FIGURE 21.1 A: Sagittal MRI of the brain with gadolinium demonstrating large pineal region mass compressing the tectal plate and effacing the posterior third ventricle. B: Sagittal MRI following sitting position suboccipital craniotomy and tumor resection.
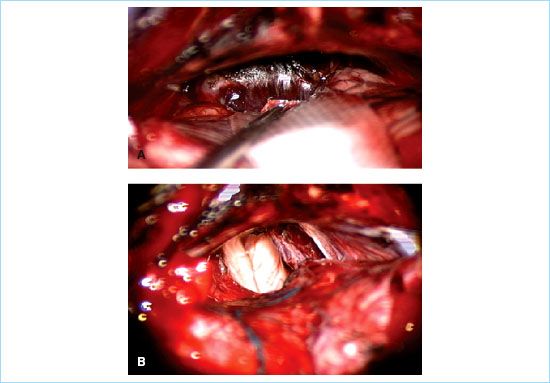
FIGURE 21.2 A: Intraoperative high magnification view of sitting position access to pineal region tumor. Note the relaxation of the cerebellar hemispheres and excellent access to the infratentorial and pineal region corridors. B: Postoperative view demonstrating complete tumor resection and exposure of the posterior third ventricle and dorsal brainstem.
1. Providing relatively comfortable direct access to superficial and deep structures (Fig. 21.1).
2. Maximum brain relaxation due to gravitational forces and optimal cerebrospinal fluid (CSF) drainage (Fig. 21.2).
3. Decreased blood loss as a consequence of reduced venous congestion.
4. Schede utilized this technique in 1905, however, Gardner in a 1935 publication credited de Martel of using this position in 1911 [1].
B. Unacceptably high complication rates forced many neurosurgeons to abandon the sitting position approach, and gave birth to several alternative routes of access including the lateral position, first described by Lester Mount in 1945 [2], and the prone position [3].
1. The lateral sitting position was described by Garcia-Bengochea in Cuba in 1956 [4]. This position utilized a modification of the sitting position. The patient is positioned such that he or she sits on the side of the operating room table, legs to the side supported by pillows, and one side of the body leaned against the OR table [4]. The lateral sitting position potentially allows the team to reposition the patient to the lateral position if unanticipated complications arise. This position was criticized by Albin for unfavorable cardiovascular alterations [5].
2. A compromise between the sitting and the prone position is the concorde position [6]. In this arrangement, the patient is positioned prone with head of the bed up to about 45 degrees, the knees flexed to about 30 degrees and the neck maximally flexed. The operating surgeon stands to either side of the patient. This position offers some of the advantages of the sitting position, direct view of the most rostral aspect of the posterior fossa, significant brain relaxation, and reduced venous congestion relative to the prone position. The most significant disadvantage is the potentially long reach and angled access for the operating surgeon.
C. Utilization of the sitting position has been on the decline, both in Europe and USA [7,8].
1. The decline is due to the complications associated with this position, such as venous air embolism (VAE), paradoxical air embolism, hypotension, and medical legal concerns [7].
2. Personal observation suggests a slow return of the sitting position. This impression is supported by a recent publication from Helsinki by Lindroos [9].
D. In addition to neurosurgery, surgical advances in shoulder surgery have increased the use of the sitting position.
1. This increase is due to frequent complications and injuries of the brachial plexus during arthroscopic shoulder surgery done in the lateral position.
2. For this reason, many orthopedic surgeons have started to perform this operation in the sitting position, which provides less strain on the brachial plexus, excellent intra-articular visualization, and the ease of converting to open procedure [10,11,12].
II. Physiologic changes in the sitting position
A. Cardiovascular changes
1. The sitting position, without anesthesia, is associated with 20% reduction in stroke volume and cardiac output; this may be compensated by rising vascular resistance from 50% to 80%. However, this compensatory mechanism may be blocked under anesthesia [13].
2. Buhre et al. [14] found a 14% decrease in intrathoracic blood volume associated with the change from supine to sitting positions without changes in total blood volume. This indicates that the drop in blood pressure and stroke volume index is due to a decrease in preload.
3. Cerebral perfusion pressure decreases by 15% in nonanesthetized patients in the sitting position. This decrease will be higher in an anesthetized patient, and can be further aggravated by jugular venous obstruction caused by unfavorable head and neck position.
1
4. In the sitting position, blood pressure at the head level is decreased by gravity. For every 1 in. of height above the heart there is approximately 2 mm Hg drop in blood pressure. Therefore we need to measure the pressure at the head level or make calculations to compensate for measurement at a different body level.
