Sinus Infections in the Ventilated Patient: Introduction
Infection of paranasal sinus cavities is a well-recognized cause of fever in mechanically ventilated patients.1–7 Easy to detect in maxillary sinuses, the infectious process also frequently involves ethmoid, frontal, and sphenoid sinuses8 where the diagnosis is more difficult to establish.9 Infectious sinusitis represents an important reservoir of bacteria10 that may disseminate into the respiratory tract11 and intracranially.12 In contrast to community-acquired sinusitis, ventilator-associated sinusitis is often clinically silent in sedated critically ill patients and may be underdiagnosed if not systematically screened for in the presence of fever of unknown origin. In the absence of diagnosis and appropriate treatment, bacteremia,2,5 ventilator-associated pneumonia,13 and life-threatening complications, such as orbital infection,14 meningitis, mastoiditis, cerebral abscess, or thrombosis of the sinus cavernosus, may result.12 Early detection and treatment of infectious maxillary sinusitis significantly reduces the incidence of ventilator-associated pneumonia and may decrease intensive care mortality.11
Physiology of Paranasal Sinuses
Located at the entry of the respiratory system, paranasal sinuses and the nose serve to humidify, filter, warm, and sense inspiratory gas.15,16 A number of other presupposed physiologic roles have not yet received firm scientific confirmation.17 Among them, the most popular are that paranasal sinuses help lighten the bones of the skull, improve the resonance of the voice, serve as a sound box for opera singers, increase the surface area of the olfactory membrane, serve as shock absorbers in mechanical impacts, protect against high pressure in the nasal region when sneezing, act as thermal insulators of the brain, and promote facial growth and architecture. More simply, paranasal sinuses might be considered as evolutionary relics or faults, whose form results from the influence of the forces created during the act of chewing.
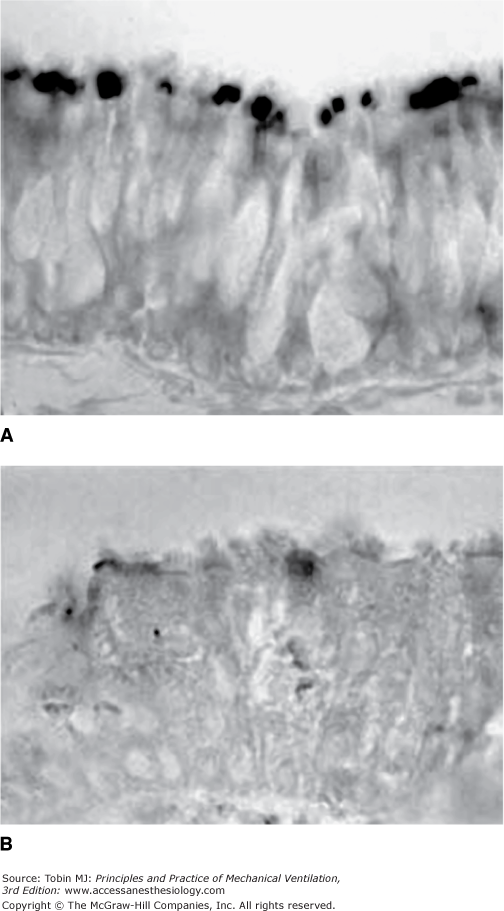
Large amounts of nitric oxide are produced in human paranasal sinuses18,19 and permanently released in the upper airways through the different ostia that link antral cavities to the nostrils.20 As shown in Figure 47-1, an inducible form of nitric oxide synthetase is present in cilia and microvilli of the maxillary sinus epithelium of healthy volunteers.18,19 Significant nitric oxide concentrations are also found in the exhaled gas of guinea pigs, pigs, rhesus monkeys, rats, rabbits, horses, and Asian elephants, all species possessing open paranasal sinuses.20–24 Interestingly, seals and baboons, which do not have open paranasal sinuses, do not exhale nitric oxide,25,26 thus confirming that pneumatic facial cavities play a critical role in the nasal production of nitric oxide in mammals. Humming, by accelerating gas exchange in sinus cavities, markedly increases exhaled nasal nitric oxide27 whereas moderate exercise has an opposite effect.28 Nitric oxide produced in the paranasal sinuses likely has an important role in host defense against inhaled pathogens, in the optimization of ventilation–perfusion ratios during normal breathing,29 and in the regulation of ciliary motility.30,31
Figure 47-1
Immunoreactive sinus inducible nitric oxide synthetase distribution is represented in black on biopsy samples from maxillary sinus epithelium. In a healthy subject (A), a strong immunoreactivity is detected in the apical part of the ciliated epithelial cells near the surface. In a patient with radiographic maxillary sinusitis (B), the signal is weaker or absent. (Reprinted with permission of the American Thoracic Society. Copyright © 2012 American Thoracic Society. From Deja M, Busch T, Bachmann S, et al. Reduced nitric oxide in sinus epithelium of patients with radiologic maxillary sinusitis and sepsis. Am J Respir Crit Care Med. 2003;168:281–286. Official Journal of the American Thoracic Society.)
