CHAPTER 48
Superior and Inferior Hypogastric Plexus Blocks
INTRODUCTION
The hypogastric plexus is the extension of the aortic plexus in the retroperitoneal space, below the aortic bifurcation. The upper part, the superior hypogastric plexus, is located anterior to the L5 vertebral body and the sacral promontory, whereas the inferior hypogastric plexus lies within the bilateral presacral tissues on either side of the rectum at S2, S3, and S4 levels. Pain from the lower abdominal as well as the pelvic and perineal area is transmitted through the hypogastric plexus.
Chronic noncancer and cancer pain of the pelvic structures are often challenging to treat and interventional approaches may well be invaluable tools. Plancarte et al described the superior hypogastric block in 1990, and found that sympathetically mediated pain was significantly reduced or eliminated in all cases without serious complications. Although this injection was originally developed for the treatment of pelvic cancer pain, as with many procedures originally limited to the terminal cancer patient in pain, these techniques are now commonly used in the nonmalignant pain. Patients have frequently failed to respond to less invasive procedures, such as lumbar or caudal epidural injections.
INDICATIONS
The indications for performing the two types of blocks have some overlap. A diagnostic block of the hypogastric plexus with local anesthetic if positive can be followed by a neurolytic procedure, which could potentially provide long-term relief.
The superior hypogastric plexus block is indicated for chronic intractable lower abdominal and/or pelvic pain:
• Gynecologic disorders like endometriosis, pelvic inflammatory disease, and pelvic adhesions
• Nongynecologic disorders like interstitial cystitis, irritable bowel syndrome
• Sympathetically maintained pelvic pain (pelvic CRPS)
• Pain secondary to neoplasm in the pelvic area
The inferior hypogastric plexus block is indicated for chronic intractable lower abdominal and/or pelvic pain:
• Sacral or perineal pain
• Bladder conditions
• Penile pain
• Prostatitis
• Vaginal pain/vulvodynia
• Rectal/anal pain
• Irradiation-induced tenesmus
• Perineal, sacral, and lower pelvic pain caused by malignant causes
• Sympathetically maintained pelvic pain (pelvic CRPS)
• Lower pelvic endometriosis
• Acute herpes zoster
• Postherpetic neuralgia of the sacral area
CONTRAINDICATIONS
• Infection (systemic or localized)
• Coagulopathy
• Distorted or complicated anatomy
• Patient refusal
Other Considerations
The risks and potential contraindications need to be weighed carefully when performed in patients with cancer pain and noncancer pain.
• Although this injection is performed outside the neuroaxis, there are large blood vessels (iliac arteries and vein) in close proximity, and therefore an adequate coagulation status is warranted.
• In the same way, injections into or through an area of infection should be avoided.
• Psychological status in cancer pain patient appears to be less of an issue, as long as the patient or health care surrogate is capable of providing informed consent.
• However, for the nonmalignant pain patient, because of the dramatic psychological overlay often seen in patients who suffer from chronic pelvic pain, including a history of medication abuse and altered self image, it is probably prudent to rule out major psychiatric disorders prior to performing this advanced procedure.
• Immunocompromised patients are potentially at high risk for infection.
• Patients with cancer may have local masses in the region.
• Patients may have thrombocytopenia secondary to chemotherapy.
• Anticoagulation is a concern because of the amount of tissue penetrated and also the vicinity of major blood vessels.
• Aspirin alone is considered safe, but the combination of aspirin with other antiplatelet therapies may increase the risk of bleeding and hematoma.
• Patients must be able to lie prone for the intended length of the procedure which may be difficult with pain and abdominal distension.
RELEVANT ANATOMY
The superior and inferior hypogastric plexuses innervate the lower pelvic viscera including the distal end of the alimental canal, bladder, ureters, prostate, penis, ovaries, uterus, and vagina.
Superior hypogastric plexus
• It is the extension of the celiac, then aortic plexus in a caudad direction, below the aortic bifurcation.
• It receives fibers from the aortic plexus, as well as contributions from L3 and L4 splanchnic nerves.
• It is situated on the ventral aspect of the L5-S1 and on the disc between L5 and S1.
• The superior hypogastric plexus is close to the sympathetic chain at this level, the common and internal iliac arteries and veins on each side.
• The ureter is located just lateral to the structures in close proximity to the anterolateral aspect of the L5 vertebral body.
• As the aorta is shifted more toward the left, the superior hypogastric plexus and hypogastric nerves are located somewhat to the left as well.
• Descending into the pelvis it bifurcates as the right and left hypogastric nerves. These “nerves” aren’t really what is traditionally thought of as a nerve, they are more like meshwork than solid nerve trunks.
• These nerve meshwork diverge lateral to the rectum on both side and curve outward and backward as they make their way down into the pelvis. They interconnect the superior and inferior hypogastric plexuses, contain no ganglia.
Inferior hypogastric plexus
• It is found by following the superior hypogastric plexus and hypogastric nerves in caudad direction as a network of nerves within the connective tissue around the rectum.
• Extensions of inferior hypogastric plexus, which include the medial rectal and vesical plexuses, continue along the branches of the internal iliac artery to innervate autonomic effector of the pelvis (Figure 48-1).
