CHAPTER 42
Stellate Ganglion Block
Stellate ganglion blockade has been utilized since the 1920s to treat a variety of medical conditions. Although blind stellate ganglion blockade had been the norm for decades, the use of fluoroscopy has allowed increased accuracy with the use of less medication and decreased complications.
INDICATIONS
The indications for stellate ganglion blockade include:
• Differentiation of sympathetically maintained (SMP) versus sympathetically independent (SIP) pain syndromes of the head or upper extremity
• Upper extremity/facial complex regional pain syndrome: type I (reflex sympathetic dystrophy [RSD]), type II (causalgia)
• To increase upper extremity perfusion
![]() Raynaud disease
Raynaud disease
![]() Upper extremity arterial embolism
Upper extremity arterial embolism
![]() Intra-arterial drug injection
Intra-arterial drug injection
• Phantom limb pain
• Cluster or atypical vascular headache
• Glaucoma
• Optic nerve neuritis
• Head and face sympathetically mediated cancer pain
• Head/neck/thoracic acute herpes zoster or postherpetic neuralgia
• Hyperhidrosis of the head/neck/axilla/thorax
• Refractory atypical chest pain
• Pulmonary embolism
• Intractable angina pectoris
• Ventricular arrhythmia secondary to sympathetic imbalance
• Post mastectomy pain
• Meniere syndrome
• Scleroderma
CONTRAINDICATIONS