Each paranasal sinus communicates with the corresponding nostril by an ostium, which provides aeration of the antral cavity. Bacteria are present in nasal secretions covering the mucociliary epithelium and on the gingival mucosa and its crevices. Microorganisms may enter the maxillary cavity by the canine fossa and the inferior meatus. Paranasal sinuses, however, are normally sterile32 as a result of two different protective mechanisms. First, the antral mucosa is covered with a protective mucus layer produced by goblet cells. Bacteria penetrating into the maxillary cavity are immediately enveloped by mucus and moved rapidly to the sinus ostium by respiratory cilia. Second, the antral concentrations of nitric oxide exert a bacteriostatic effect. Many pathogens are sensitive to nitric oxide in concentrations less than 1 part per million.33–36 The antral concentrations of nitric oxide, produced by the maxillary epithelium, are equal to or greater than 2 parts per million and likely contribute to antral sterility.32
Pathogenesis and Predisposing Factors
Pathogenesis of radiographic sinusitis diagnosed in intubated and tracheostomized patients is incompletely understood.
Rabbits have large and accessible nostrils and their sinuses show anatomical similarities to those of humans. In this species, sinuses consist of a number of cavities connected to each other and can be considered as one, called the maxillary sinus.37 Historically, the first experimental model was created by opening the maxillary sinus through an anterior wall antrostomy, gluing and closing the natural ostium, and injecting bacterial strains directly supress “injected” into the maxillary cavity.38 Although the model is extremely reliable for producing purulent sinusitis, it causes a traumatic injury that questions its relevance for human sinusitis. As a consequence, a rhinogenic model was proposed in the late 1990s and remains to date the reference:39,40 a foreign body—an endotracheal tube,41 a catheter,42 or a sponge impregnated or not with bacteria43—is implanted into nostrils for a period of time ranging from several days to several weeks. In the rhinogenic rabbit model, computed tomographic evidence of maxillary sinusitis is detected at the sixth day following foreign-body nasal placement.43
A number of lessons can be drawn from experimental studies. Direct or indirect obstruction of the ostia rapidly induces an acute sinus inflammation. The intranasal placement of a foreign body over several days results in purulent sinusitis, characterized by the accumulation of a thick and purulent discharge within the sinus cavity.43 Initial histologic lesions are made of inflammation and exudation of maxillary mucosa; the number of goblet cells increases, augmenting mucus production and causing fluid accumulation within the cavity. Then, inflammatory polyp formation is observed,41,43,44 associated with permanent loss of cilia, squamous metaplasia, and fibrosis.43,45 The risk of sinusitis increases with the nasal catheterization period and the size of the intranasal catheter.41,42 Relief of ostial obstruction promotes resolution of radiographic sinusitis within a few days,46 whereas sinus inflammation persists for several weeks.43 Over time, the fluid-filled maxillary cavity is contaminated41 or infected43 by species present in the adjacent nostril.41 Surprisingly, bacteria impregnating the intranasal sponge are rarely found in the nasal cavity and are often replaced by bacteria belonging to the normal flora of the rabbit nostrils.43,47
Finally, the following sequence may lead to bacterial sinusitis. First, the presence of a nasal foreign body induces an ipsilateral inflammatory antral disease. Second, mucus accumulates within the antral cavity because of goblet cell proliferation, impairment of mucociliary clearance, and ostial obstruction. Third, the antral contents are contaminated and infected by microorganisms issued from the nostrils whose proliferation into the sinus cavity is facilitated by the lack of regional nitric oxide production.
