Acute Renal Failure
• ↑ of Cr by ≥0.5 mg/dL or ↑ of Cr by ≥20% over 2 wks
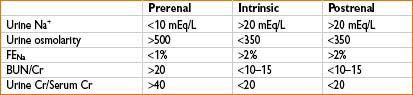
• Prerenal
• Renal hypoperfusion resulting in ↓ GFR
• Causes
• Hypovolemia, ↓ cardiac output, liver failure, sepsis
• Renal vasoconstriction (ACE/COX inhibitors)
• Intrinsic (renal)
• Damage to renal parenchyma
• Causes
• Acute tubular necrosis (ATN)—causes include ischemia & toxins (aminoglycosides, myoglobin, IV contrast)
• Acute interstitial nephritis (AIN)—usually caused by drugs (NSAIDs, b-lactams, sulfonamides, rifampin)
• Glomerulonephritis
• DIC
• TTP
• Postrenal
• Outflow obstruction (must have bilateral obstruction, unilateral obstruction if only one kidney present, kinked Foley)
• Causes
• Nephrolithiasis, BPH, prostate cancer, neurogenic bladder
• Treatment
• Treat underlying disorder
• Avoid nephrotoxic drugs
• Fenoldopam & low-dose dopamine (controversial) may help prevent or treat ARF by dilating renal arteries & ↑ RBF & GFR
• Dialysis if indicated due to:
• Acidosis
• Electrolyte disturbances (hyperkalemia)
• Intoxication (methanol, ethylene glycol)
• Volume overload
• Uremia
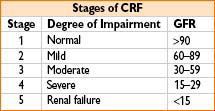
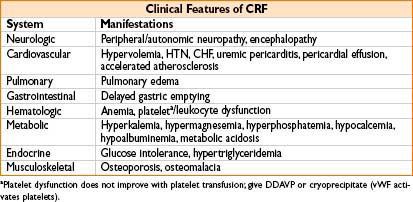
Chronic Renal Failure
• Either GFR <60 mL/min/1.73 m2 or evidence of kidney damage (abnormal urinalysis, imaging or histology) for ≥3 mos
• Causes:
• Hypertension
• Diabetes mellitus
• Glomerulonephritis
• Polycystic kidney disease
• Renovascular disease
• Treatment
• ACE inhibitors/ARBs may slow progression of diabetic renal disease
• Erythropoietin for anemia
• Dialysis as indicated (hemodialysis/peritoneal dialysis)
• Phosphate binders for hyperphosphatemia
• Renal transplantation
For a list of commonly used diuretics, see Chapter 2H-56, Clinical Characteristics of Commonly Encountered Diuretics
ANESTHESIA FOR PATIENTS WITH RENAL DISEASE
Effects of Anesthesia on Renal Function
• Reversible ↓ in RBF, GFR, urine production during regional & general anesthesia can occur despite maintenance of normal BP/volume status
• RBF & GFR will usually return to normal within several hours postop
Indirect Effects of Anesthesia
• Anesthetic agents & sympathetic blockade (during regional techniques)
→ Hypotension & myocardial depression → ↓ RBF & GFR
• Hydration before anesthesia may lessen hypotension and changes in RBF
Direct Effects of Anesthesia
• Fluorinated agents can cause direct renal toxicity (fluoride impairs kidney’s ability to concentrate urine & causes tubular necrosis)
• Fluoride production negligible with halothane, desflurane, & isoflurane
• Sevoflurane & enflurane release fluoride (no clinical evidence of renal damage)
• Sevoflurane reacts with carbon dioxide absorbents to form compound A (shown to cause renal damage in rat models)
• Low fresh gas flows should be avoided with sevoflurane (use flows of ≥1 L/min)
• Consider avoiding sevoflurane in pts with renal insufficiency (theoretical risk of nephrotoxicity)
• Common IV agents do not cause changes in GFR
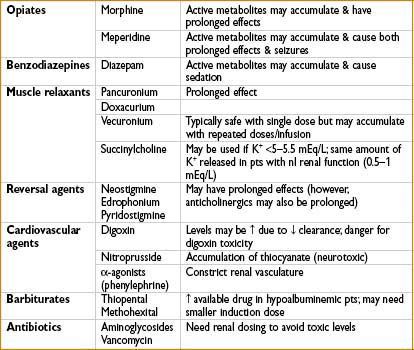
MEDICATIONS TO AVOID OR USE WITH CAUTION IN RENAL FAILURE
• Lipid-insoluble, ionized drugs, & water-soluble metabolites of hepatically metabolized drugs are renally excreted & may accumulate in renal failure
• Highly protein-bound drugs can accumulate if patient is hypoalbuminemic
UROLOGIC SURGERY
Cystoscopy/Ureteroscopy/TURBT
General Considerations
• Indications: Need for biopsies, laser lithotripsy, extraction of stones, placement of ureteral stents