• Systemic or local infection in the area of injection
• Primary or secondary coagulopathy
• Untreated allergy to any of the procedure medications
• Previous anterior lower cervical surgery
• Patient refusal
RELEVANT ANATOMY
The stellate ganglion is usually formed by the fusion of the inferior cervical and first thoracic sympathetic ganglia (Figure 42-1). The stellate ganglion lies just anterolateral to the seventh cervical vertebral body at the base of the C7 transverse process, lateral to the first thoracic vertebral body and over the neck of the first rib, in the groove between the vertebral body and the transverse process. It lies anterior or immediately lateral to the longus colli muscle (Figure 42-2) and is posterior to the vertebral and carotid arteries. The ganglion also lies just anterior to the C8 and T1 spinal roots.
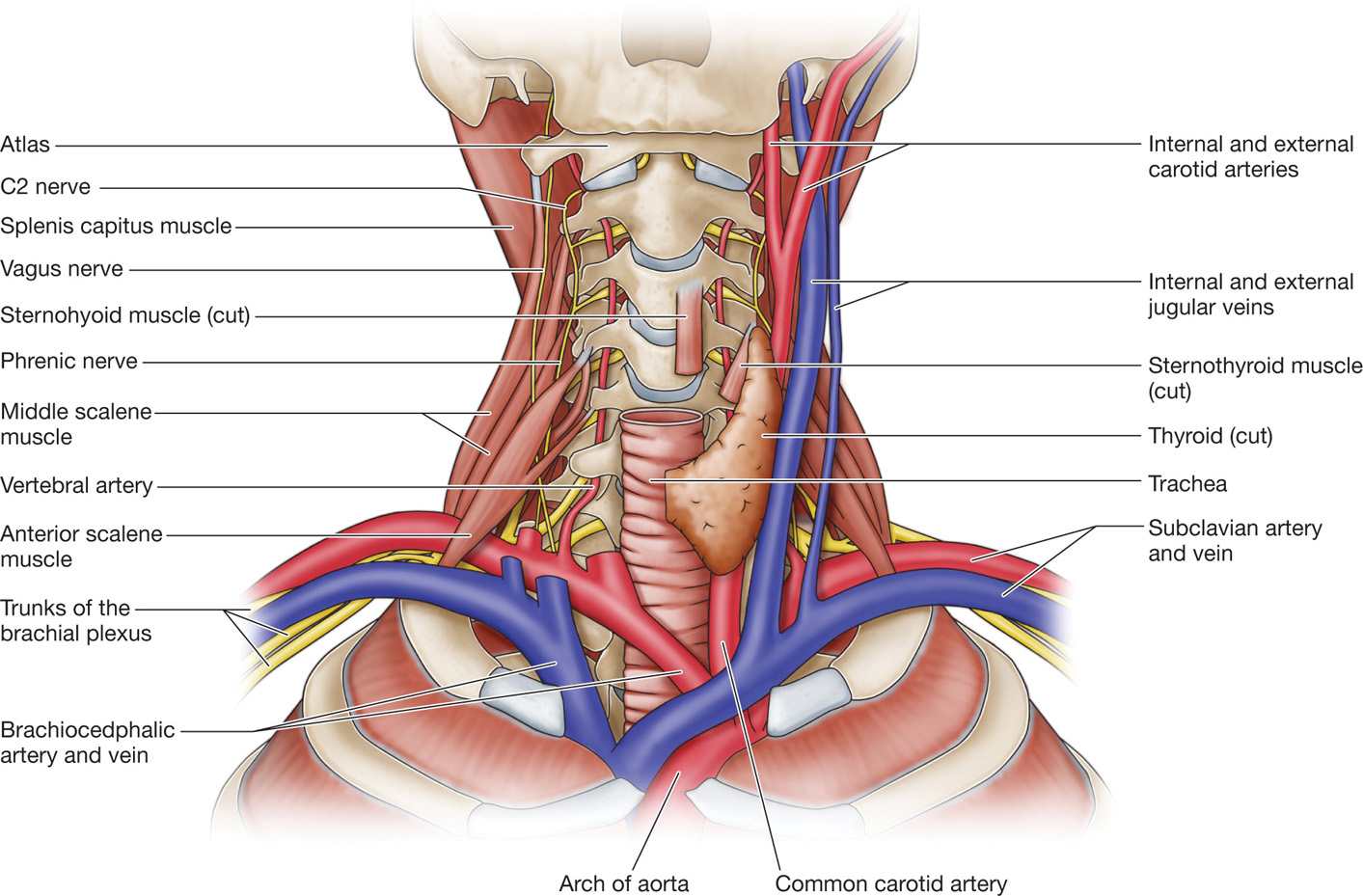
Figure 42-1. Cervical anatomy depicting cervicothoracic (stellate) ganglion. (Reproduced from Netter. Atlas of Human Anatomy. 4th ed. Plate 130, with permission.)
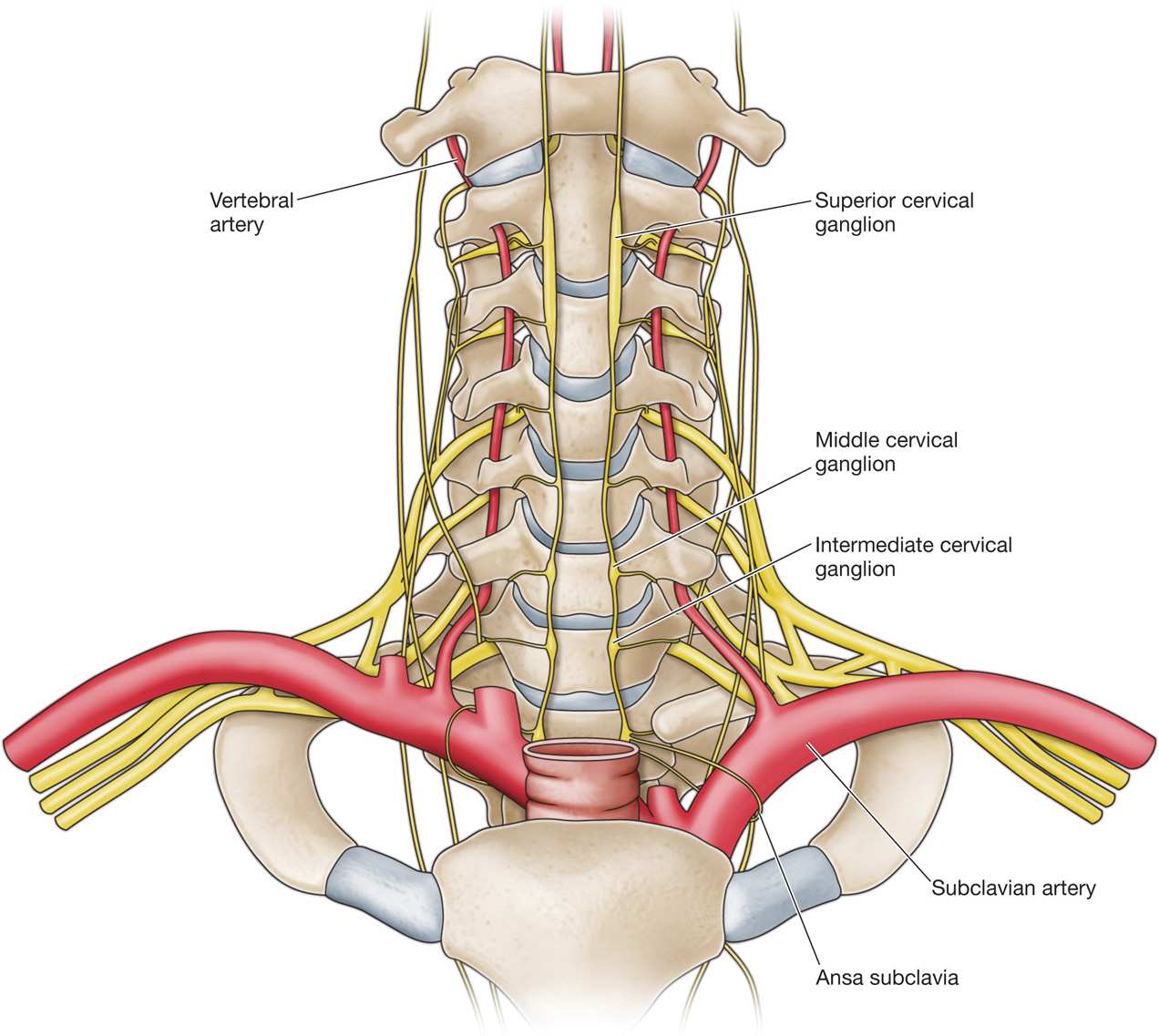
Figure 42-2. Anteroposterior view of cervical sympathetic chain and stellate ganglion lying over the longus colli muscle. (Radiofrequency Part 2 Sluijter, Fig 7-1, p. 130.)
Under fluoroscopy, the ganglion lies just lateral to the vertical line joining the uncovertebral joints in an anteroposterior view.
