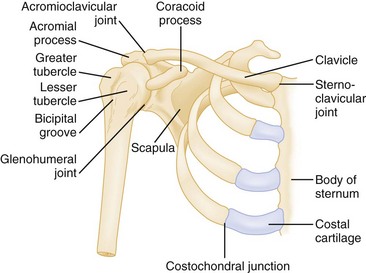
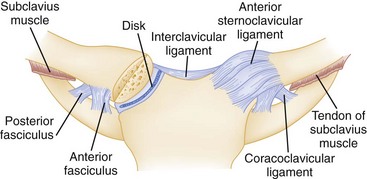
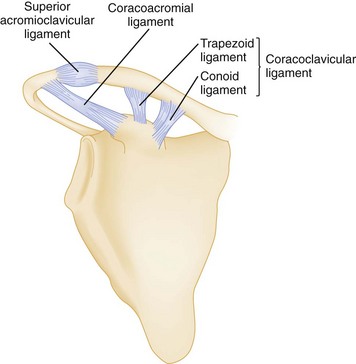
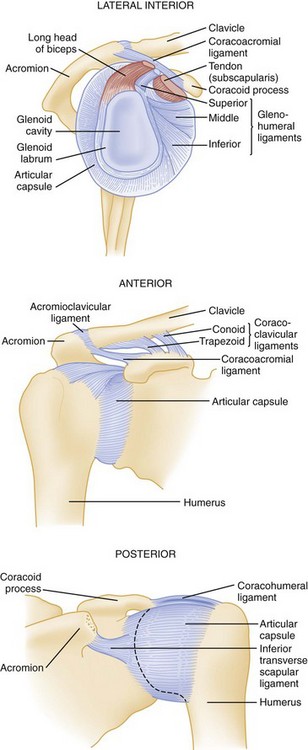
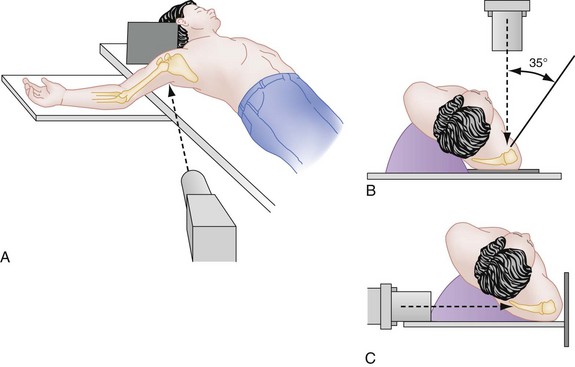
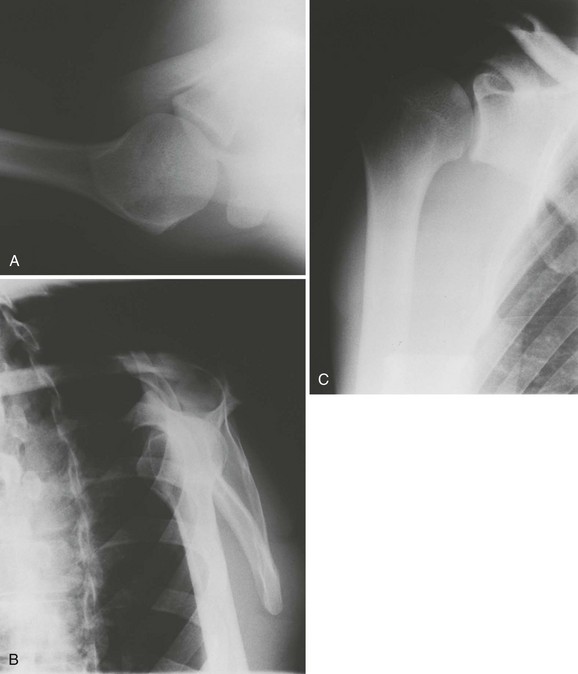
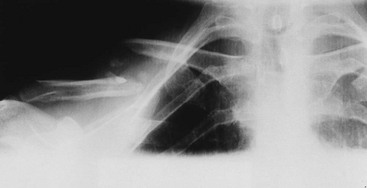
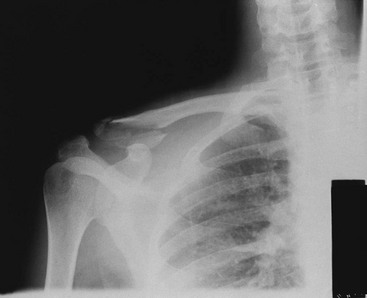
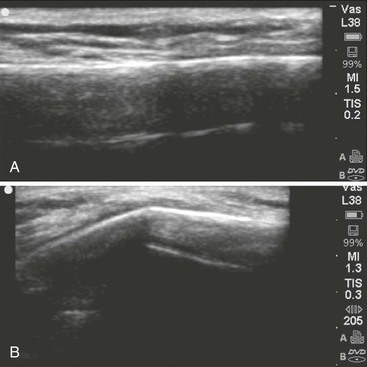
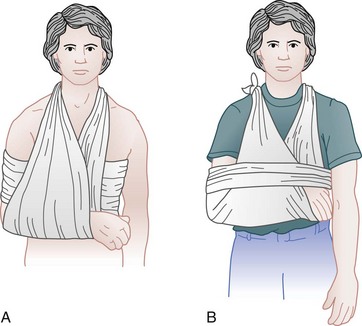
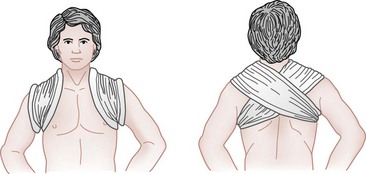
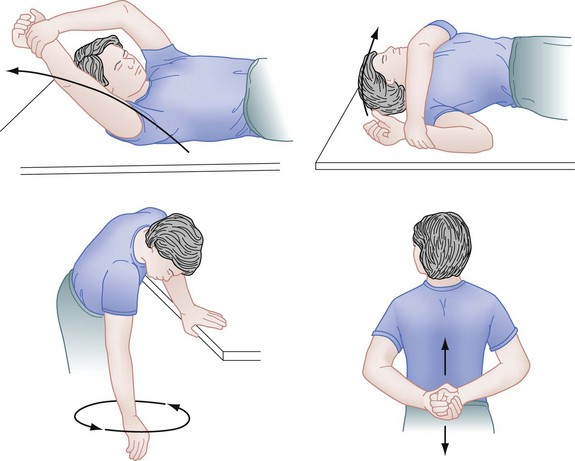
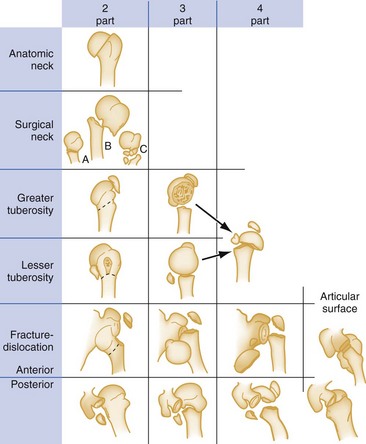
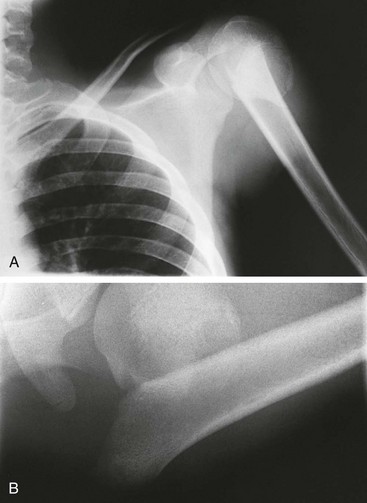
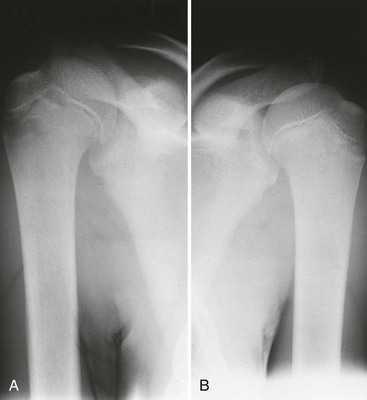
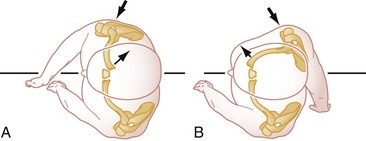
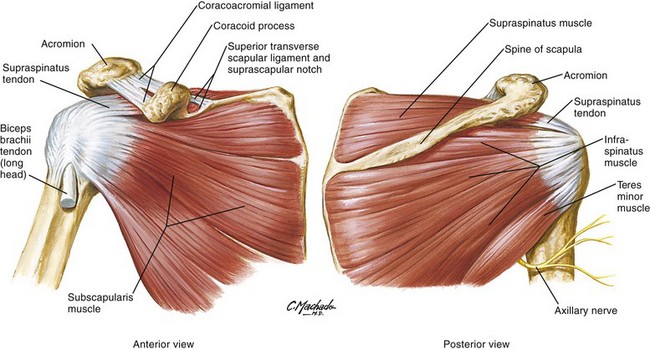
Chapter 53 The shoulder joint is a unique and complex articulation unit. It has the largest range of motion of any appendicular joint in the body and can be moved through a space that exceeds a hemisphere in extent. The nature of shoulder injuries has been long recognized: Wall paintings in Egyptian tombs from 3000 BCE show accurate drawings of manipulations (similar to the Kocher technique) used to reduce shoulder dislocations.1 Hippocrates outlined the oldest known method for reduction of shoulder dislocations.2 Shoulder injuries are commonly encountered in emergency medicine. Statistical studies show that 8 to 13% of all athletic injuries involve the shoulder and that shoulder dislocations account for more than 50% of all major joint dislocations seen in the emergency department (ED). Almost every major sport or athletic activity involves use of the shoulder joint in one way or another. The shoulder can be injured by trauma (indirect or direct) or by overuse. Traumatic injuries tend to occur in contact sports such as football and ice hockey, whereas overuse injuries (impingement syndromes) are more common in swimming and baseball. Shoulder injuries also are common in wrestling, tennis, volleyball, and javelin throwing.3 In general, children are