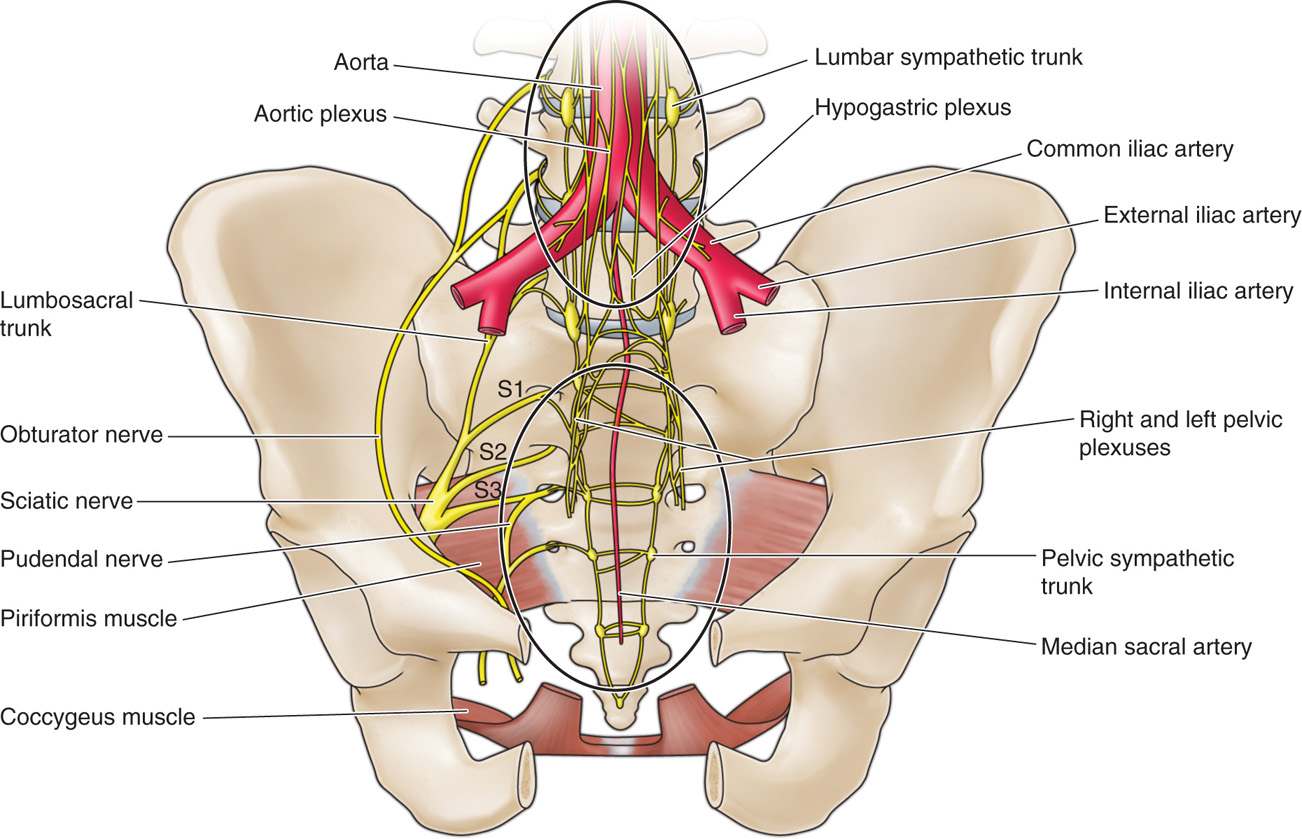
Figure 48-1. Illustration of the superior and inferior hypogastric plexus with relation to nearby anatomical structures on the left. (From Schultz DM. Inferior hypogastric plexus blockade: a transsacral approach. Pain Physician. 2007 Nov;10(6):757-763.)
The key to successfully locating the superior hypogastric plexus lies in identifying the following:
• Iliac crest
• Sacral ala
• L4 and L5 vertebral body and transverse processes
• L5-S1 disc
• Assessing the depth from the skin to the anterior portion of L5
Other relevant anatomy that should be taken into consideration when performing this injection is:
• Iliac arteries and veins
• Ureters at the lateral aspects of L5 vertebral body
• L5 nerve root
The key to successfully locating the inferior hypogastric plexus lies in identifying the following:
• S2 or S3 neural foramina, both posterior and anterior openings
• Anterior surface of the sacrum
Other relevant anatomy that should be taken into consideration when performing this injection is:
• Iliac arteries and veins
• S1-S4 exiting nerve roots
• Rectum is separated from the anterior surface of the sacrum by a layer of extraperitoneal fat and other connective tissues.
PREOPERATIVE CONSIDERATIONS
Preoperative considerations like in all sympathetic blocks, attention should be paid to the potential for sympathetic lysis of vasoconstriction, contributing to hypotension. In addition, review of the CT or MRI performed is mandatory, paying close attention to any abnormal structures present anterior to the sacral promontory or sacral concavity. As there is a significant amount of tissue which the needle must go through, this procedure can be uncomfortable. There is also a significant risk of paresthesia, either at the L5 nerve root for the superior hypogastric block or sacral nerve roots for the inferior hypogastric block.
Preparation of the Patient
• Informed consent and proper explanation of all potential complications.
• Physical examination of the area for infection, skin ulceration or necrosis, and extent of disease.
• Intravenous access for IV fluid and medications for sedation or hypotension caused by sympathectomy or vasovagal reaction.
• Evaluation for contrast allergy—this is of the utmost importance as the utilization of contrast will allow for precise needle placement just anterior to the promontory or the anterior sacral surface.
Documentation for Off-Label Indications
As noted above, this technique was developed for patients with intractable cancer pain, and was often performed with neurolytic agents, with or without a preceding diagnostic block. However, it has recently shown promise as a diagnostic and potentially therapeutic technique for patients with chronic intractable pelvic pain, including interstitial cystitis and chronic pain caused by prostatitis. Although technically potentially difficult to perform, the procedure itself has relatively few risks, and therefore may provide benefit to a larger group of patients. However, as with all procedures for nonmalignant pain, conservative therapies including medication, psychological interventions, and more standard interventions such as epidurals should be tried first.
Superior Hypogastric Plexus Block
Medication
• 1% lidocaine
• 0.25% or 0.5% bupivacaine
• Iohexol 180 (nonionic water-soluble contrast)
Although some authors recommend the use of steroids in sympathetic blocks, there appears to be a little evidence to support this.
Equipment
• 22-gauge 7-in spinal needle
• 25-gauge 2-in needle
• 3-cc syringe for local anesthetic
• 5-cc syringe for contrast
• 10-cc syringe for medications
• Connector tubing (extension)
Technique
Various techniques have been described for needle passage to gain access to the superior hypogastric plexus: lateral approach, transdiscal approach, and anterior approach (Figure 48-2).