PREOPERATIVE CONSIDERATIONS
• Appropriate indications have been determined
• Evaluation and treatment of bleeding diathesis, contrast, or medication allergy
• Physical examination should identify previous neck or thyroid surgery, infection at the site of needle insertion, or decreased range of neck extension
• A detailed informed consent including the potential benefits and risks as well as realistic expectations of sympathetic blockade
• Possible postprocedural effects should be explained to the patient including ptosis; miosis; blurred vision; enophthalmos; anhidrosis; facial and conjunctival flushing; upper extremity numbness or weakness; contralateral blockade; and sense of dyspnea, dysphagia, or a lump in the throat
• Intravenous access for administration of fluid or medications to treat rare hypotension, seizure, or other complication
• Preprocedural sedation for anxiety depending on the individual
FLUOROSCOPIC VIEWS
• Begin with anteroposterior imaging along with a caudal tilt of the image intensifier that allows optimal visualization of the C6-C7 disc space and the C7 uncinate processes to clearly identify C7 (Figure 42-3).
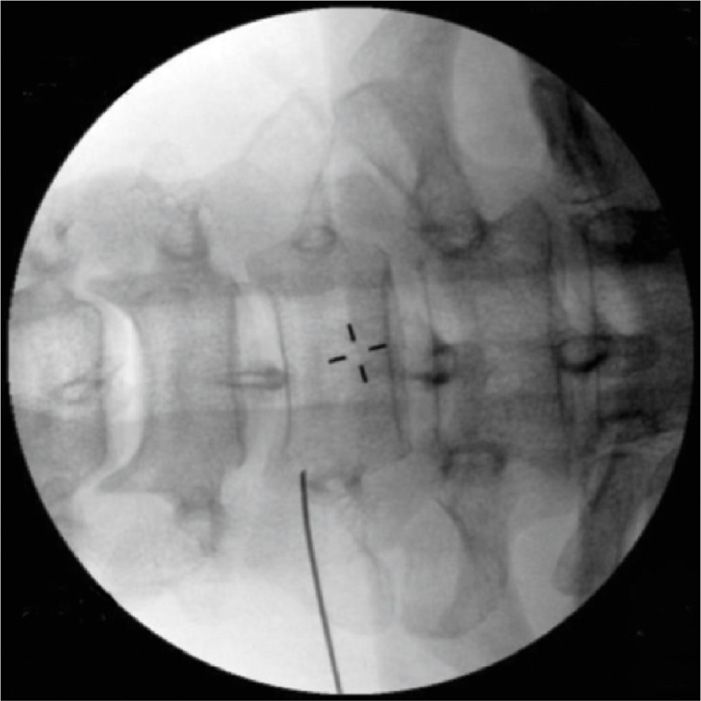
Figure 42-3. Fluoroscopic anteroposterior view with needle seen in perpendicular view at the base of the uncinate process. Note the midline spinous processes.