5. The reason for the relationship between height and blood pressure is the higher density of mercury, which is 13.54562 g/cm3 at 20°C compared to that of water.
6. If only noninvasive cuff pressure is used, then calculations to compensate for height differences should be used to avoid cerebral ischemia.
7. The lack of such compensation may mask cerebral hypotension, leading to cerebral ischemia and postoperative neurologic deficits [13].
8. Improper position may lead to hypotension caused by blood pooling which is magnified during the use of potent anesthetic agents that promote vasodilation.
9. Hypotension in patients having surgery under general anesthesia in the sitting position requires treatment with vasopressors to maintain cerebral blood flow which can be maintained as long as mean blood pressure is kept above 70 mm Hg [15].
B. Respiratory changes
1. Spontaneous ventilation and changes in ventilatory patterns have been used to monitor brainstem function during surgery in the posterior fossa until it was replaced by cardiovascular parameters. However, recently there has been a report of using spontaneous ventilation to monitor surgery done in the sitting position [16].
2. Hyperventilation and low CO2 are not recommended during surgery in the sitting position due to the relatively lower intracranial pressure (ICP) in the sitting position and possible cerebral ischemia caused by severe vasoconstriction.
C. Intracranial pressure
1. The sitting position is ideal for patients with increased ICP since it facilitates blood return to the heart and shifts CSF to the spinal canal.
2. Such decrease in ICP is enhanced by proper neck and head position which enhances venous drainage [13].
III. Placing the patient in sitting position
A. Preparation
1. Sitting position starts with the patient supine. After all lines are inserted and monitors applied, the patient will be moved to the sitting position.
2. Lines inserted include arterial line, multiorifice central line, intravenous lines, and urinary catheter.
2
3. The central line is inserted either via the central vessels or in the antecubital veins. The tip location of the multiorifice catheter is confirmed by x-ray, pressure transducer (obtain ventricular pressure tracings and pull back to the junction of the superior vena cava to the atrium), or by utilizing the EKG and connecting lead five to the special adaptor at the end of the catheter to locate the biphasic P-wave (Fig. 21.3).
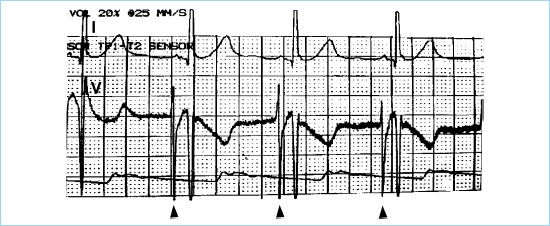
FIGURE 21.3 EKG, upper tracing is from lead I while lower tracing is from lead V which shows the biphasic P-wave. The biphasic P-wave is recorded from the metal adaptor located at the distal CVP line and reflecting signals at the tip of the multiorifice, saline-filled CVP line.
4. Recording of the EKG from the central venous pressure (CVP) is facilitated by removing any air bubbles in the line and by filling the catheter with 7.5% sodium bicarbonate solution.
B. Positioning
1. The Mayfield head holder will be placed, the table sections will be adjusted by flexing the table in the middle toward 90 degrees and lowering the legs section at the knees by 30 degrees. The table head section is brought upward. During the previous movements, the table may be brought into Trendelenburg position to further help achieving the sitting position by allowing the head section more room to move. In this position, the knees will be at the level of the heart to minimize the drop in blood pressure.
2. Once the table is in position, the arch bar located toward the feet, which have the holding part, will be extended to connect securely with the Mayfield frame (Fig. 21.4). The arch bar can be placed on the same back section of the table where the patient’s back is resting. This will eliminate accidental movement of the table which can put strain on the head. However, applying the normal-size arch bar at this location may be difficult and can generate pressure on the patient body trunk. The second location to place this bar is toward the end of the second section of the table where the patient is sitting.
3. Once the patient is in the sitting position, special attention is paid to the table movements. It is important to move the table as a unit and not to move sections of the table which can severely damage the cervical spine. Special attention is directed to the head–neck position to secure good blood drainage, assure free airway, and unkinked endotracheal tube. Attention, also, should be directed to the cross table bar, which holds the Mayfield frame, and to the straps to prevent pressure injuries which can be minimized by proper padding of the patient’s body pressure points.

FIGURE 21.4 Patient in sitting position with BP transducer at head level, CVP transducer at heart level, arm comfortably on the abdomen.
CLINICAL PEARL
Once the patient is in the sitting position, special attention should be directed to table movements to prevent accidental neck movements.

Full access? Get Clinical Tree







