Fig. 30.1
“Bent inner tube” sign associated with sigmoid volvulus. Published with permission from William Herring, MD, FACR, learningradiology.com
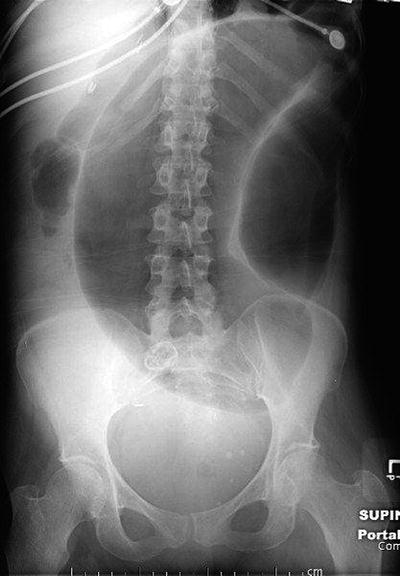
Fig. 30.2
“Omega” sign associated with sigmoid volvulus. Published with permission from William Herring, MD, FACR, learningradiology.com
Management
The initial management of sigmoid volvulus involves preparing the patient for intervention. Typically, patients are volume depleted and may have electrolyte abnormalities. A nasogastric tube and urinary catheter should be inserted. Broad spectrum antibiotics are recommended due to the potential for bacterial translocation through the compromised bowel wall. Depending on the severity of systemic manifestations, central venous pressure (CVP) monitoring should be considered to help guide in the resuscitation.
A proposed algorithm for the management of sigmoid volvulus is presented in Fig. 30.3. Since the publication of Bruusgaard’s article in 1947, nonoperative decompression is considered the initial treatment of choice for patients with sigmoid volvulus. However, the first decision that must be made is whether or not the patient is a candidate for nonoperative reduction. If there is any evidence that the patient has colonic ischemia, there should be no delay in operative treatment and the patient should proceed immediately to surgery. These patients should not have an attempt at endoscopic reduction. Mortality rates for patients with sigmoid volvulus increase dramatically in the presence of compromised bowel. In a study published more than 100 years ago by Moynihan looking at patients with sigmoid volvulus, mortality was 80% in patients with gangrenous bowel as compared to 10.6% in patients with viable colon [9]. This has not changed dramatically. In 2000, Madiba and Thompson cited an overall 38% mortality rate in patients with gangrenous colon, which (similar to the Moynihan study) is eight times higher than the mortality rate for those with viable bowel [10].
Fig. 30.3
Algorithm for the management of sigmoid volvulus
Patients with peritonitis or any signs of bowel ischemia should proceed directly to the operating room. Likewise, patients who fail endoscopic decompression or those that have evidence of ischemia on endoscopic evaluation also require surgical resection. The type of operation in this case will depend on the viability of the colon and the patient’s clinical condition. Although there are reports describing non-resectional operations for sigmoid volvulus such colopexy, mesosigmoidoplasty and laparoscopic fixation, they are not considered standard and are beyond the scope of this chapter. Therefore, only resectional options are discussed. If the colon is viable at the time of operation it is appropriate to proceed with sigmoid resection and primary anastomosis. The extent of sigmoid resection should be limited to the area of sigmoid colon that is redundant and freely mobile. If the bowel is ischemic and/or the patient is hemodynamically unstable, the operation of choice is a sigmoid resection and end colostomy (Hartmann procedure). As stated previously, if the volvulus has progressed to the point of intestinal gangrene at the time of colectomy the mortality rate is extremely high (50–80%). Cirocchi et al. reviewed 23 patients with sigmoid volvulus and separated them into two groups: patients who were completely obstructed and those with symptoms considered “sub-occlusive.” The mortality rate in the obstruction group overall was 44% but increased to 57% in patients who had signs and symptoms of peritonitis and required sigmoid resection with end colostomy. In the group with sub-occlusive symptoms, mortality increased from 35 to 50% in patients with a delayed diagnosis who required sigmoid resection with end colostomy [11].
If there is no evidence of ischemia, the first step in management is endoscopic detorsion. As mentioned previously, in the Bruusgaard series, reduction was achieved 123 times with a combination of proctoscopy and rectal tube placement. A review of 19 American series involving a total of 596 patients also confirmed that endoscopic decompression is successful in the majority of cases. In these patients, nonoperative reduction was successful 417 times. Nineteen percent of cases were reduced with proctoscopy, 40% with a combination of proctoscopy and rectal tube and 0.2% with colonoscopy [1]. A more recent study, published in 2010 by Tan et al. reviewed their 9-year experience with sigmoid volvulus. Seventy-one patients were admitted 134 times for acute sigmoid volvulus. The authors were able to achieve endoscopic decompression with a success rate of 78%. They used flexible sigmoidoscopy as their modality of choice. Decompression with a rectal tube only was successful in 57.1% of cases. Their results also reinforce the benefits of endoscopic decompression as the mortality rate for emergency surgery in their series was 17.6% [12].