• For oblique approach. Then obtain an oblique image of approximately 25 to 30 degrees off the median sagittal plane to obtain a foraminal view of the lower cervical foramina. The target point is at the base of the C7 uncinate process on the anterolateral aspect of the C7 vertebral body (Figure 42-4).
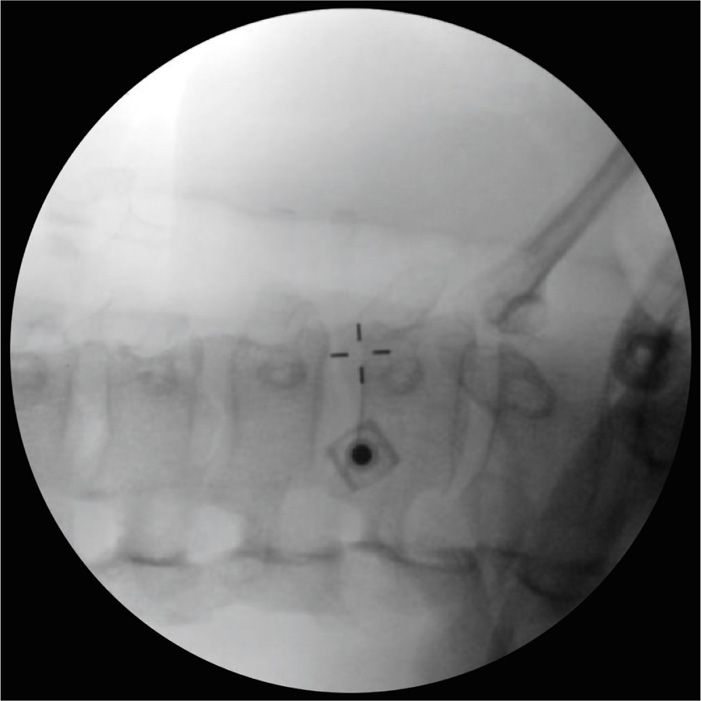
Figure 42-4. Fluoroscopic oblique view with needle seen in tunnel view at the base of the C7 uncinate process. Note the cervical foramina and the squared off superior endplate of C7.
• For anterior approach. Then identify the C6 vertebral body and Chassaignac tubercle. The target point after retracting the sternocleidomastoid muscle and carotid sheath is Chassaignac tubercle or slightly medial to this structure on the transverse process. (See Figure 42-3). Note Chassaignac tubercle which is the anterior tubercle of the C6 transverse process.
Positioning of Patient
The patient is placed in a supine position on the fluoroscopy table pad with the head neutral, or slightly rotated contralateral to the side of the procedure, and slightly extended. Arms are adducted. Pillows are placed behind the upper thorax or shoulders to promote head extension and behind the knees.
Needles and Supplies
• 22-gauge 2.5-in Chiba or stellate block needle
• 25-gauge 1.5-in needle
• 3-mL syringe for skin local anesthetic
• 3-mL syringe for contrast
• 5-mL syringe for injectate
• 12-in extension tubing
• Kelly clamp
Medications
• Preservative-free 0.25% bupivacaine or 0.2% ropivacaine or 1% lidocaine
• Iohexol 240 (nonionic water-soluble contrast)
• Triamcinolone or methylprednisolone (optional)
Equipment
• Blood pressure monitor
• Pulse oximeter
• Oxygen available
• Resuscitation equipment and medications
• Fluoroscopy (ultrasound, CT, or MRI may also be utilized)
INTRAOPERATIVE TECHNICAL STEPS
Different techniques have been described for stellate ganglion blockade.
Oblique Approach
This is the preferred technique of the author.
