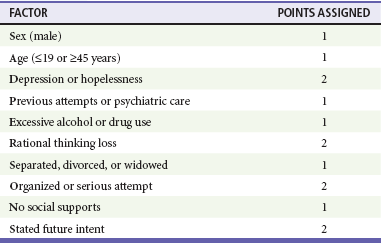
Chapter 115 Although suicide has occurred in all societies since the beginning of recorded history, attitudes toward suicide have differed dramatically among various eras and cultures. Seneca viewed suicide as the ultimate expression of personal freedom, but later Judeo-Christian religions have routinely condemned it. Shakespeare portrayed suicide sympathetically and expressed either pity or admiration for the victim.1 In the United States, suicide is illegal in 49 states, and only since 1994 has assisted suicide of terminally ill patients been sanctioned in Oregon. On the Internet, suicide help groups provide active advice on methods, and numerous bulletin boards condemn them. More than 100,000 sites about suicide now appear on the Internet.2 Suicidal patients represent almost 2% of emergency department (ED) visits.3 Two facts are especially important to remember in approaching potentially suicidal patients. First, many suicide attempts occur during an acute crisis, such as a personal loss or the exacerbation of an underlying psychiatric disorder. This acute crisis is usually time limited and may be resolvable or treatable. Second, except for the acutely psychotic patient, suicidal patients are usually ambivalent about dying. The attitude and approach of the emergency physician can help a patient choose crisis resolution rather than death. The term suicide, from the Latin suicidum (“to kill the self”), refers to a continuum of thought and action that runs from ideation to completion of the act.4 Parasuicide is used by the British to describe an attempted suicide that is more of a gesture than a serious act. Statistically, there are 10 to 40 suicide attempts for every completed act.5 Chronic suicidal behavior consists of recurrent self-destructive acts, such as heavy drinking in the presence of alcoholic liver disease. Occult suicide refers to self-destructive acts disguised as accidents, such as the intoxicated, depressed driver in an apparently accidental car crash. Silent suicide describes the act of slowly killing oneself by nonviolent means, such as starvation or noncompliance with essential medical treatment. Silent suicide is most common in elders and frequently goes unrecognized. A suicide pact is an agreement between two people who are intimately involved and accounts for 0.6% of all suicides.6 Mass suicide or group suicide involves a number of willing and sometimes not-so-willing persons, such as members of an apocalyptic cult. Suicidal ideation is common, and as many as one in three people consider suicide during their lifetime.7 In 2006, suicide was the eleventh leading cause of death among persons older than 9 years, accounting for 33,289 deaths.8 This is the equivalent of 89 suicides per day or one suicide every 15 minutes. It is the fourth leading cause of death for adults between the ages of 18 and 65 years. In the United States, there are more than 800,000 suicide attempts per year, many of which do not present to EDs.9 In one study performed during a 5-year period, there were approximately 412,000 annual ED visits for attempted suicide and self-inflicted injury. The most common method of injury was poisoning (68%), followed by cutting or piercing (20%). One third were admitted to the hospital, with 31% going to the intensive care unit. A psychiatric diagnosis was assigned for 55% of visits, with depressive disorder accounting for 34% and alcohol abuse for 16%.10 The rate of self-harm visits to the ED appears to be increasing. From 1999 to 2004, intentional self-harm episodes increased by 20% with a correspondingly greater increase in hospitalizations for the same.11 Unemployment and financial troubles may play a role in this rise, and a recent study links suicidal behavior to economic conditions. Longitudinal data show that overall suicide rates rise during recessions and fall during expansions, particularly for patients aged 25 to 64 years.12 In addition to the recent economic troubles, there are other factors that may play a role in the increasing number of suicide attempters seen in the ED. These include a rise in homelessness and the collapse of the mental health hospital system in most states.13 Suicide rates vary with age, gender, race, and marital status. Suicides are highest among older individuals, particularly elderly white men. The case fatality rate also increases tremendously with advancing age, from 5% in youths aged 5 to 14 years to 34% in adults older than 64 years.14 White men commit 73% of all suicides in the United States. Whites and Native Americans are much more likely to commit suicide than are African Americans, Hispanics, or Asians. Marriage decreases the likelihood of suicide, but the rate of suicide is higher for separated or divorced people than for those who never had a close relationship. Women attempt suicide three to four times more often than men do, whereas men are three to four times more likely to succeed. In one