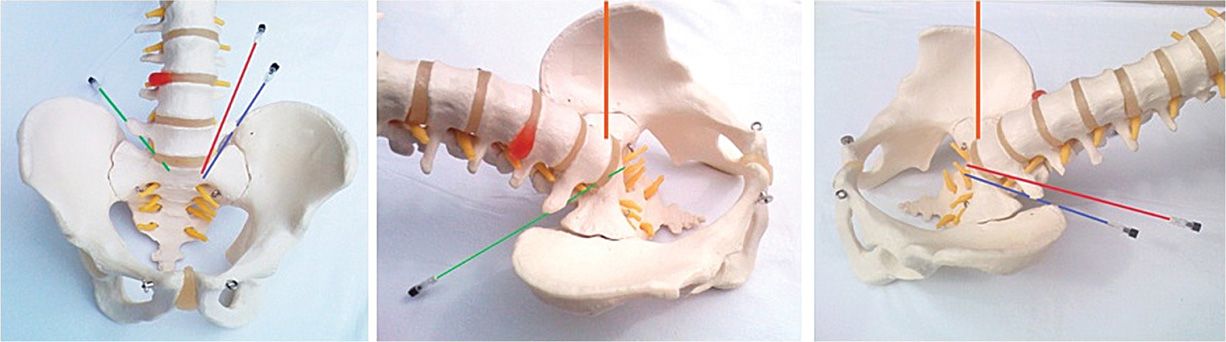
Figure 48-2. Superior hypogastric plexus block. Lateral approach, skin entry at L4 level (red needle), lateral approach, skin entry at L5 level (blue needle), transdiscal approach (green needle), and the anterior approach (orange needle). (Used with permission from Dr. Agnes Stogicza.)
Lateral Approach
Patient Position
Patient is positioned in the prone position with a pillow under the abdomen to decrease the lumbar lordosis.
Fluoroscopic Views
This procedure, unlike most of our other interventional techniques, does not necessarily benefit from an oblique view. The use of three-dimensional imaging helps the clinician to better visualize the eventual needle location.
• Start with anteroposterior image of the lumbosacral area, centered on L5 vertebral body. Note the L5 transverse process, the sacral ala and iliac crest, as the needle has to be advanced anteriorly at the bone-free space. A cephalad tilt of the C-arm is likely to increase the visibly bone-free area.
• Lateral view allows the physician to control the depth of the needle tip as it advances anteriorly past the anterior surface of the L5-S1 disc. This is also the view in which contrast will be injected to verify the position of the tip.
• After the L5 vertebral body endplates optimized, an imaginary line is drawn from the tip of the transverse process of L4 or L5 inferiorly to the midline S1 spinous process. The decision to use a higher (L4) or lower (L5) entry site is dictated by the height of the iliac crests.
• After sterile prep and drape, lidocaine is infiltrated subcutaneously lateral to the transverse process, and the spinal needle is directed anteriorly and inferiorly toward the midline S1 sacral promontory.
• Care must be taken around the L5 nerve root, since the path of the needle may pass close to the root itself, so the patient should be warned about possible paresthesias.
• If the vertebral body is encountered, the needle needs to be withdrawn and repositioned more anteriorly.
• Once the needle is placed, the position is confirmed by injection of a small amount of contrast with firm location anterior to the promontory and to also confirm the lack of vascular uptake (Figures 48-3 and 48-4).
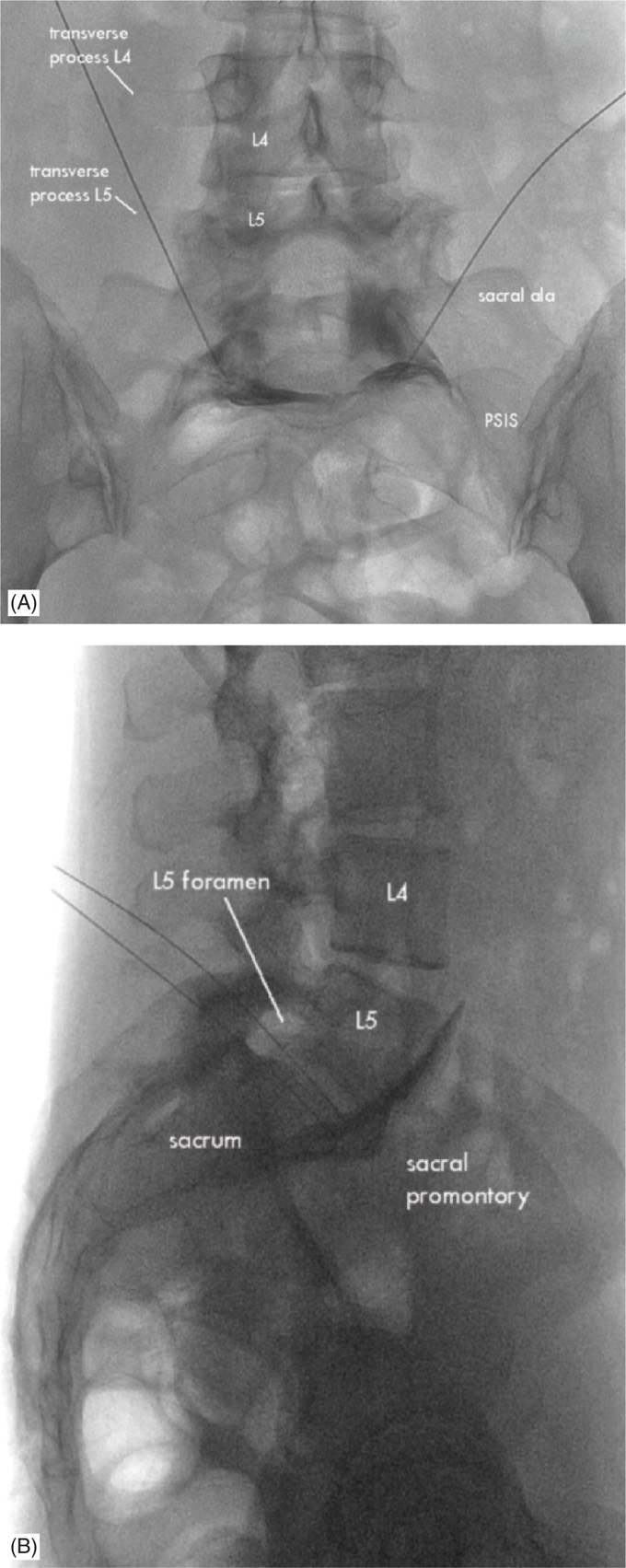
Figure 48-3. Superior hypogastric plexus block. Lateral approach: needles are in the final position. Contrast spreads anterior to L5 vertebral body and the promontorium. Lateral view (A), anteroposterior view (B). Contrast spreads more laterally and then, ideal, bilaterally. (Used with permission from Dr. Agnes Stogicza.)