• The patient is placed in a supine position with a pillow beneath the upper thorax to promote head extension with the head maintained in a neutral median plane or slightly rotated contralateral to the side of the procedure.
• The skin is prepped with a 4% chlorhexidine gluconate solution three times and a sterile drape is placed with the opening over the cervicothoracic junction.
• The lower cervical and upper thoracic spine is identified under fluoroscopy.
• An anteroposterior view is obtained with a slight caudal tilt of the image intensifier to optimize the C6-C7 interspace and the C7 uncinate processes. This allows absolute identification of the C7 vertebral body (see Figure 42-3).
• An oblique view is obtained allowing optimal visualization of the lower cervical foramina. This view affords the safest approach to the target.
• A Kelly clamp is utilized as a marker on the skin for needle insertion and for holding the hub to guide the needle using tunnel vision.
• The tip of the Kelly clamp is placed on the skin at a target point where the base of the ipsilateral uncinate process meets the anterolateral C7 vertebral body.
• A 25-gauge 1.5-needle is used to inject 2 mL of skin local anesthetic (0.25% bupivacaine or 0.2% ropivacaine or 1% lidocaine).
• A 22-gauge Chiba needle with a slightly bent tip is gently advanced under intermittent tunnel vision fluoroscopic guidance until bone is contacted (see Figure 42-4).
• The contrast syringe is attached to the needle via the extension tubing and the needle is withdrawn 2-3 mL so that the tip is just anterior to the longus colli muscle.
• Following a negative aspiration for blood or cerebrospinal fluid an injection is made with 2 to 3 mL of Omnipaque 240 (Figures 42-5 and 42-6). The initial 0.5 mL of the injection is observed under real-time fluoroscopy to rule out early intravascular absorption.

Figure 42-5. Fluoroscopic oblique view with 3 mL Omnipaque 240 injected via extension tubing. Note dye spread to top of C5 and extending below T1.
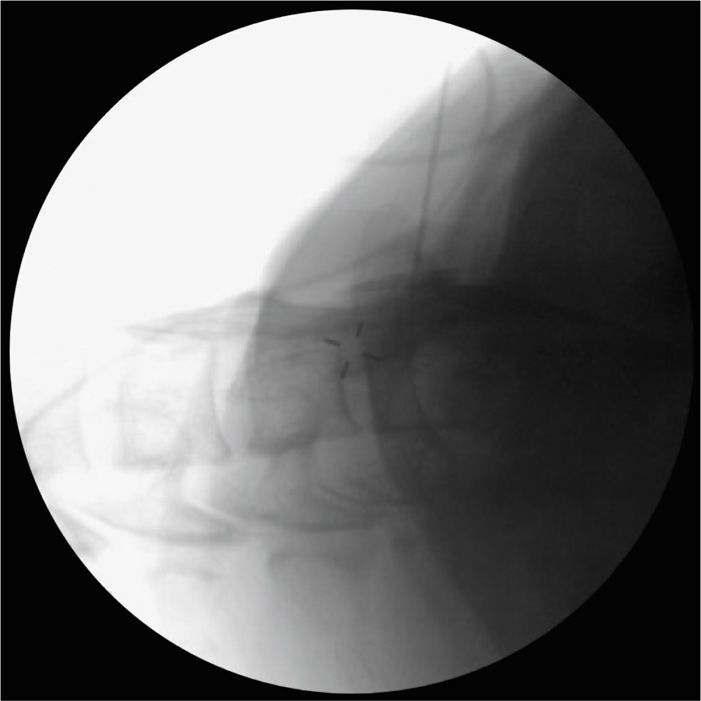
Figure 42-6. Fluoroscopic lateral view with 3 mL Omnipaque 240 injected. Note dye spread to top of C5 and extending below C7 the view is obscured by the shoulders.
• The desired contrast pattern should result in flow parallel to the axis of the spinal column. Dye spread is observed for flow down to the C7-T1 level.
• The dye syringe is removed from the extension tubing and the injectate syringe containing 4 mL of preservative-free 0.25% bupivacaine (or 0.2% ropivacaine or 1% lidocaine) with 40 mg of triamcinolone (or methylprednisolone) is attached.
• Following a negative aspiration, a 0.5-mL test dose is made.