Endoscopic decompression may be performed with either a rigid or flexible scope. An advantage of the flexible scope is that it is longer and easier to maneuver. The rigid scope, however, allows for the placement of a rectal tube through the lumen of the scope. The patient should be positioned supine, on their left side with knees flexed towards the chest. The scope is gently inserted through the anus and advanced slowly to the point of obstruction. The most common location of obstruction is around 15 cm above the anal verge. It should be noted that if there is any evidence of intestinal ischemia or necrosis, the scope should be terminated and the patient taken immediately to the operating room. In the case of viable mucosa, gentle insufflation and advancement is employed until the loop of colon is decompressed. This is usually verified by the scope passing into a more dilated segment of colon along with a return of flatus and stool. The evacuation of flatus and stool may be immediate so the practitioner should be prepared and dressed in a gown, gloves and mask. When using the rigid scope, a rectal tube can be inserted via the lumen. If a flexible scope is used it should be gently withdrawn and a rectal tube advanced. It is appropriate to use either a red rubber catheter or Foley catheter as the rectal tube. This must be secured to the thigh or perineal region to prevent dislodgement and left in place for 48–72 h. Fig. 30.4 shows successful decompression of the colon after rectal tube placement.


Fig. 30.4
Decompressed sigmoid colon after rectal tube placement. Published with permission from William Herring, MD, FACR, learningradiology.com
Although nonoperative reduction of sigmoid volvulus spares the patient emergent surgery, it is not considered definitive treatment as patients decompressed by endoscopy are likely to recur. In a study from Northwestern, the recurrence rate after endoscopic decompression was 90% [13]. In the Tan study, the rate of recurrence after successful nonoperative reduction was 60.9%. Furthermore, a 15.4% mortality rate is associated with detorsion without resection. Brothers et al. reviewed 39 patients with colonic volvulus over a 9-year period. Twenty-nine attempts were made at reduction with either colonoscopy or sigmoidoscopy with a success rate of 55%. The recurrence rate after successful decompression, however, was 57% [14].
Endoscopy is a temporizing measure that allows the patient to be prepared for elective resection, ideally with primary anastomosis. Once detorsion is achieved, the patient can be adequately hydrated and undergo bowel preparation for surgery scheduled during the same hospital admission. Elective resection would proceed as described previously with removal of the redundant and freely mobile segment of sigmoid colon involved in the volvulus. This procedure is associated with low morbidity and mortality rates and an approximately 5% anastomotic leak rate. In a small percentage of cases, the remaining colon is massively dilated (megacolon) as a result of the distal obstruction caused by the volvulus. If megacolon is present and there is concern for the viability of the remaining colon, the surgeon should consider a total abdominal colectomy with either ileo-rectal anastomosis or end ileostomy and planned reconstruction at a second operation. This is a rare circumstance and typically not encountered at operation for sigmoid volvulus.
Summary
Sigmoid volvulus is a clinical entity that has been recognized and treated since ancient times. It is a surgical emergency that the practicing acute care surgeon must recognize and treat promptly. Diagnosis is based on physical exam findings in combination with radiographic imaging. As mentioned previously, patients with evidence of bowel ischemia must proceed directly to the operating room without delay. In the absence of signs of bowel ischemia, the initial treatment is endoscopic decompression followed by definitive operative intervention. Overall the patients who have the best outcomes after sigmoid volvulus are those that undergo successful endoscopic detorsion followed by resection and primary anastomosis of prepared bowel on the same hospital admission.
Cecal Volvulus
Epidemiology
Cecal volvulus was first described by Hildanus in the sixteenth century and later by Rokitansky in 1837. It is a surgical emergency, resulting from an axial twist of the cecum, distal ileum and proximal colon around a mesenteric pedicle. It is the second most common location for colonic volvulus following the sigmoid and is responsible for 20–40% of all cases. The overall incidence of cecal volvulus in the general population is approximately 2.8–7.1 million people per year [5]. Unlike sigmoid volvulus in which the predisposing anatomic factors are acquired, cecal volvulus has a congenital etiology. The right colon is a midgut structure that initially leaves the abdominal cavity during fetal development and rotates counterclockwise around the superior mesenteric artery. When the midgut structures return to the abdominal cavity at 9 weeks gestation, the ascending colon assumes a fixed retroperitoneal position. Patients who present with cecal volvulus have a mobile cecum that lacks normal retroperitoneal fixation. In a review of 125 cadavers at Northwestern, 11.2% were found to have freely mobile right colons and 25.6% had enough cecal mobility to allow volvulus to occur [5].
The age, geographic distribution, and predisposing factors of patients who present with cecal volvulus are different than those with sigmoid volvulus. In 1949, Donhauser reviewed 100 patients with cecal volvulus; the mean age of presentation was 40 [16]. Rabinovici and colleagues reviewed 561 cases of cecal volvulus from 1959 to 1989. This is the largest review in the literature to date. The mean age at presentation was 53.3 years and there was a slight female predominance [15]. In the Ballantyne series of 71 patients with cecal volvulus, the mean age at presentation was 59 years and the authors also noted a female-to-male predominance (59% versus 41%) [5]. More recent literature reflects an increase in age at presentation but this may be due to the aging of the population. Cecal volvulus is more prevalent in India where it accounts for 4.3% of cases of acute obstruction. In the United States, Britain and Western Europe, cecal volvulus is the cause of 1% of acute obstructions [7].

Full access? Get Clinical Tree