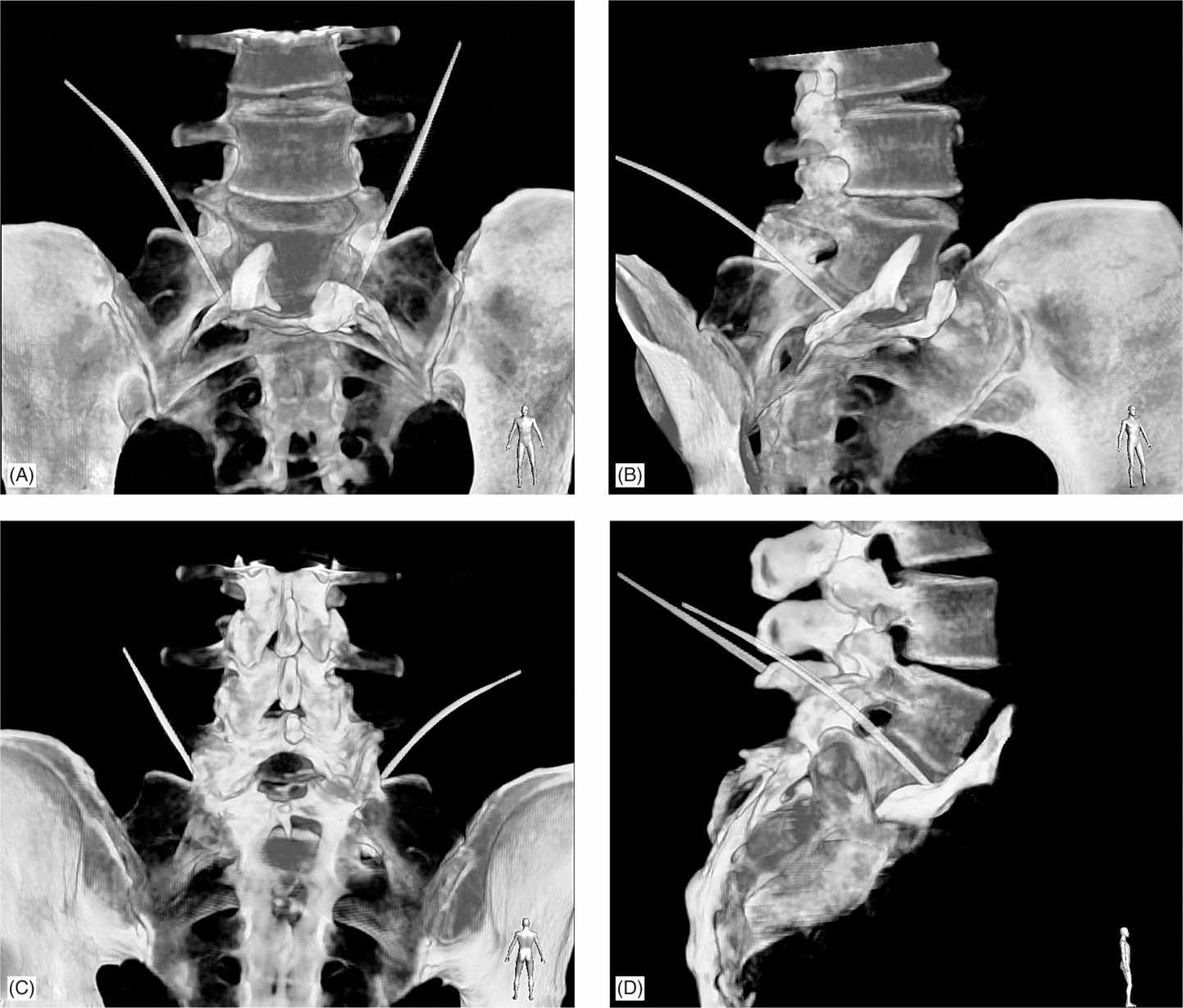
Figure 48-4. Superior hypogastric plexus block, lateral approach, 3D reconstruction. The image was taken with ALLURA Xper FD 20 Phillips. Final needle position and contrast show contrast spread anterolateral to the L5 vertebral body, L5-S1 disc and promontorium. Needles pass between the sacral ala and L5 transverse process. (Used with permission from Dr. Agnes Stogicza.)
• Although the optimum amount of local anesthetic has not been defined, 6 to 8 cc of local anesthetic on each side appears to usually adequately cover the sacral promontory. Using short-acting local anesthetic first, and if the patient notes relief on the table but no complication, following with the bupivacaine is a safe and efficient approach.
• Needle is removed, and the area is covered with a Band-Aid.
Because it is relatively difficult to get contrast truly midline with this approach, the procedure almost always has to be repeated on the contralateral side so that medication will flow bilaterally.