• A slow injection with the remaining injectate is performed under intermittent fluoroscopy. Dilution of the dye is observed to visualize spread down to the C7-T1 level where the stellate ganglion is located (Figures 42-7 and 42-8).
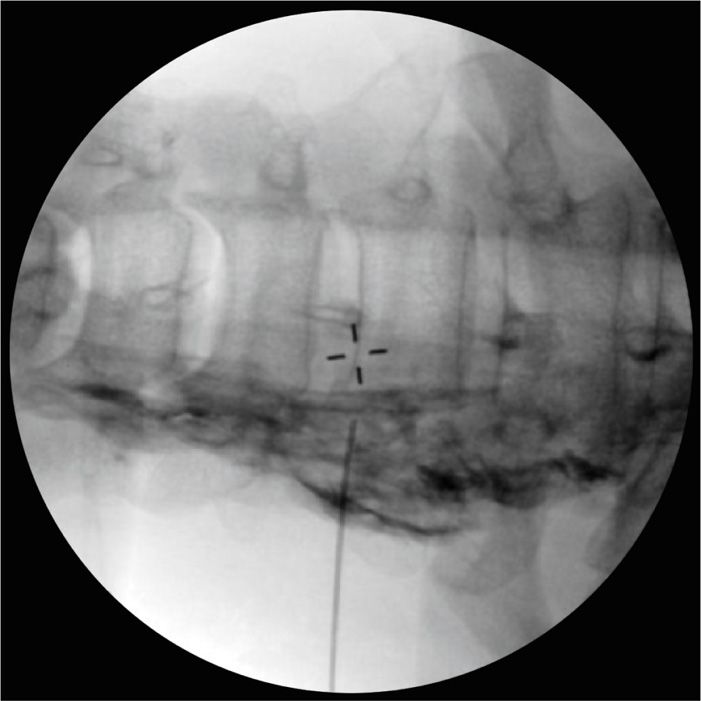
Figure 42-7. Fluoroscopic anteroposterior view with 5 mL injectate displacing Omnipaque. Note injectate spread to C4 and extending to T2.

Figure 42-8. Fluoroscopic oblique view with 5 mL injectate displacing Omnipaque. Note injectate spread to C4 and extending to T2.
• The needle may be flushed with saline and is then removed.
• A band aid or sterile dressing is applied.
Anterior Paratracheal Approach
This is the classic technique.
• For this approach the practitioner must stand on the ipsilateral side of the patient.
• The patient is placed in a supine position and the skin is prepped and draped as above.
• The lower cervical and upper thoracic spine is identified under fluoroscopy.
• An anteroposterior view is obtained with a slight caudal tilt of the image intensifier to optimize the C6-C7 interspace and the C7 uncinate processes. This allows absolute identification of the C7 vertebral body.
• The nondominant hand retracts the ipsilateral sternocleidomastoid muscle and the carotid sheath laterally (Figure 42-9).
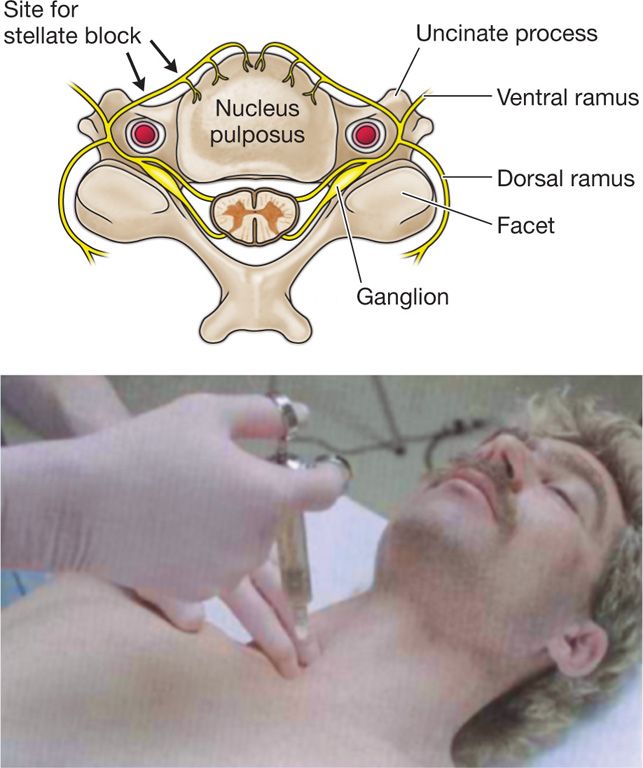
Figure 42-9. Schematic transverse view of cervical anatomy illustrating sternocleidomastoid retraction and the sympathetic chain at C6. (Reproduced with permission from Brown D, Atlas of Regional Anesthesia, 2e.)
