teres minor, and subscapularis) and the glenohumeral ligaments serve to stabilize the joint. The muscles of the rotator cuff originate from the scapula (hence their nomenclature), and their tendinous insertion is found on the fibrous capsule of the glenohumeral joint after traversing through the subacromial space. The presence of the subacromial bursa, as for all bursae, serves to ensure fluidity of movement, but it may become inflamed as a part of an impingement syndrome.13 Impingement of the tendons occurs because of their unique position interposed between the humeral head and the acromion, which may predispose to a chronic tendinopathy. The functional arc of the elevated shoulder is forward and in the anterior plane. As a result of this position, the greater tuberosity of the humerus may compress (impinge) the tendons of the rotator cuff (usually the supraspinatus) against the undersurface of the anterior third of the acromion. Because of the insertion of the tendon of the long head of the biceps, it too may be involved as part of the impingement syndrome.13 Development of this tendinopathy may be a result of overuse of the extremity that leads to microtrauma of the tendinous fibers, or it may be due to individual anatomic differences (congenital or from the process of aging, such as osteophytic changes) that predispose to tendinopathy, or both. Other entities that may coexist and complicate an impingement syndrome include subacromial bursitis, bicipital tendinopathy, and calcific tendinopathy.14 More than 30 years ago, Neer noted that 95% of rotator cuff tears are associated with impingement (excluding tears due to a one-time traumatic event). He described three progressive stages of the impingement syndrome as a result of overuse.15 The first stage is frequently seen in athletes younger than 25 years who participate in sports that require repetitive overhead motions of the shoulder (e.g., swimming and baseball).15,16 It is characterized by edema and hemorrhage within and around the tendon. The pain is usually described as a dull ache over the anterolateral shoulder, extending from the shoulder to the middle upper arm, often occurring after an activity involving flexion and abduction of the arm. Point tenderness may be elicited over the greater tuberosity. No weakness or loss of motion is generally present. This condition is generally believed to be reversible with appropriate treatment. In the second stage, as mechanical trauma continues, fibrosis and thickening of the tendon and subacromial bursa can occur. This generally affects patients between 25 and 40 years of age. The pain becomes constant and may worsen at night. Active motion may be limited by pain, and any activity involving overhead movement exacerbates the symptoms. Passive range of motion should be preserved, and on physical examination, pain is more diffuse and intense. The third stage has symptoms similar to those of the second stage but may involve a prolonged history of shoulder problems. The range of motion of the shoulder is usually decreased because of either disuse or a partial rotator cuff tear. On pathologic examination, tendon degeneration and attrition may be present. Partial-thickness tears may occur or extend with minor trauma or stress. Complete tears of the rotator cuff, biceps tendon rupture, and osteophytic bone changes are sometimes seen. Physical examination in the evaluation of a rotator cuff tendinopathy includes maneuvers that can exacerbate the symptoms of impingement.17 Because the supraspinatus tendon is most often involved, a physical examination sign (sometimes referred to as Jobe‘s sign, after Frank Jobe, team physician of the Los Angeles Dodgers, or the empty can test, describing the position of emptying aluminum cans) is helpful in assessing the supraspinatus tendon with resistance testing. With the arms abducted at 90 degrees in the scapular plane (30 degrees anterior to the coronal plane), the arms are internally rotated with the thumbs pointed downward. The examiner places a downward force on the arms, and the patient is instructed to resist the examiner and to keep the arms parallel to the floor. Weakness or pain is considered a positive finding. If the patient is unable to resist the force of the examiner, supraspinatus weakness should be suspected. A complete rotator cuff tear is evaluated by the drop arm test, in which the arm is passively abducted at 90 degrees and the patient is asked to maintain the abduction. If the arm drops to the side, a large rotator cuff tear should be considered.17 The shrug sign is exhibited when a patient with acute macrotrauma to the rotator cuff is asked to abduct the arm at 90 degrees and appears to be giving a shrug with that side. This movement results from the scapula’s attempting to abduct the arm without the assistance of the rotator cuff. Although this has historically been associated with rotator cuff disease, it is somewhat nonspecific and can be associated with other shoulder disease.18 Patients with adhesive capsulitis (frozen shoulder) have limitation of active and passive range of motion.19 Bicipital Tendinopathy.: The tendon of the long head of the biceps, given its insertion into the humerus in proximity to the rotator cuff, can be associated with the impingement syndrome. The patient with bicipital tendinopathy may report pain in the anterior shoulder that radiates down to the radius. Discomfort occurs when the individual rolls on the shoulder at night or attempts to reach a hip pocket or a back zipper. Focal tenderness can be obtained by palpation in the groove between the greater and lesser tuberosities of the humerus while testing for Yergason’s sign, which is elicited by having the patient flex the elbow to 90 degrees with the arm against the body and resisting supination of the forearm. Pain in the area of the proximal tendon is considered to be a positive finding and indicative of bicipital tendinopathy.17 Another physical examination tool in the diagnosis of bicipital tendinopathy is the Speed sign. With the elbow extended and the forearm supinated, the patient is instructed to resist forward flexion of the adducted shoulder at 60 degrees. Pain in the area of the proximal biceps tendon (bicipital groove) is indicative of a positive finding. This may also be suggestive, however, of labral disease.20 Calcific Tendinopathy.: Calcific tendinopathy is an acute or chronically painful condition associated with deposition of calcium