• Pts commonly elderly with comorbid medical conditions
• Irrigation fluids often used to improve visualization & for flushing
• Sterile water: Hypotonic, causes hemolysis & hyponatremia when absorbed systemically; safe with electrocautery
• Nonelectrolyte solutions (glycine, sorbitol, mannitol): Slightly hypotonic, can cause hyponatremia if absorbed in large volumes; safe with electrocautery
• Electrolyte solutions (NS, LR): Isotonic, do not cause hemolysis when absorbed systemically; cannot be used with electrocautery
Anesthetic Technique
• Positioning: Lithotomy
• Usually GA, can use local/MAC/regional (T10 level necessary for instrumentation of lower GU tract), consider using LMA
• Muscle relaxation not usually necessary (consider ETT with relaxation if surgeon anticipates working near obturator nerve)
• Minimal to no postop pain; short-acting opioids (fentanyl) usually sufficient
Complications
• Peroneal nerve injury from lithotomy position (causes foot drop)
• Bladder perforation: Extraperitoneal perforation is more common; signs and symptoms include nausea, diaphoresis & inguinal, retropubic or lower abdominal pain
Transurethral Resection of the Prostate (TURP)
General Considerations
• Indications: Relief of bladder obstruction from enlarged prostate (typically BPH)
• Typically elderly pts with comorbid medical conditions
• Opening of venous sinuses may lead to absorption of large amounts of irrigation fluid (see cystoscopy above) & can result in TURP syndrome (see below); fluid absorption dependent on duration of procedure, number of sinuses opened (related to prostate size), peripheral venous pressure, & height of irrigation fluid
Anesthetic Technique
• Positioning: Lithotomy
• General or regional (T10 level necessary)
• Base choice on pt’s preference, coexisting diseases
• Regional anesthesia allows for evaluation of TURP syndrome during procedure
• Muscle relaxation not required, although patient movement should be avoided (prevent further bleeding/perforation of prostate)
• Postop pain usually not significant
Complications
• TURP syndrome
• Results from absorption of large volumes of irrigant fluid through venous sinuses of prostate
• → Hyponatremia & volume overload
• Signs/symptoms: Headache, confusion, nausea/vomiting, HTN, angina, seizures, coma, cardiovascular collapse
• May also see toxicity from absorption of irrigant solutes
• Glycine: Can cause transient blindness, seizures
• Ammonia: Can cause delayed awakening, encephalopathy
• Hyperglycinemia may result in CNS toxicity & circulatory collapse
• Treatment: Fluid restriction & diuretics to correct hyponatremia & volume overload; if pt has seizures/is comatose → consider hypertonic saline
• Bladder perforation
• Coagulopathy: Dilutional thrombocytopenia from excessive fluid absorption & DIC
• Bacteremia: Since prostate is colonized by bacteria, bacteremia may result after instrumentation
• Prophylactic antibiotics may ↓ risk of bacteremia/septicemia
Alternatives to TURP
• Medical management with alpha blockers
• Vaporization of prostate tissue with electrocautery/laser/thermocoagulation (avoid danger of TURP syndrome)
Urologic Laser Surgery
General Considerations
• Indications: Condyloma acuminatum, ureteral strictures, BPH, ureteral calculi, & superficial carcinomas of penis, ureter, bladder, or renal pelvis
• Different lasers may be used (CO2/argon/pulsed dye/Nd-YAG/KTP-532)
• Safety concerns
• Goggles should be worn by OR personnel & patient to protect eyes from an inadvertent break in laser fiber