Transdiscal Approach
Patient Position
Patient is positioned in the prone position with a pillow under the abdomen to decrease the lumbar lordosis.
Fluoroscopic Views
• The fluoroscopic image should be centered on the L5 vertebra in anteroposterior view, then the C-arm rotated cephalad until the end plates at L5-S1 are as sharp as possible.
• The C-arm is then obliqued slightly toward the ipsilateral side in order to position the superior articular process into the distal one-third of the disc.
• After sterile prep and drape and local anesthetic infiltration subcutaneously, the needle is introduced in a “down the barrel” view, taking care to direct the needle laterally instead of medially to avoid entering the nucleus pulposus. As the annulus is expected to be difficult to inject and the prevertebral tissue easy to inject, Trescot recommends a loss of resistance technique utilizing saline, lidocaine, or contrast.
• Verify needle position in a lateral view. The tip of the needle should be slightly anterior to either the L5 body, L5-S1 disc, or promontory.
• Contrast should also spread at L5-S1 area, retroperitoneally (Figures 48-5 and 48-6).
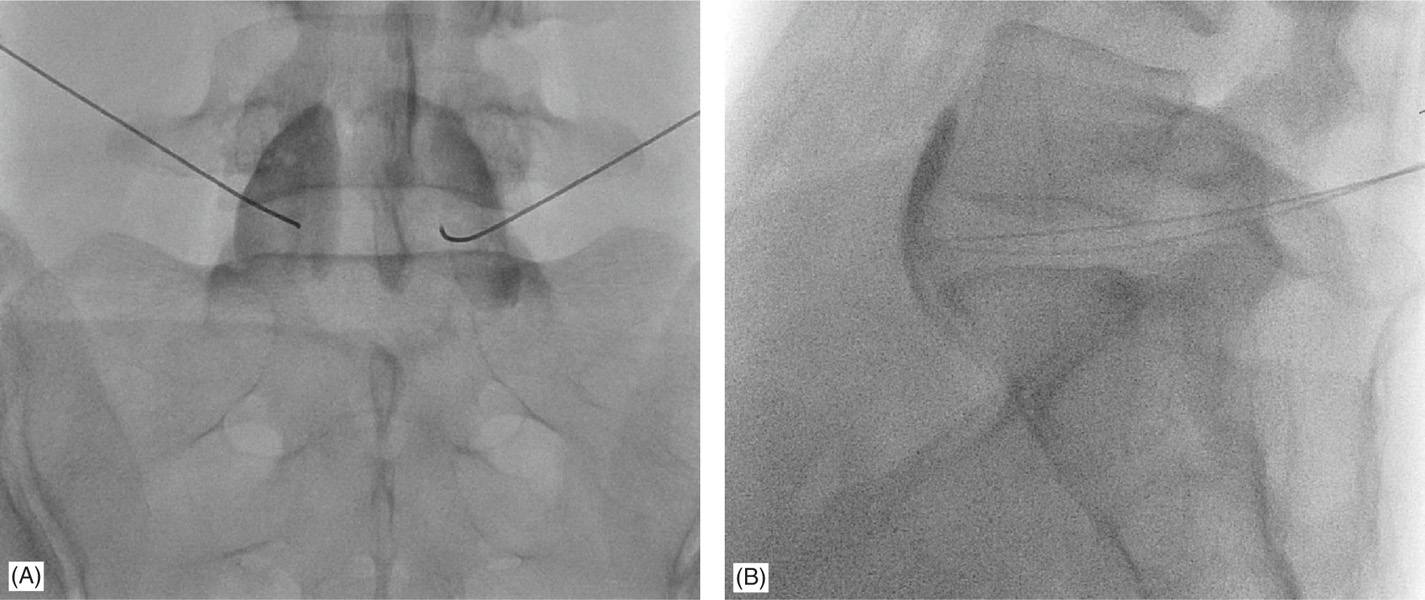
Figure 48-5. Superior hypogastric plexus block, transdiscal approach, needles are in the final position. Contrast spreads anterior to L5 vertebral body and the promontorium. Lateral view (A), anteroposterior view (B). (Used with permission from Dr. Agnes Stogicza.)
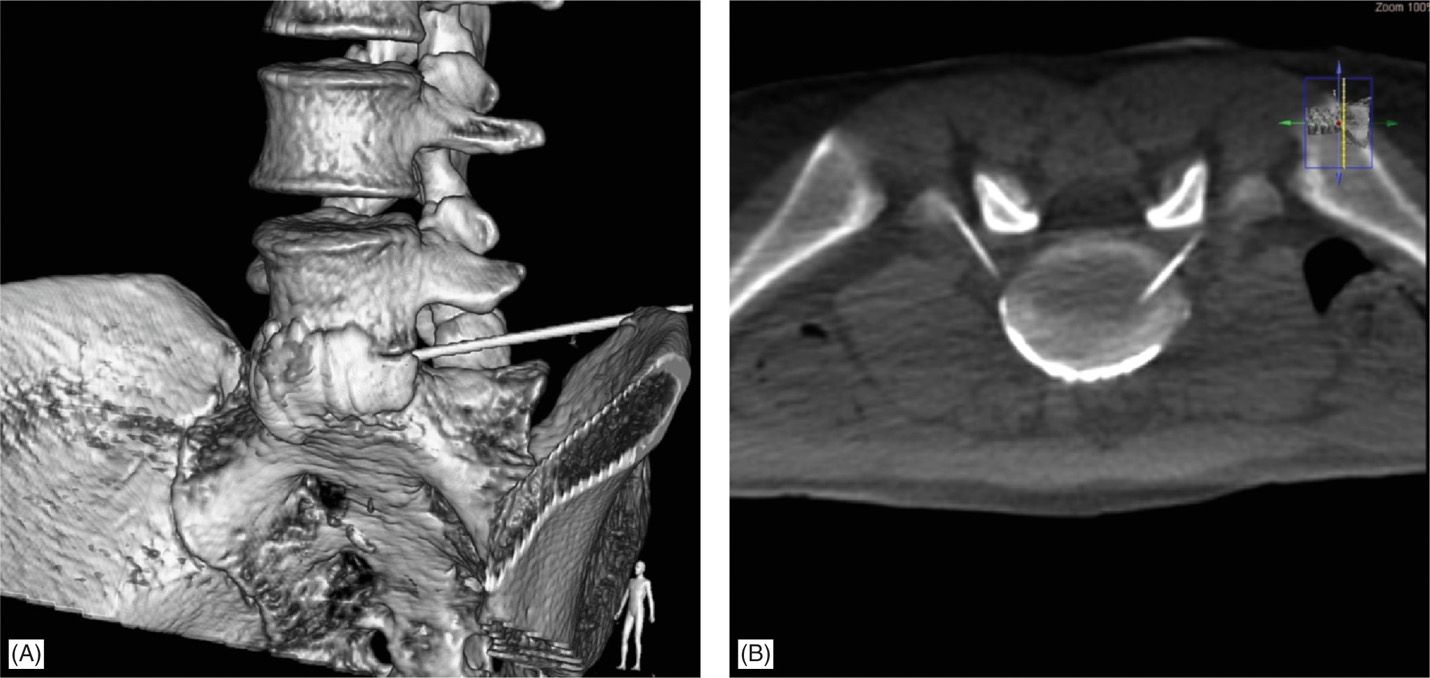