Only a few studies have reported macroscopic and histologic disorders characterizing radiographic maxillary sinusitis in critically ill patients.19,48–50 In thirty-three neurosurgical patients receiving prolonged mechanical ventilation with radiographic maxillary sinusitis, antroscopies were performed by the canine fossa route.49 Most of radiographic maxillary sinusitis corresponded to “inflammatory” sinusitis, with the antral cavity filled with thin and transparent secretions and/or gelatinous and transparent mucus with a neutral smell. In a minority of patients, bacterial sinusitis was diagnosed as the presence of viscous and opaque pus with a foul smell. Both types of sinusitis were associated with varying mucosal reactions, ranging from pallid to vermilion edema with different degrees of transparency. Interestingly, in two patients with “inflammatory” sinusitis and one patient with bacterial sinusitis, maxillary mucosa was macroscopically normal. When present, mucosal edema always included the medial side with the ostial region.49 Biopsy specimens of antral mucosa revealed various grades of inflammation. Acute inflammation involving the maxillary epithelium, the connective tissue, and the vessels with a massive infiltration by polymorphonuclear neutrophils was observed in patients with bacterial maxillary sinusitis. In patients with “inflammatory” sinusitis, mild inflammation was observed, characterized by a moderate cellular infiltration of the connective tissue with a massive infiltration of vessels by eosinophils.48
Several prospective and retrospective studies have shown that the occurrence of radiographic sinusitis has a higher incidence in the antrum adjacent to nasotracheal and nasogastric tubes than in the nonadjacent sinus.3,4,6,7,51–62 The presence of a nasogastric tube for enteral feeding appears as an independent risk factor.63 As in experimental sinusitis, the presence of a foreign body within the nostrils creates an ostial obstruction that initiates sinus inflammation and mucus accumulation within the sinus cavity. Confirming experimental data,42 a large endotracheal tube induces radiographic sinusitis more frequently and faster than a small nasogastric tube.55,58 In addition, the plastic nasotracheal tube is the site of biofilm formation for bacteria with adhesive capacity and enhanced pathogenicity:64–66 microorganisms adhere to the internal and external surfaces of the endotracheal tube and some species exude an exopolysaccharide that acts as a slimelike adhesive.67 Bacteria encased in this biofilm become partially resistant to the action of antimicrobials and host defences.68,69 The bacterial proliferation around nasal foreign bodies forms a reservoir from which microorganisms penetrate into the antral cavity.41
Ostial size, upon which drainage and ventilation of the sinus cavities depends, can markedly vary from one patient to another.70 In humans, supine position is known to reduce ostial patency71 by inducing swelling of the ostiomeatal complex.72 A functional ostial area less than 5 mm2 induces hypoventilation of the maxillary cavity, local hypoxia, decrease in mucosal blood flow, and predispose to maxillary sinusitis by impairing mucociliary clearance.73
Generalized sepsis, well known for stimulating numerous tissue-inducible nitric oxide synthetases, inhibits the nitric oxide metabolic pathway at the maxillary level.19 Autoinhaled nitric oxide plays an important antiinflammatory and antiviral role in colds.74 Community-acquired, as well as ventilator-associated, sinusitis decreases exhaled nasal nitric oxide19,75,76 by reducing its antral production (see Fig. 47-1). Sepsis originating in other organs also markedly inhibits the antral production of nitric oxide through downregulation of inducible nitric oxide synthetase messenger ribonucleic acid.19 The sepsis-induced reduction of antral nitric oxide concentrations contributes to impaired mucociliary clearance and decreased perfusion of the maxillary epithelium, both factors that facilitate infection of the maxillary cavity by impairing bacterial cleansing.77
Epidemiology and Complications
In critically ill patients, the reported incidence of radiographic sinusitis varies from 25% to 75%.78 More than 80% of radiographic abnormalities of the maxillary sinuses are associated with radiographic abnormalities of the ethmoid, sphenoid, and frontal sinuses.8,79 Variability in the estimated incidence stems from the many radiographic techniques used for diagnosis: Conventional radiography is much less accurate than computed tomography or maxillary ultrasound. After 12 hours of nasal endotracheal intubation and/or nasogastric tube placement, 38% of critically ill patients have computed tomographic evidence of radiographic maxillary sinusitis.8 Among factors other than the presence of a foreign body in the nostrils, the supine position, head63 and/or facial trauma,51,53,80 allergy, and sepsis have been incriminated.80 After 7 days, the incidence of radiographic maxillary sinusitis increases to 80%.8 Infectious sinusitis is less frequent than radiographic sinusitis, occurring only in 20% to 30% of patients intubated longer than 7 days.79 Its incidence is higher in nasotracheally than in orotracheally intubated patients.8
A link between infectious maxillary sinusitis and bronchopneumonia has been established experimentally.47,82 In critically ill patients, nosocomial sinusitis is considered a major cause of ventilator-associated pneumonia.8,13,56,62 In a randomized study assessing a systematic search for sinusitis in nasotracheally ventilated patients, the incidence of ventilator-associated pneumonia was significantly higher in the control group than in the study group, where infectious maxillary sinusitis was systematically sought and treated, when confirmed, by sinus drainage and intravenous antibiotics.11 In addition, the mortality rate significantly decreased from 46% in the control group to 36% in the study group. Although the association between nosocomial sinusitis and ventilator-associated pneumonia appears highly likely, the frequent discordance between microbiologic results from sinus and lower airway cultures8,11 suggests that these two infections may also arise simultaneously and independently because of shared risk factors and diminished host defense for infection. A heavily contaminated nasopharynx may be the common bacterial reservoir from which sinuses and lungs are infected. Conversely, antral infection, characterized by high concentrations of microorganisms,8 can also be a reservoir from which the oropharynx, the tracheobronchial tree, and the lung parenchyma are secondarily infected. Interestingly, concentrations of nitric oxide in the maxillary and nasal cavities markedly increase as infectious maxillary sinusitis is treated with antibiotics and sinus lavage.83 The restoration of normal local concentrations of nitric oxide, by reestablishing maxillary ciliary function and immune defense, may help in preventing maxillary cavity superinfection and eliminating one of the risk factors for ventilator-associated pneumonia.
