ANESTHESIA TECHNIQUES: (GOALS)
• Monitored anesthesia care (MAC): Anxiolysis, sedation, analgesia & monitoring by anesthesia personnel able to anticipate and react to changes in pt status & anesthetic state/requirements
• General anesthesia: Pt unresponsive to significant stimulation; often requires airway, ventilatory, and/or cardiovascular support
• Neuraxial techniques: Spinal/epidural alone or combined with above techniques for intraop & postop analgesia to chest, abdomen, & lower extremity
• Peripheral nerve block: Minimal physiologic effects make these techniques useful, especially in a pt with significant comorbidities.
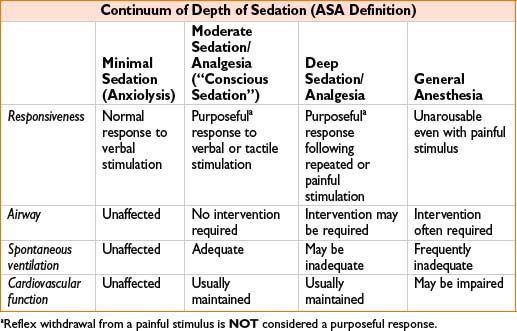
MONITORED ANESTHESIA CARE VS. GENERAL ANESTHESIA: ASA DEFINITIONS
• MAC: Anesthesia service that involves varying depths of sedation, analgesia, & anxiolysis but, most importantly, requires that provider is “prepared & qualified to convert to general anesthesia when necessary.”
• General anesthesia: State when “patient loses consciousness & the ability to respond purposefully … irrespective of whether airway instrumentation is required”
FLUMAZENIL (FOR ANTAGONISM OF BENZODIAZEPINE EFFECTS)
• Initial recommended dose = 0.2 mg
• If desired level of consciousness not achieved in 45 sec, repeat 0.2 mg dose
• 0.2 mg dose may need to be repeated q60sec to max of 1 mg
• Note: Be aware of potential for resedation due to short half-life
INHALATIONAL INDUCTION
• Allows induction without IV access, as IV placement can be anxiety-provoking
• Onset of anesthesia faster in children than in adults (ratio of alveolar ventilation to FRC is in inverse proportion to body size; i.e., infants & children have increased ratio of alveolar ventilation to FRC)
Pediatric Technique
• For infants & children who tolerate a mask:
• Start with 70% nitrous oxide in mask on pt
• Introduce volatile agent only after 3 to 5 min of N2O/O2
• Cut back N2O and increase O2 percentage as potent agent is added
• For anxious children—rapid induction (in as few as 4 breaths):
• Often requires involvement of multiple personnel and/or parents
• Prime circuit with 70% N2O, O2 & 8% sevoflurane
• Place mask firmly on pt while monitoring airway throughout
• With loss of consciousness, increase percentage of O2 & decrease N2O
• Decrease sevoflurane conc over next few minutes as agent equilibrates
• Support ventilation as needed
• Place IV (often with an assistant to assure appropriate attention to airway)
Note: Sevoflurane induction has been associated with bradycardia, especially in patients with Down’s syndrome [J Clin Anesth. (22):8, Dec 2010, 592–597]
Adult Inhalational Induction
• Consider for adults in whom IV placement is extremely anxiety-provoking/difficult
• Disadvantages: May cause ↑ cough, hiccups, & possibly ↑ risk of nausea/vomiting
• Prime circuit with 8% sevoflurane & 70% N2O (usually requires 3 fill/empty cycles of an occluded anesthesia circuit)
• Instruct pt to exhale completely & then inhale from mask to vital capacity & hold
• If still conscious & unable to hold breath any longer, instruct pt to take additional deep breaths
INTRAMUSCULAR INDUCTION
• May be useful technique for:
• Uncooperative pts in whom IV placement/inhalation induction impossible
• Loss of control of pt and/or airway during attempted inhalation induction
• Agitation/disinhibition with premedication
• Need for rapid sequence induction without venous access
• Typical IM dosing:
• Ketamine 6.5–10 mg/kg, 10% solution
• Atropine 0.02 mg/kg, to reduce secretions
• Succinylcholine 3–4 mg/kg, included for rapid sequence induction