Figure 48-6. Superior hypogastric plexus block, transdiscal approach. 3D reconstruction, oblique view (A) and transsection (B). Final needle position and contrast spread anterior to the L5 vertebral body, L5-S1 disc and promontorium. Needles pass between the sacral ala and L5 transverse process. The image was taken with ALLURA Xper FD 20 Phillips. (Used with permission from Dr. Andrea Trescot.)
• 6 to 8 mL of bupivacaine 0.25 % is injected on each side after negative aspiration.
• Needle is removed, and the area is covered with a Band-Aid.
Since the needle is placed more medially, the local anesthetic often passes bilaterally, obviating the need for a second needle placement (Figure 48-7). This technique has the distinct advantage of being very familiar to those who have performed discograms, and perhaps avoids some of the risk of paresthesia. However, because the needle passes through the disc, there is a theoretical risk of discitis. The patient should probably receive IV antibiotics before the procedure and certainly should be advised of the potential risk of discitis. In my experience, this procedure has been significantly less traumatic for patients who have undergone aforementioned standard techniques.
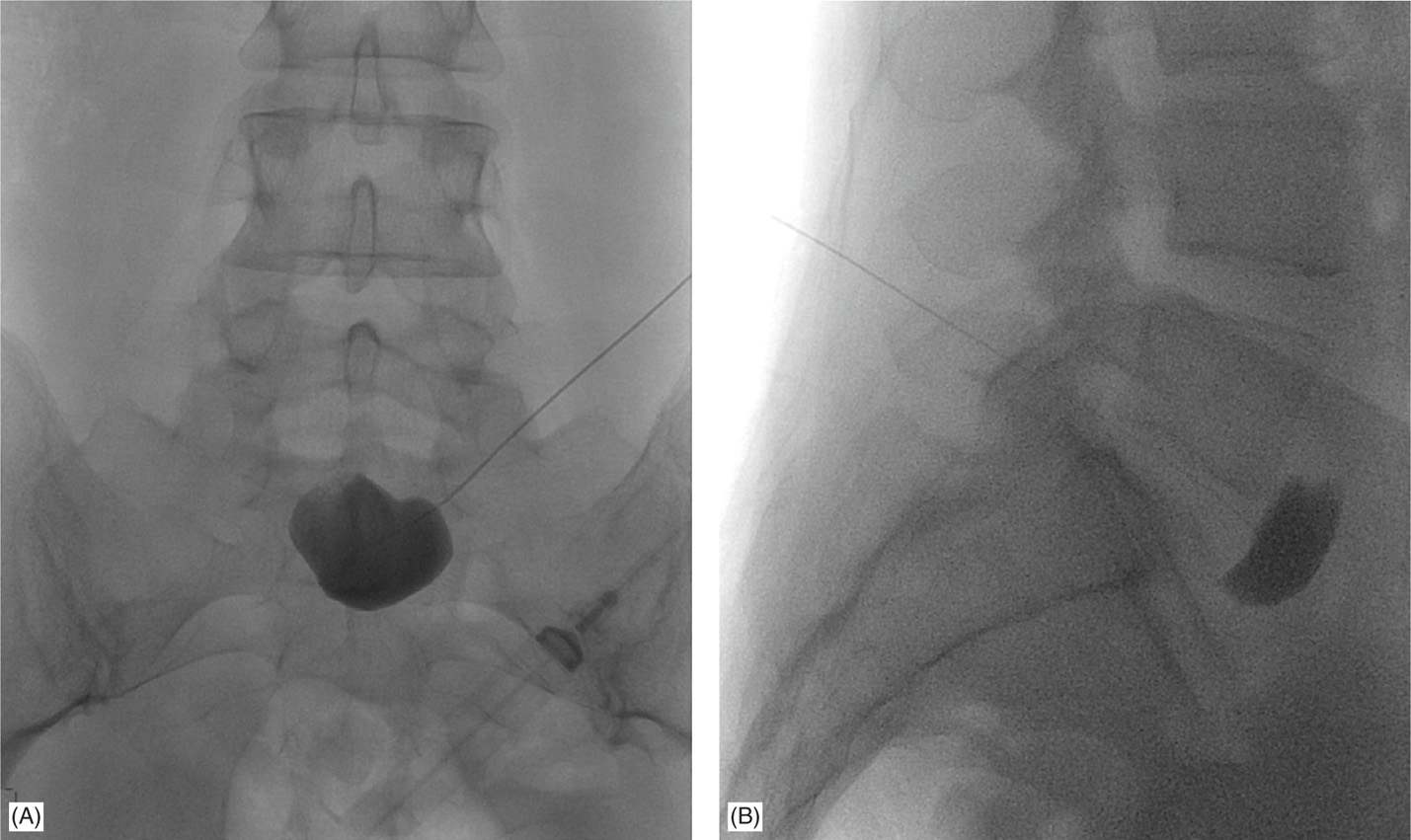
Figure 48-7. Superior hypogastric plexus block, transdiscal approach, single needle technique. Contrast spreads anterior to L5-S1 disc in the midline. Lateral view (A), anteroposterior view (B). (Used with permission from Dr. Agnes Stogicza.)