U.S. study, only 5% of suicide attempts by women were fatal compared with 23% of those by men.14 In general, men tend to use more lethal methods, such as firearms. Worldwide, Chinese and Indian women have rates of suicide higher than those of women of other nationalities.15 Pregnant women are at a significantly lower risk than are women of childbearing age who are not pregnant. Motherhood seems to protect against suicide, except that postpartum depression is associated with a higher than normal suicide rate. Most people who attempt suicide have one or more known risk factors (Box 115-1). Individuals with the highest risk include those with psychiatric disorders, alcohol or substance abusers, adolescents, elders, and patients with certain chronic illnesses. In patients hospitalized for psychiatric disorders, the first month after discharge carries a high risk of suicide,16 and that risk is especially great for patients who are in the first week after discharge from a psychiatric facility.17 Any prior history of suicide, even in the remote past, is an important risk factor.18 A strong association may exist between suicide risk and bisexuality or homosexuality in men.19 This association is also seen in lesbian, gay, and bisexual adolescents.20 Unemployment appears to be a risk factor for suicide among 18- to 24-year-old men.21 Homeless people with mental illness are at particularly high risk for suicidal behavior, in part because of the high prevalence of traditional risk factors. Recent incarceration is also a risk factor for suicide. During the first 2 weeks after release, the risk of death among former inmates is more than 12 times that of the general population. The leading causes of death among former inmates include drug overdose, cardiovascular disease, homicide, and suicide.22 In general, the risk of suicide in recently released prisoners approaches that in recently discharged psychiatric patients.23 Suicide completers and suicide attempters represent separate but overlapping populations.24 Although 10 to 15% of suicide attempters ultimately complete suicide, 60 to 70% of suicide completers have no prior history of attempts and commit suicide on the first known attempt.25 In individuals who committed suicide while not in contact with mental health services, nearly one third of cases had no concurrent mental disorder.26 Societal, Psychiatric, and Biologic Factors Psychoanalysts explain suicide in terms of psychic forces. Freud believed that suicide stems from aggression initially directed toward another person but that ultimately turns against the self. Depression and suicide in the Freudian model represent internalized anger. Many authorities have recognized this association between aggression and suicide. In the United States, more than 1000 deaths each year result from murder-suicides. The perpetrators are usually depressed mothers, despairing elderly men, or young men with intense sexual jealousy. Their victims are usually young children, blood relatives, or female sexual partners. The dual risk for suicide and violence is greatest in alcoholics.27 Current research suggests a biologic basis for depression and suicide involving the serotonergic and dopaminergic systems. People who attempt suicide have altered serotonin receptor function and low serotonin levels.28,29 These abnormalities may be regulated through serotonergic-related genes in persons with major depression.30 The genetic basis of suicide is not clearly understood. The STin2 genetic locus might, at least in part, account for the observed familial aggregation of suicidal behavior.31 Polymorphisms in the tryptophan hydroxylase gene may affect the synthesis of serotonin. Recent data also indicate that certain genetic markers may be linked to suicidal ideation associated with medications used to treat depression.32 The genetic susceptibility to suicide, however, may affect individuals only when it is associated with psychiatric illness or stress.33 The rate of suicide is twice as high in families of suicide victims, and a family history of suicide predicts suicide independent of severe mental disorder.34 Relatives of suicide completers are more than 10 times more likely than relatives of comparison subjects to attempt or to complete suicide.35 Depressed patients who attempt suicide excrete less homovanillic acid in their urine and produce less dopamine than depressed patients who have not attempted suicide. Low concentrations of dopamine and serotonin metabolites in the cerebrospinal fluid also correlate with suicidal behavior. Suicide attempts in women vary with estrogen levels, with 42% of attempts occurring during the first week of the menstrual cycle.36 Neuroanatomy may also influence suicidality; suicide victims have smaller right-sided parahippocampi than control subjects.37 Although there are no currently available laboratory tests that can identify individuals at increased risk for suicide, research holds promise for biologic markers in the