crystals that occurs in or around the tendons of the rotator cuff. The cause is unknown but has been postulated to be related to tissue hypoxia and degeneration due to overuse.21 Although it can affect any of the rotator cuff tendons, it seems to have a predilection for the supraspinatus. The symptoms are similar to those of an impingement syndrome, and the condition generally affects people older than 40 years. Calcium deposition occurs over time and then undergoes spontaneous resorption. This resorptive phase is thought to be the painful aspect, but the severity of the symptoms is not related to the size of the deposit. Pain is believed to be in response to the local chemical pathologic disorder and direct mechanical irritation.22 On physical examination, there may be specific tenderness over the greater tuberosity as well as symptoms consistent with impingement. Radiographic evaluation may show evidence of calcification in or around the rotator cuff tendons (Fig. 117-2). The presence of calcium in the tendon does not necessarily affirm the origin of the pain because asymptomatic patients may have evidence of calcification on a routine radiograph.22 Elbow.: Increasingly, athletes of all ages and skill levels are participating in sports involving overhead arm motions; consequently, elbow injuries are increasingly seen.23 From an anatomic and functional perspective, the extensors and supinators of the wrist attach to the lateral elbow, and the flexors and pronators attach medially. Lateral Epicondylitis.: Lateral epicondylitis (“tennis elbow”) is a painful elbow condition that occurs at the insertion of the common extensor tendon (extensor carpi radialis brevis) onto the lateral epicondyle of the humerus. Although it occurs in many tennis players, epidemiologic studies suggest that less than 5% of patients with such a syndrome actually play tennis. Activities such as driving in screws, use of a wrench, and repetitive work on an assembly line have also been implicated. Symptoms often begin as a dull ache on the outer (lateral) aspect of the elbow.24,25 The discomfort can be exacerbated by activities that involve extension or supination of the wrist, such as grasping and twisting. Cozen’s test is performed by having the patient keep the fist clenched while extending the wrist. The examiner grasps the forearm with the left hand while the right hand pulls the patient’s hand toward flexion against the patient’s resistance. A positive finding is pain at the lateral epicondyle, reproducing the patient’s symptoms.26 Active extension of the long finger against resistance with the elbow in extension can also reproduce the pain over the lateral epicondyle at the insertion of the extensor carpi radialis brevis. In addition, patients will typically have tenderness to palpation just distal to the lateral epicondyle, over the origin of the extensor carpi radialis brevis.26 Radiographs can be helpful in cases with atypical or prolonged symptoms and to rule out other pathologic conditions. Approximately 20% of patients demonstrate tendon calcification or a reactive exostosis at the tip of the epicondyle.24 The differential diagnosis of lateral epicondylitis includes posterior interosseus nerve entrapment (motor aspect of radial nerve in forearm). Other associated lesions include plica, synovitis, chondromalacia, and adolescent osteochondral defect.24 Medial Epicondylitis.: The pain of the less common medial epicondylitis (“pitcher’s elbow” or “golfer’s elbow”) can result from microtrauma at the site of the insertion of the flexor carpi radialis on the medial epicondyle. It is important to differentiate medial epicondylitis from other causes of medial elbow pain, including medial ulnar collateral ligament injury. As a result of repetitive valgus stress placed on the joint, microtraumatic injury and valgus instability at the ligament can occur. With disruption of the medial ulnar collateral ligament, abnormal stress is placed on the articular surfaces, which may lead to degenerative changes and the formation of osteophytes.27 In the case of medial epicondylitis, patients will generally have tenderness over the flexor-pronator origin slightly distal and anterior to the medial epicondyle. Pain can be reproduced by having the patient attempt wrist flexion and forearm pronation against resistance.28 de Quervain’s Tenosynovitis.: The wrist and hand comprise several tendons that pass through thick, fibrous retinacular tunnels. These help prevent subluxation of the tendons and act as a pulley system. Overuse syndromes are thought to result from changes of the synovial lining between these tendons and retinaculum. de Quervain’s tenosynovitis involves the synovial lining of the abductor pollicis longus and extensor pollicis brevis. Although the term tenosynovitis indicates an inflammation of the tendon sheath, it has been noted that there are many potential forms of tenosynovitis. Classic acute inflammatory changes that are characteristic of tenosynovitis may be related to systemic manifestations of disease (e.g., rheumatoid arthritis and gout); tenosynovitis related to de Quervain’s syndrome is referred to by some practitioners as stenosing tenosynovitis. The pathologic process of de Quervain’s tenosynovitis does not generally involve inflammation because the primary change is thickening of the extensor retinaculum covering the first dorsal compartment of the wrist. It has been suggested that de Quervain’s disease is a result of intrinsic degenerative mechanisms rather than extrinsic inflammatory ones.29 The history may consist of chronic, repetitive trauma or unaccustomed repetitive efforts, such as firm grasping and movement of the hand in a radial direction. Direct trauma, such as a direct blow or fall, has occasionally been implicated.30 The discomfort of de Quervain’s tenosynovitis can be localized over the radial styloid process. Radiation of pain proximally to the forearm or distally down the thumb has been noted. The pain is generally constant but may be exacerbated by maneuvers that include grasping, abduction of the thumb, and ulnar deviation of the wrist. In most cases of de Quervain’s tenosynovitis, the onset is gradual and not associated with a history of acute trauma.
Tendinopathy and Bursitis
Tendinopathy
Principles of Disease
Clinical Features
Specific Tendinopathies

Full access? Get Clinical Tree


Tendinopathy and Bursitis
Only gold members can continue reading. Log In or Register to continue