Anterior Approach
Patient Position
Patient is placed in supine position with pressure points protected.
Fluoroscopic Views
• Using an AP view the L5 vertebral body is identified.
• The tunnel view can be utilized to guide the needle until bony contact on L5.
• Lateral view is used to verify the needle tip placed on either L5 vertebral body or L5-S1 disc.
• After sterile prep and drape lidocaine is infiltrated subcutaneously about 5 cm below the umbilicus.
• A 22-gauge 3.5-in needle is advanced until bony contact.
• Contrast is injected to verify medication spread.
• 10 to 15 cc of 0.25% bupivacaine is injected through the needle.
• Needle is removed, and the area is covered with a Band-Aid.
Even though this approach might be the easiest of all, it is rarely utilized because of the potentially increased risk of infection.
Inferior Hypogastric Plexus Block
Equipment
• 22-gauge 2-in spinal needle
• 25-gauge 2-in needle
• 3-cc syringe for local anesthetic
• 5-cc syringe for contrast
• 10-cc syringe for medications
• Connector tubing (extension)
Medications
• 1% lidocaine
• 0.25% or 0.5% bupivacaine
• Iohexol 180 (nonionic water soluble contrast)
Although some authors recommend the use of steroids in sympathetic blocks, there appears to be a little evidence to support it.
Fluoroscopic Views
• Start with anterior-posterior image of the sacrum and identify the sacral foramina. Choose the foramen that is most easily visible. This block can be performed through S2, S3. Cephalo-caudad and ipsilateral rotation is likely to optimize foraminal view.
• Lateral view allows the physician to control the depth of the needle tip as it advances anteriorly past the anterior surface of the sacrum.
This is also the view in which contrast will be injected to verify the position of the tip
Technique
The inferior hypogastric plexus block was first described by Schultz in the journal Pain Physician. Utilizing the ability to fluoroscopically line up the foramen between the posterior and anterior sides, Schultz recommends finding the most visible foramen (usually S2 or S3, and slightly obliquing the C-arm ipsilaterally to optimize superimposing the posterior and anterior foramen).
• After sterile prep, drape, and local anesthetic infiltration of the subcutaneous tissues, a 25-gauge 5-in needle is utilized.
• The needle is passed through the posterior tissues onto the lateral edge of the posterior foramen and then walked anteriorly.
• Switching to a lateral view, the needle is advanced just anterior to the anterior sacral plate.
• Contrast shows a thin layer, hugging the anterior border of the sacrum area (Figure 48-8).
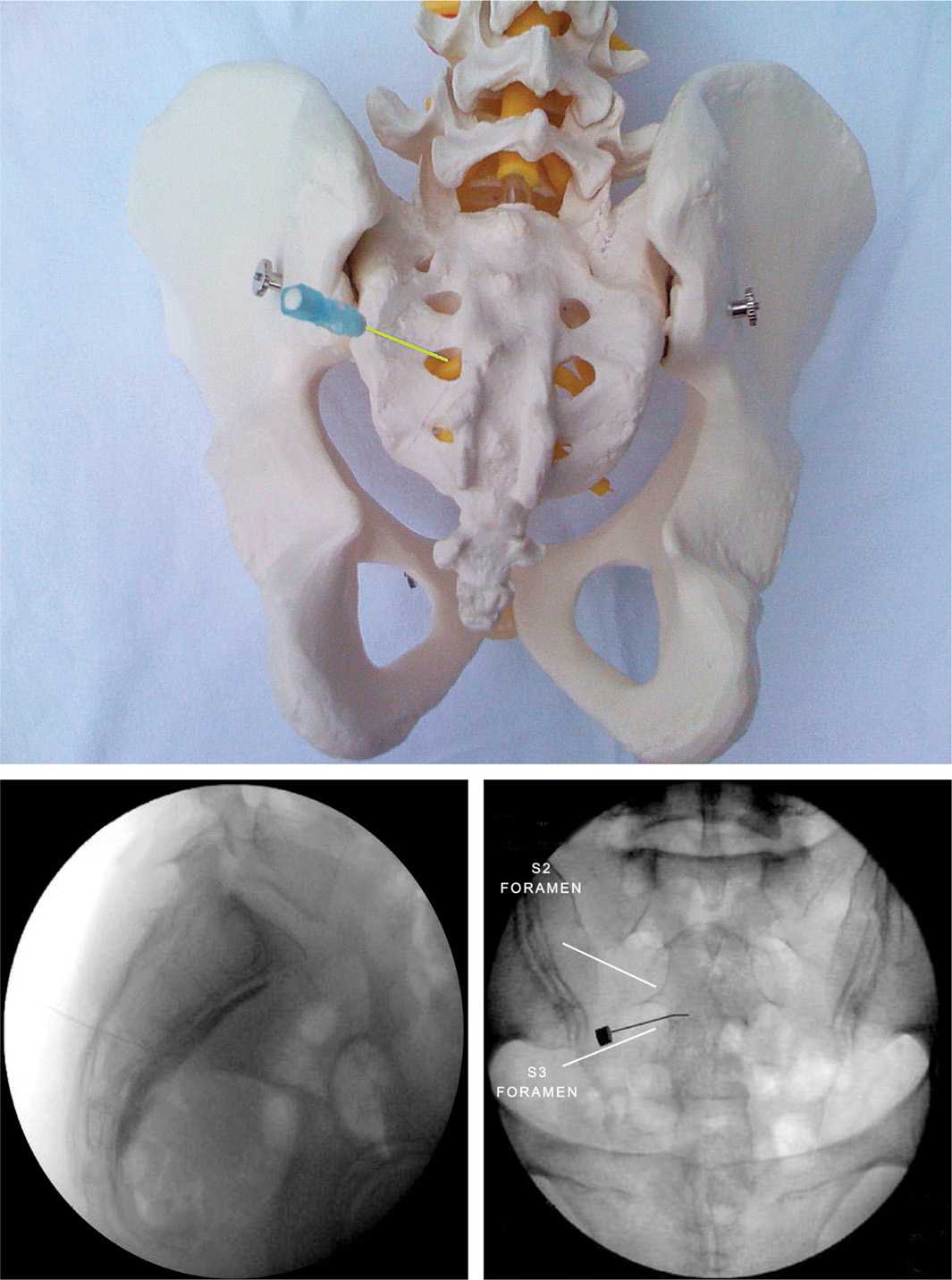
Figure 48-8. Inferior hypogastric plexus block. Schematic picture (upper): needle is in the S3 foramen. Lateral view (left): needle is in final position; contrast spreads at the anterior surface of the sacrum. Anteroposterior view (right): needle is passing through the S3 foramen, toward medial to the anterior surface of the sacrum. (Used with permission from Dr. Agnes Stogicza.)