future. Some drugs, including reserpine, benzodiazepines, and barbiturates, are associated with depression and suicidal behavior. The Food and Drug Administration recently linked suicidal ideation among children and adolescents to selective serotonin reuptake inhibitors (SSRIs) and added a black box warning for SSRI use in all age groups.38 It is ironic that in both the United States and the Netherlands, SSRI prescriptions for children and adolescents decreased after these regulatory warnings and these decreases were associated with increases in suicide rates in both children and adolescents.39 Patients who commit suicide shortly after the initiation of antidepressant medications are explained by the “mobilization of energy” theory.40,41 According to this theory, patients who are profoundly depressed may have the energy to attempt suicide only as their condition improves with treatment. Such patients should be monitored very closely during their initial phase of treatment. Most completed suicides involve firearms (70%), whereas most attempted suicides involve the ingestion of drugs or poisons (72%).42 In one large study, poisoning with drugs accounted for 74% of acts but only 14% of fatalities; firearms and hanging accounted for only 10% of acts but 67% of fatalities. Firearms were the most lethal means (91% resulted in death), followed by drowning (84%) and hanging (82%).14 Episodes involving firearms are 2.6 times more lethal than the second most lethal suicide method, suffocation.43 In 2005, 17,002 suicides involved firearms in the United States.44 Guns represent the most common method of suicide in all victim subgroups, especially among older persons and adolescents, and the use of guns has increased dramatically in the past decade, recently replacing ingestion as the major cause of suicide among women.45 The simple presence of a gun in the home represents an independent risk factor for firearm-related suicide but not by non-firearm means.46 This is particularly true for adolescents, whose risk for suicide increases 5 to 10 times when there is a gun in the household.47,48 In general, firearm prevalence is positively related to the suicide rate, even after control for rates of attempted suicide.49 Suicide by handgun is often associated with drug or alcohol use.50 The rate of gun-related suicide is 57 times higher in the first week after purchasing of a handgun.51 After gun-related deaths, other lethal methods chosen by men include hanging, suffocation, and jumping from a height, whereas women are more likely to commit suicide by poisoning. Antidepressant overdose is the most common cause of suicide by ingestion.52 Cyclic antidepressants are associated with more deaths because of their widespread use and high potential for lethality. Most patients hospitalized for self-poisoning have ingested drugs prescribed by their physicians for depression.53 SSRIs, including fluoxetine (Prozac), sertraline (Zoloft), and paroxetine (Paxil), are less lethal when they are taken in overdose and have replaced cyclic antidepressants as the first therapy in depression. The method of suicide depends on many factors, including psychic issues of self-hate, the desire for a peaceful versus violent death, and the availability of fatal means. Those who jump to their death are more likely to be single, unemployed, or psychotic. Those who use firearms are more likely to be male, to be alcoholic, to have been arrested, or to have an antisocial or borderline personality disorder.54 Communities with tall buildings and bridges have higher rates of suicide from falls, whereas suicide by gunfire occurs more often in areas where firearms are prevalent. “Suicide by cop” occurs when a suicidal individual intentionally provokes a police officer by orchestrating a lethal situation in which the officer is forced to shoot in self-defense or to protect other civilians. This may account for as many as 11% of officer-involved shootings in Los Angeles.55 Certain individuals carry a suicide note; some offer an eerie postmortem apology to the police officer who ultimately kills them. Although most psychiatric patients never attempt suicide, most people who commit suicide have either a diagnosable psychiatric illness or alcoholism. Exceptions include those with mental retardation, dementia, and agoraphobia.56 Patients with an affective disorder, especially major depression, are at highest risk.57,58 Approximately 15 to 20% of people with major depression commit suicide, usually while under psychiatric care.59 Individuals who experience hopelessness, anhedonia (loss of ability to experience pleasure), and mood cycling are at highest risk. Impulsive-aggressive personality disorders and alcohol abuse are independent predictors of suicide in major depression.60 Approximately 10% of schizophrenic patients will kill themselves. Psychotic patients who commit suicide are most often unmarried white individuals with high intelligence quotient scores.61 Patients with