I. GENERAL PRINCIPLES
A. Background.
1. The purpose of temporary cardiac pacing is to reestablish circulatory integrity and normal hemodynamics in acutely compromised bradyarrhythmia or tachyarrhythmia by maintaining an appropriate heart rate until it resolves or until long-term therapy can be initiated.
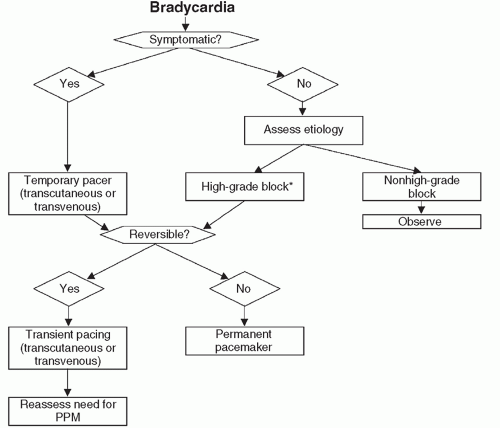
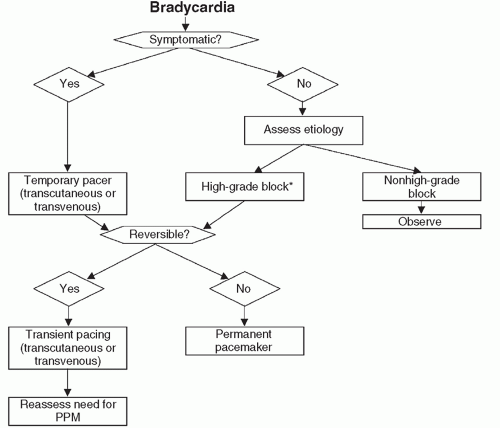
2. Algorithm for managing patients with bradycardia (
Fig. 37-1).
B. Pacing options.
1. Transcutaneous.
a. Primary use: prophylaxis in patients at risk for high-grade atrioventricular (AV) block.
b. Pros: multifunctional capabilities including sensing; can be used for overdrive pacing.
c. Cons: patient discomfort, adequate ventricular capture may be challenging.
2. Transvenous: has commonly supplanted transcutaneous pacing given ease of use and less patient discomfort.
II. INDICATIONS
A. Overview.
1. Indications for temporary pacing in the setting of acute myocardial infarction (MI) have been well defined and outlined in a consensus guideline from American Heart Association and the American College of Cardiology (AHA/ACC) (see
Table 37-1).
2. No similar guidelines available for other conditions causing bradycardia (i.e., electrolyte abnormalities, drug reactions, or infections).
3. Of patients needing temporary pacing, about half require permanent pacing before discharge.
B. Specific indications.
a. Bradycardia/AV block related to ischemia or infarction of conduction system.
i. Revascularization is the primary management—in particular when AV nodal or fascicular blood supply is compromised.
(a) Inferior ischemia (disruption of AV nodal blood supply).
(b) Anterior ischemia (disruption of fascicular blood supply).
ii. Prognosis.
(a) Depends on extent of underlying ischemia and LV function.
(b) Death is rare from complete heart block.
a. The most common indication is symptomatic bradycardia that is unresponsive to pharmacologic therapy.
b. Classifications.
i. Disordered impulse formation (i.e., sinus node dysfunction).
ii. Disordered impulse propagation (i.e., conduction block).
a. Temporary pacing rarely used in clinical practice due to efficacy of medications and increased prevalence of implantable defibrillators.
b. Pacing can play a role in prevention or termination of arrhythmia.
c. Many reentrant rhythms are susceptible to pace termination.
i. Supraventricular tachycardia (SVT) (AV nodal reentrant tachycardia, accessory pathway-mediated tachycardia).
ii. Ventricular tachycardia (VT) (scar mediated).