vulnerable to the same injuries as those incurred by adults; however, the presence of the epiphysis and its growth plate changes the pattern of injuries.4 The strength of the joint capsule and its ligaments is two to five times greater than that of the epiphyseal plate. An injury that produces a sprain or dislocation in an adult often causes a fracture through the hypertrophic zone of the growth plate in a child. The shoulder girdle has epiphyseal plates at the acromion process, proximal humeral head, coracoid process, glenoid cavity, and medial end of the clavicle. Complete or greenstick fractures of the clavicle and fractures of the proximal humeral epiphysis are encountered more commonly in the pediatric population. Most shoulder injuries in children can be treated conservatively, with a good prognosis for full return of function.4 The shoulder girdle connects the upper extremity to the axial skeleton (Fig. 53-1). It consists of three bones, the clavicle, humerus, and scapula; three joints, the acromioclavicular, glenohumeral, and sternoclavicular joints; and one pseudoarticulation, the scapulothoracic pseudoarticulation. The sternoclavicular joint (SCJ) represents the only true articulation between the upper extremity and the axial skeleton (Fig. 53-2). Stabilizers of this diarthrodial joint include the anterior and posterior sternoclavicular ligaments, the interclavicular ligament, and the costoclavicular ligament. The costoclavicular ligament opposes the pull of the sternocleidomastoid and is considered the most important stabilizing ligament.5 The SCJ participates in all movements of the upper extremity and is the most moved joint in the body. The superior mediastinum with its great vessels, trachea, esophagus, thoracic duct, lung apices, and other important structures is immediately posterior to the joint. The clavicle is an S-shaped bone that acts as a strut to support the upper extremity and keep it away from the chest wall. It