borderline personality disorders are also predisposed to commit suicide. Women with borderline personality disorder who attempt suicide often have a history of childhood sexual abuse and impulsive behavior. The risk is especially high when patients require hospitalization for psychiatric illness and is greatest the first month after discharge.62,63 Approximately 40% of patients with panic disorder attempt suicide at some point in their lives. These patients usually have an additional comorbid psychiatric diagnosis (e.g., borderline personality disorder, substance abuse, emotional instability). However, any preexisting anxiety disorder (including social phobia, simple phobia, generalized anxiety disorder, panic disorder, agoraphobia, obsessive-compulsive disorder) is an independent risk factor for subsequent suicidal ideation and attempts.64 Post-traumatic stress disorder, sustained by military combat personnel and disaster survivors, is also associated with suicide. Post-traumatic stress disorder frequently coexists with a major depressive episode, and this combined psychopathology enhances the risk for suicidal behavior.65 In 2005, there were at least 6256 suicides among those who served in the U.S. armed forces, a rate double that of nonveterans. Veterans between the ages of 20 and 24 years who served in Iraq or Afghanistan had the highest suicide rate among all veterans.66 Of successful suicides reported by the National Violent Death Reporting System, 33.3% tested positive for alcohol, 16.4% for opiates, 9.4% for cocaine, 7.7% for marijuana, and 3.9% for amphetamines.67 Other studies show that approximately 25% of all suicides involve alcoholics, and estimates of the lifetime risk of suicide from chronic alcoholism range from 3 to 25%.68 Alcoholics who commit suicide usually have multiple risk factors, including major depressive episodes, unemployment, medical illness, and interpersonal loss. In psychiatric patients, the use of alcohol increases depression and suicidal behavior. Nearly half of all adolescents who attempt suicide use drugs shortly before the attempt, and alcohol intoxication is strongly associated with suicide by firearms.69 Cocaine use is particularly dangerous. In New York City, 20% of all suicide victims younger than 61 years used cocaine within days of their death. Among young Hispanic men, nearly half of the suicide victims have toxicologic screens positive for cocaine.70 In general, cocaine abusers choose violent means of self-destruction, especially firearms. Suicide among adolescents has quadrupled during the past 40 years and is now the third leading cause of death (after accidents and homicides) in people between 5 and 24 years of age.71 Approximately 2 million U.S. adolescents attempt suicide each year, and 19% report serious consideration of suicide in the past year.72 Although some authorities believe that the rise in adolescent suicide simply corresponds to changing demographics in the United States, others believe that the increase is related to a growing sense of hopelessness, increased economic pressures, and access to firearms. In a survey of high-school students in North Carolina, 24% had seriously considered suicide, 19% had planned suicide, and 9% had actually attempted suicide during a 1-year period.73 Adolescent girls are more likely to attempt suicide, whereas adolescent boys are more likely to complete suicide; the ratio of attempted to completed suicides is 25 : 1 for adolescent girls and 3 : 1 for boys.74 Most adolescents who complete suicide have made previous suicide threats. The majority of youths who kill themselves meet criteria for diagnosable psychiatric disorders, and both alcohol and substance abuse play a significant role in teenage suicide attempts. Adolescents with panic attacks are twice as likely as adolescents without panic attacks to make suicide attempts.75 Gay, lesbian, bisexual, or “not sure” youths may also be more prone to self-harm.76 Belonging to the “Goth” subculture is a predictor of self-harm and attempted suicide.77 Nearly 40% of youths in runaway programs report prior suicide attempts.78 Young people may also be influenced by movies or television shows that feature suicide. Teenage suicides typically increase after television broadcasts on the subject. From 1989 to 1995, suicide by firearm in young people increased dramatically.79 The firearm-related suicide rate in U.S. adolescents is 11 times higher than the combined rates of 25 other industrialized countries.80 Having a gun in the home places the troubled adolescent in great danger, and storing the gun in a locked cabinet or separating it from the ammunition does not deter suicide attempts.81 Surprisingly, up to 23% of adolescents who have attempted suicide report that their families continue to keep firearms and ammunition in the home despite their suicide attempt. The highest rates of completed suicide occur in elders. Suicide by firearm is the fourth leading cause of injury-related