Note: Atropine & succinylcholine may be combined in same syringe; administer midazolam after IV placement to prevent ketamine emergence delirium
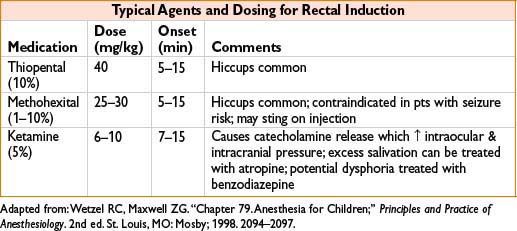
RECTAL INDUCTION
Characteristics
• Convenient for healthy children old enough to have separation anxiety but still not mature enough to cooperate (8 mos to 5 yrs/o)
• Parents & child familiar with rectal route for other medications (i.e., acetaminophen)
• Avoids needle for IM/IV induction & struggle involved with inhalational induction
Technique
• Cut 14-Fr suction catheter to 10 cm & lubricate
• Place catheter in pt’s rectum & administer medication through syringe
• Follow medication with air bolus to purge remaining drug from catheter lumen
• Instruct parent/caregiver to hold buttocks together for at least 2 min
• Anticipate defecation & provide caregiver with waterproof mat
• Harmless hiccupping may occur
• Constant monitoring by anesthesia personnel required throughout
• Pt should be taken to procedure area as soon as sufficient sedation achieved
• Maintain primary attention on supporting pt’s airway
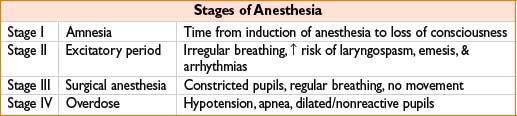
COMPONENTS OF ANESTHESIA
• An anesthetic may contain any or all of the following components: Anxiolysis, analgesia, hypnosis, amnesia, paralysis
• Inhalational & IV agents provide anxiolysis & hypnosis, little or no analgesia (except for ketamine and nitrous oxide) (Anesthesiology 2008;109(4):707–722)
• Narcotics provide analgesia, little or no hypnosis/sedation
“BALANCED ANESTHETIC” TECHNIQUE
• A technique of general anesthesia based on the concept that administration of a mixture of small amounts of several neuronal depressants summates the advantages but not the disadvantages of the individual components of the mixture
A “balance” of virtues of different agents allows less of each to be used
• Allows for faster emergence & less risk of cardiovascular collapse
• Use of muscle relaxants may increase risk of intraoperative awareness
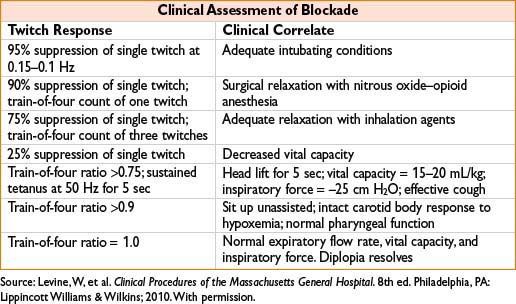
MONITORING OF NEUROMUSCULAR BLOCKADE/PARALYSIS
Technique
Peripheral nerve stimulator (PNS) electrically stimulates motor nerve adductor pollicis (ulnar n.), obicularis oculi (facial n.), posterior tibial n., peroneal n.
Train of Four
Four stimuli given at a frequency of 2 Hz every 5 sec
→ Potentially eliciting 4 twitches (T1–T4)
→ TOF ratio T4:T1 indicates degree of neuromuscular block
→ Nondepolarizing agents:
Produce progressive reduction in magnitude of T1–T4; number of elicited twitches indicates degree of blockade with recovery, twitches appear in reverse order
→ Depolarizing agents (succinylcholine):
Produce equal but reduced twitches (no fade)
Tetanic Stimulation
Tetanic stimulation: Concept that acetylcholine is depleted by successive stimulations; 50 Hz for 5 continuous seconds produces detectable fade in muscle contraction
→ The extent of fade is related to the degree of neuromuscular block
→ No fade = no neuromuscular block
→ Sustained response to tetanus present when TOF ratio is >0.7
Double-Burst Stimulation
• Two bursts of three stimuli at 50 Hz with each triple burst separated by 750 ms
• Decrease in second response indicates residual block
• Ratio is related to TOF ratio but easier to interpret reliably
Post-Tetanic Count
• 50 Hz tetanic stimulus given for 5 sec, followed by stimulus at 1.0 Hz 3 sec later
• No. of responses detectable predicts time for spontaneous recovery
• Fade response appears earlier than train of four
• Can be used under deep paralysis to estimate time to recovery and potential for use of reversal agents.