Diagnosis
Unlike clinical symptomatology of community-acquired maxillary sinusitis, clinical signs of ventilator-associated maxillary sinusitis are scarce and of limited specificity.78 General signs of infection such as fever and leukocytosis have poor specificity. Mucopurulent nasal discharge is evocative but of limited sensitivity.51 Frontal headache is often blunted by sedative drugs aimed at facilitating mechanical ventilation. As a consequence, ventilator-associated maxillary sinusitis cannot be reliably detected on clinical signs alone and should be systematically sought in the presence of fever of unknown origin.4,11,84
Rather than standard sinus radiography using the Blondeau’s view performed in the upright position, sinus ultrasound is the first diagnostic tool for demonstrating community-acquired acute maxillary sinusitis in ambulatory and spontaneously breathing patients, and ventilator-associated maxillary sinusitis in ventilated patients lying in the supine position.85,86
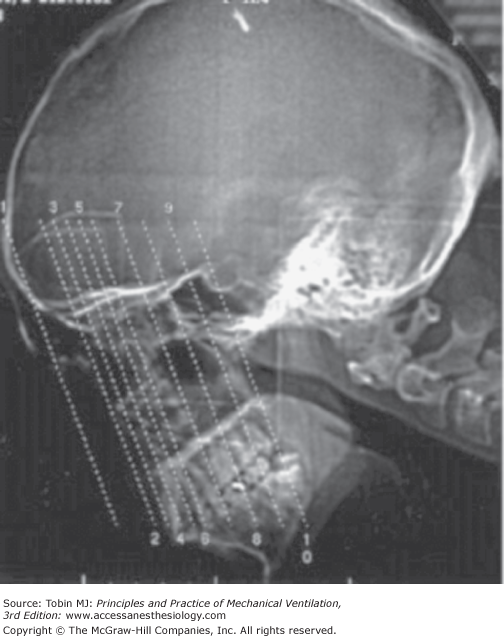
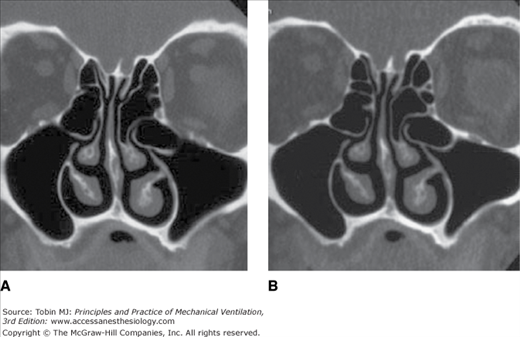
Paranasal computed tomography is the reference technique for establishing the diagnosis of radiographic sinusitis.8,87–91 A low-dose computed tomography examination is preferred to avoid excessive radiation exposure.91 Ten thin, noncontiguous computed tomography sections, using an initial interslice gap of 15 mm aimed at avoiding direct radiation to the eye lens (Fig. 47-2), should be performed. Such a technique decreases radiation exposure by more than 90% without seriously affecting the quality of the images (Fig. 47-3).
Figure 47-2
Scout view with different interslice gap between the 10 slices of the low-dose computed tomography protocol recommended for diagnosis of radiographic sinusitis. (Reproduced, with permission, from Hagtvedt T, Aalokken TM, Notthellen J, Kolbenstvedt A. A new low-dose CT examination compared with standard-dose CT in the diagnosis of acute sinusitis. Eur Radiol. 2003;13:976–980. With kind permission from Springer Science and Business Media.91)
Figure 47-3
Standard-dose. (A) compared to low-dose (B) computed tomography images of normal ethmoid and maxillary sinuses obtained in a coronal plane through the ostiomeatal complex. (Reproduced, with permission, from Hagtvedt T, Aalokken TM, Notthellen J, et al. A new low-dose CT examination compared with standard-dose CT in the diagnosis of acute sinusitis. Eur Radiol. 2003;13:976–980. With kind permission from Springer Science and Business Media.)

Full access? Get Clinical Tree