• Lasers should be used intermittently to prevent thermal injuries
• Special masks should be worn to prevent inhalation of active HPV particles when condyloma are being treated
Anesthetic Technique
• Positioning: Lithotomy
• Local with MAC, general, or regional anesthesia
Open Prostatectomy
General Considerations
• Indications: Simple prostatectomy for BPH that cannot be resected transurethrally; radical prostatectomy for prostate cancer
• Pts often elderly with comorbid medical conditions
• Blood loss can be significant
• Retroperitoneal lymph node dissection is performed for staging in prostate cancer
• Bilateral orchiectomy may be performed in symptomatic, advanced disease.
Monitoring/Access
• Standard monitors; large-bore IV
Anesthetic Technique
Open prostatectomy
• Positioning: Supine
• Anesthesia: Regional, general, or combined general/epidural
• Epidural may ↓ blood loss, improve postop pain relief, & result in recovery of bowel function more quickly
• Experienced surgeons typically able to perform procedure under general anesthesia with minimal blood loss/small incisions
• Surgeon may ask for methylene blue/indigo carmine to assess integrity of urinary tract
• Indigo carmine: Can cause hypertension (α-agonism)
• Methylene blue: Can cause hypotension/interfere with SpO2 readings
Laparoscopic and robotic-assisted prostatectomy
• Laparoscopy +/- robotic-assisted
• Advantages: Less blood loss (vs. open), smaller incisions with less postop pain
• Positioning: Lithotomy; steep Trandelenberg
• Anesthesia: General endotracheal anesthesia
Cystectomy
General Considerations
• Indications: Simple cystectomy for benign bladder disease (hemorrhagic/radiation cystitis); radical cystectomy for invasive bladder tumors
• Pts often elderly with comorbid conditions; given the association between smoking & bladder cancer, pts may be at risk for CAD & COPD
• After cystectomy, a urinary diversion must be constructed
• → Piece of ileum can be formed into an ileal conduit (brought out to the abdominal wall as a stoma)
• → Bladder suspension more involved operation (piece of bowel is formed into a pouch & connected to the urethra)
• Significant blood & fluid loss may occur
Monitoring/Access
• Standard monitors; consider arterial line, central line given potential for large blood loss & fluid shifts; large bore IV
Anesthetic Technique
• Positioning: Supine or lithotomy
• General or combined general/epidural anesthesia
Nephrectomy
General Considerations
• Indications: Neoplasm, transplantation, chronic hydronephrosis/infection, trauma
• Pts undergoing nephrectomy for renal cell carcinoma, will undergo preop staging to determine if tumor involves IVC or right atrium
• Tumor may partially/completely obstruct IVC (reduces venous return & may cause hypotension); IVC may need to be clamped during resection
• Tumor may embolize to pulmonary vasculature (signs: ↓ SpO2, hypotension, supraventricular arrhythmias)
• Complications: Venous air embolus, diaphragmatic injury (causing pneumothorax)
• May be performed open or laparoscopically
Monitoring/Access
• Standard monitors; consider arterial line
• Large-bore IV (potential for significant blood loss)
Anesthetic Technique
• Positioning: Lateral decubitus position for retroperitoneal approach/supine for transabdominal approach
• General anesthesia or combined general/epidural anesthesia (T7–T9 level)
• Hydration to preserve renal blood flow

Full access? Get Clinical Tree