Phase II Blockade with Succinylcholine
• Postjunctional membranes repolarized, but still not responding to acetylcholine
• Resembles blockade by nondepolarizing agents (get TOF fade, tetanic stim)
• Mechanism unknown, occurs when succinylcholine dose exceeds 3–5 mg/kg IV
• Reversal agents (neostigmine) may or may not antagonize phase II blockade
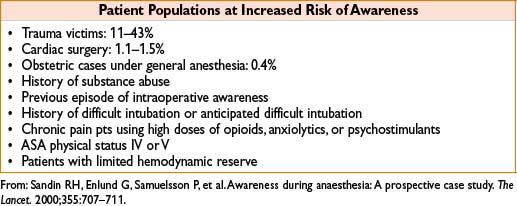
AWARENESS
• Complication where pt regains consciousness during general anesthetic & can recall events afterward. Important to distinguish goals of General Anesthesia from that of Monitored Anesthesia Care.
• Pts experience ranges from benign recall of conversation to posttraumatic stress disorder (PTSD) involving disturbed sleep, nightmares, flashbacks, & general anxiety
• Negative psychologic consequences can last for years after the event
• If awareness occurs, pts often respond favorably to a complete explanation, apology, & reassurance that they are not crazy. Psychology consult should be considered early if patient is in favor
Frequency of Awareness (from prospective study of 11,785 general anesthetics)
• 0.15% of all cases
• 0.18% with paralysis
• 0.10% without paralysis
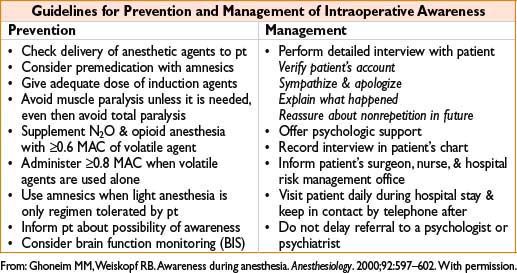
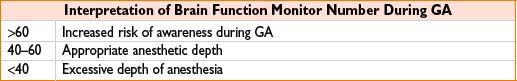
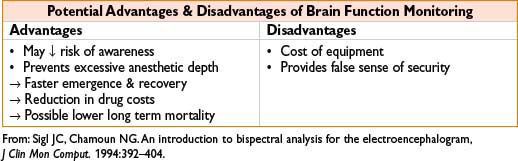
BRAIN FUNCTION MONITORING, DEPTH OF ANESTHESIA, AND AWARENESS
• Brain function monitors analyze EEG signals & translate them into a number between 0 and 100 that corresponds to anesthetic depth
• Two devices currently available (BIS from Aspect, SEDLine from Masimo)
• ASA position: BIS not routinely indicated & decision to use should be made on a case-by-case basis by individual practitioner
When compared to monitoring of the end-tidal anesthetic-agent concentration (ETAC), BIS does not appear to reduce the incidence of intraoperative awareness (N Engl J Med 2011;365:591–600, August 18, 2011)
BRAIN FUNCTION MONITORING & ANALGESIA
• Number correlates best with hypnotic component of anesthetic provided by benzodiazepines, propofol, & potent volatile agents
• N2O, low-dose narcotics & neuraxial/peripheral nerve blocks have little effect on the number (These agents do ↓ amount of additional hypnotic needed to keep the number constant when pts are exposed noxious stimuli)
• Ketamine confounds the number & contraindicates its use. Use of Nitrous Oxide (alone) may result in inaccurate correlation of BIS and level of sedation and hypnosis (A & A August 2006 vol. 103 no. 2 385–389).