deaths among older U.S. residents.82 Older Americans use highly lethal methods when attempting suicide and, unlike adolescents, rarely stage an attempt that permits rescue. Self-inflicted gunshot wounds account for 88% of elder suicides. White men older than 65 years account for approximately 80% of suicide deaths, whereas suicide is rare among elderly people belonging to minority groups.83 Suicide among older adults is especially common in those with prior suicide attempts or major depression. Severity of depression is the strongest predictor of suicide in elders.84 Physicians often overlook signs of depression in older patients, even though most who commit suicide see their primary care physician during the month before their death. In one study, almost half of all elders who committed suicide visited a physician in the preceding week.85 Elders also have more chronic illnesses that predispose to suicide. Perceived poor health, poor sleep quality, and limited presence of a relative or friend to confide in are also associated with suicide among elders.86 Patients with terminal illnesses may commit suicide to end their suffering and to reduce the emotional and financial burden on their families. Diseases more highly associated with suicide include cancer, stroke, renal failure, congestive heart failure, and chronic lung disease. In elders, cancer, congestive heart failure, chronic obstructive lung disease, seizure disorder, urinary incontinence, anxiety disorders, depression, bipolar disorder, and moderate to severe pain are specific illnesses associated with suicide.83 The acquired immunodeficiency syndrome (AIDS) epidemic has also increased suicide rates, and the relative risk of suicide in men with AIDS is nearly 37 times higher than that in uninfected men. Patients who are positive for human immunodeficiency virus but do not have AIDS-defining conditions are more likely to be suicidal than those with active disease.87 After a suicide attempt, patients with a normal mental status should be asked about the details of the act after medical evaluation and treatment are initiated. Suicidal patients may give inaccurate histories or may refuse to speak to the physician. Because most people who attempt suicide communicate their intent to others at some point, family, friends, police, and paramedics should be interviewed about the patient’s recent actions and possible motivations. They may also provide information about the specifics of the current suicide attempt. Although some physicians worry that current federal laws regarding patient privacy conflict with the need to obtain information with the family, there is an emergency exception in the Health Insurance Portability and Privacy Act. Section 164.512(j), “Uses and Disclosures to Avert a Serious Threat to Health or Safety,” allows physicians to disclose protected health information without individual authorization “based on a reasonable belief that use or disclosure of the protected health information was necessary to prevent or lessen a serious and imminent threat to health or safety of an individual or of the public.”88 Once the patient is medically stable, the presence of risk factors for suicide should be determined. Such factors may include a history of previous suicide attempts or psychiatric care; a history of excessive alcohol or drug use, both acute and long term; family history of suicide; and signs of depression, including a sense of hopelessness. A history of a “near-lethal” prior attempt is particularly worrisome.89 Patients who have a history of deliberate self-harm (self-poisoning, cutting, burning, or hitting oneself) have a higher risk of suicide, especially male patients.90 More than 5% of people seen at a hospital after self-harm successfully commit suicide within 9 years.91 The patient’s marital status and social support are important factors, and the motivation for and the seriousness of the suicide attempt are assessed. Some physicians ask patients to provide their own lists of “reasons why they want to live”—a sort of reverse score for suicidality. If discharge is being considered, patients should be asked whether they would harm themselves if they were released from the ED. Additional demographic information may be helpful (see Box 115-1). The SAD PERSONS mnemonic can be used to document salient points and to facilitate subsequent communications with primary care providers and psychiatrists (Table 115-1). Table 115-1 From Hockberger RS, Rothstein RJ: Assessment of suicide potential by nonpsychiatrists using the SAD PERSONS score. J Emerg Med 6:99, 1988.
Suicide
Perspective
Definitions
Epidemiology
Pathophysiology and Etiology
Methods of Attempting Suicide
Clinical Features
Alcoholism and Substance Abuse
Adolescents
Older Adults
Chronic Illness
History
Patients Who Present after a Suicide Attempt or Have Suicidal Ideation

Full access? Get Clinical Tree


Suicide
Only gold members can continue reading. Log In or Register to continue