• Then 5-cc of local anesthetic, first lidocaine, followed by bupivacaine 5 cc, is injected to anesthetize the inferior sacral plexus.
• Needle is removed, and the area is covered with a Band-Aid.
POSTPROCEDURE CONSIDERATIONS
Because these are sympathetic blocks, there is a potential for vascular dilation leading to hypotension. There is also at least a theoretical risk of increasing gastrointestinal motility in the lower abdominal region, leading to the potential for diarrhea. The patient should be counseled to monitor pain relief, ideally with a pain diary to confirm the diagnostic aspects and also the therapeutic effects. Patient education about the signs and symptoms of infection or bleeding is necessary.
Monitoring Potential Complications
During the procedure, blood pressure, heart rate, and Sao2 are monitored for potential epidural or intravascular injection, allergy, or bleeding caused by complications.
Postprocedure complications include bleeding (which would be expected immediately after the procedure), acute and late infections, and, for the inferior hypogastric, local anesthetic bathing of the lower extremity nerves, leading to weakness and difficulty walking. There is at least a theoretical risk of loss of sensation of the bladder and bowel that would normally trigger the urge to urinate or defecate, and therefore the patient should be counseled to attempt to urinate and defecate on a regular schedule.
CLINICAL PEARLS AND PITFALLS
• Performing a superior hypogastric block from a lateral approach, starting first at the L4 transverse process especially in males with high riding iliac crests, will provide the most straightforward injection with a low risk of L5 paresthesia. The temptation to start low should be avoided (Figure 48-9).
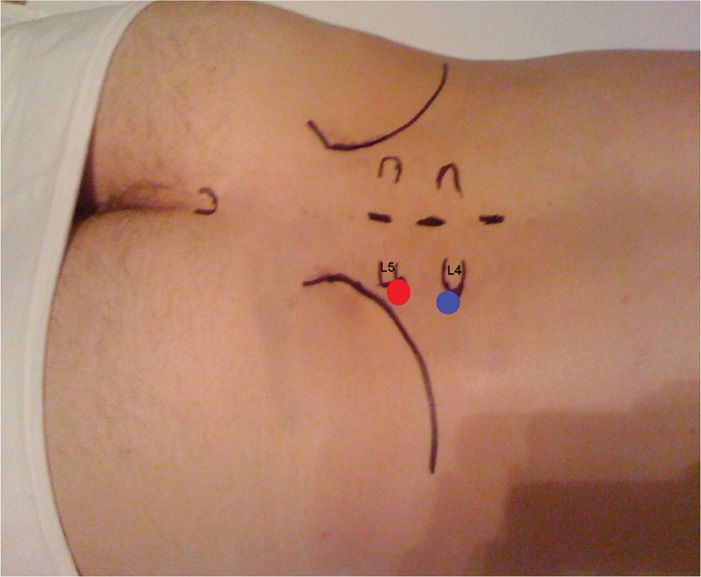
Figure 48-9. Skin entry points for superior hypogastric block, lateral approach. The red dot corresponds to the L5 and the blue dot corresponds to the L4 transverse process. In this male patient, with high riding iliac crest the recommended entry level is L4. (Reproduced with permission from Schultz DM. Inferior hypogastric plexus blockade: a transsacral approach. Pain Physician 2007: 10:757-63.)
• The transdiscal approach, though associated with the potential for discitis, may well prove to be the easiest on the patient and therefore the easiest on the operator, because it is a familiar view. It has proven to be the easiest approach to teach; after one attempt on a cadaver, almost all participants are able to place the needles appropriately.
• The injections can be diagnostic as well as therapeutic. The patients with positive diagnostic injections are generally candidates for neurolysis by phenol or alcohol.
• The superior hypogastric block does not necessarily cover the areas innervated by the inferior hypogastric plexus.
• Most studies report no or only transient complications, and complications mostly arise from the wrong needle placement and injection:
![]() Transient paresthesia is the most common complication.
Transient paresthesia is the most common complication.
![]() Rectal puncture is easily avoided with using lateral views with the fluoroscope.
Rectal puncture is easily avoided with using lateral views with the fluoroscope.
![]() The most vulnerable structures are at the iliac artery and vein, so although it increases costs, using a blunt needle for the superior hypogastric plexus block is reasonable and might minimize risks and complications.
The most vulnerable structures are at the iliac artery and vein, so although it increases costs, using a blunt needle for the superior hypogastric plexus block is reasonable and might minimize risks and complications.

Full access? Get Clinical Tree