• If a C6 procedure is desired, Chassaignac tubercle is targeted.
• If a C7 procedure is desired, the anterolateral C7 vertebral body at the base of the uncinate process is targeted.
• The remainder of the procedure is performed in a similar fashion as described above.
Posterior Approach
This is rarely used when the oblique or anterior approach is not desired (anterior neck trauma, tumor, or infection) and therefore will not be discussed further.
POSTPROCEDURE CONSIDERATIONS
• The patient should be monitored and observed for at least 30 minutes following the procedure.
• Identify if sensory or motor block is present versus selective sympathetic blockade.
• Ipsilateral temperature monitoring may be done to confirm sympathetic blockade.
• Pain score changes are recorded prior to discharge.
• The patient may be contacted the day following the procedure for follow-up and any questions or concerns.
• A discharge sheet is provided with instructions to call the pain center for any procedure-related complications.
Monitoring of Potential Complications
There are multiple dangerous structures in this region, including the carotid and vertebral arteries (Figures 42-10 and 42-11). The patient should be observed for any of the following:

Figure 42-10. Gross anatomy of stellate ganglion with cervical sympathetic and upper thoracic sympathetic chain in right anterior, slightly oblique view. At the top, small wire is exiting the vertebral artery; the attached vertical wire overlies the cervical sympathetic chain leading to the stellate ganglion (wire loop); the vertical wire caudad to the stellate overlies the thoracic sympathetic chain. (Dissection used with permission of Frank H. Willard, Ph.D.)

Figure 42-11. Gross anatomy of stellate ganglion with the thoracic sympathetic chain in lateral view. At the top a small wire comes straight out of the vertebral artery; the uppermost loop surrounds the cervical sympathetic chain; the lower loop surrounds the stellate ganglion; the vertical wire overlies the thoracic sympathetic chain; the transverse wires overlie intercostal nerves. Visualize the convergence of the lower cervical and uppermost thoracic ganglia forming the stellate ganglion within the lower loop. Note the stellate in this case is located at T1 and how posterior the thoracic sympathetic chain lies in relation to the thoracic vertebrae. (Dissection used with permission of Frank H. Willard, Ph.D.)
• Hypotension
• Bradycardia
• Dyspnea
• Hematoma
• Intravascular puncture and injection of vertebral, carotid, or subclavian arteries
• Loss of consciousness or seizure from vertebral artery injection or local anesthetic toxicity
• Intrathecal or epidural injection
• Prolonged Horner syndrome that may occur with cervical sympathetic chain or stellate ganglion blockade
• Hoarseness and dysphagia from blockade of the recurrent laryngeal nerve
• Upper extremity weakness secondary to brachial plexus blockade
• Infection or fever
• Diaphragmatic paralysis from phrenic nerve blockade
• Pneumothorax
• Thoracic duct injury
• Esophageal perforation
CLINICAL PEARLS AND PITFALLS
• Absolutely identify C7 as described above for accuracy of needle placement. If too caudal a view is utilized, one may mistake C6 for C7 resulting in inadequate block.
• Use caution at the C7 level not to target just lateral to the vertebral body where the transverse process begins, as the vertebral artery is exposed to potential puncture.
• Use of fluoroscopy and tunnel vision (eye through the needle) technique is extremely important due to the proximity of important structures including the carotid, vertebral, and subclavian arteries; cervical discs; spinal nerve roots; and the dome of the lung.
• Real-time fluoroscopy at the time of dye injection is critical to avoid unrecognized intravascular injection—especially vertebral artery injection—that may result in seizure with as little as 0.25 mL of local anesthetic.
• Small amounts of local anesthetics (3-5 mL) do not reliably block all fibers to the hands because contributions from T2 and T3 (Kuntz fibers) may be present.

Full access? Get Clinical Tree