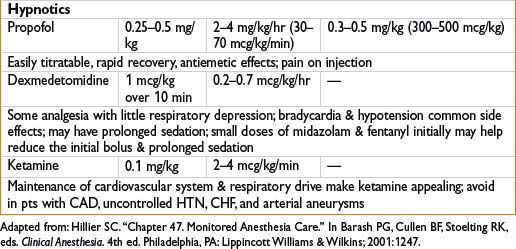
TOTAL INTRAVENOUS ANESTHESIA (TIVA)
• TIVA anesthetics usually include hypnotic (propofol) + analgesic (remifentanil)
• IV infusion drugs should be connected as closely as possible to pt’s IV catheter (Minimize dead space where infusion meds can accumulate)
• TIVA may be more susceptible to dosing errors
• Must always monitor for: IV lines that are infiltrated/kinked
Disconnections & dosing errors
Advantages of TIVA over Inhalation Induction & Maintenance
• Smooth induction with minimal coughing/hiccupping
• Easier control of anesthetic depth
• More rapid, predictable emergence
• Lower incidence of PONV
• Ideal operating conditions for neurologic surgery with reduced cerebral blood flow & cerebral metabolic rate; allows intraoperative neuromonitoring
• ↓ organ toxicity & atmospheric pollution
• Avoids N2O side effects (expansion of closed airspaces & bone marrow suppression)
Common Indications for TIVA
• Anesthesia for airway endoscopies, laryngeal & tracheal surgeries
• Anesthesia in remote locations or during transport
• Malignant hyperthermia–susceptible patients
• History of significant PONV
Advantages of Continuous Infusions Compared with Intermittent Bolus Dosing
• Avoid oscillations in drug concentration
• Minimize relative over- or underdosing
• Provide stable depth of anesthesia
• Reduce incidence of side effects (hemodynamic instability)
• Shorten recovery times
• ↓ total drug requirements by 25–30%
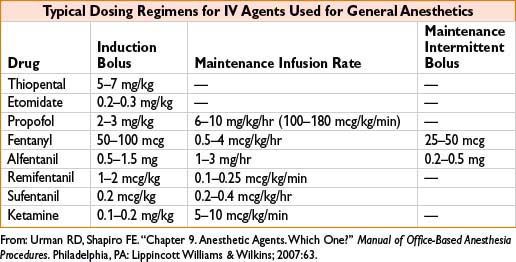
Titration of Maintenance Infusions
• Titrate to anticipated intensity of observed responses to surgical stimulus
• Drug requirements are highest during endotracheal intubation
• Requirements ↓ during surgical prep & draping
• Infusion rates should be ↑’d a few minutes before skin incision
• Pt movement & changes in hemodynamics should guide infusions titration
• After start of surgery: If no response for 10–15 min, ↓ infusion rate by 20%
if response, administer bolus & ↑ infusion rate
• Opioid should be administered to achieve analgesia
• Hypnotic should be titrated to individual requirements & surgical stimulus
• Infusion rates need to be titrated down to restore spontaneous respiration at surgery’s end
GUIDELINES FOR USING PROPOFOL
Induction of General Anesthesia
• 2–3 mg/kg IV (reduced in pts given opioids/other premeds, aged >50)
Maintenance of General Anesthesia
• 80–150 mcg/kg/min IV combined with N2O or an opiate
• 120–200 mcg/kg/min IV if sole agent
• Consider reducing dose after 2 hr (propofol accumulates)
• Turn off infusion 5–10 min prior to desired time of emergence (can give 1–2 mL boluses as needed to keep pt asleep until emergence)
Sedation
• 10–50 mcg/kg/min IV
EXTUBATION & EMERGENCE
Common Extubation Criteria
• Regular respiratory rate
• Stable SpO2
• Adequate paralysis reversal (sustained head/leg lift for 5 sec); able to protect airway
• Tidal volumes >4 mL/kg
• Return of consciousness (following commands)
• Stable end-tidal CO2 at physiologic levels
Indications for Continued Postop Intubation
• Epiglottitis
• Localized upper airway edema secondary to surgery or trauma
• Surgery causing injury to recurrent laryngeal nerves
• Upper airway edema from massive intraoperative volume infusion (especially combined with prolonged Trendelenburg or prone positioning)
• Unstable hemodynamics or continued bleeding
• Neurologic compromise (GCS <8)
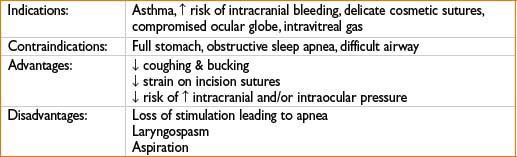
Deep Extubation

Full access? Get Clinical Tree