articulates medially with the sternum and laterally with the acromion process. The clavicle provides the neck with an acceptable cosmetic appearance and protects the subclavian vessels and brachial plexus. Its middle third, which is thin and untethered, is the most commonly fractured segment.6 The acromioclavicular joint (ACJ) connects the lateral end of the clavicle with the medial aspect of the acromion process (Fig. 53-3). The diarthrodial ACJ has little or no bony stability and is dependent on the associated ligaments and muscles for support.7 The weak acromioclavicular ligaments provide posterior support while the clavicular and acromial attachments of the deltoid and trapezius muscles provide static and dynamic support for the superior aspect of the joint. The most important stabilizers are the coracoclavicular ligaments (conoid and trapezoid), which provide vertical and anterior support. The scapula is a flat triangular bone that forms the posterior aspect of the shoulder girdle. The thin body of the scapula lies flat against the posterior thorax and widens laterally to form the glenoid fossa. The scapula’s thickened borders are the attachment sites for 18 muscle origins and insertions.8 The thick muscle coat and ability to recoil along the posterior chest wall protect the scapula from both direct and indirect trauma. A synovial membrane extends from the glenoid fossa to the humeral head. The membrane is large and redundant inferiorly to accommodate the extensive range of movement. Overlying the synovial membrane is a loose and redundant fibrous capsule. Anteriorly, the capsule is thickened to form the superior, middle, and inferior glenohumeral ligaments. The anterior band of the inferior glenohumeral ligament is the most important restraint to anterior glenohumeral dislocations.9 The glenohumeral articulation is a ball-and-socket–type joint that depends largely on associated capsule, muscles, and ligaments for stability (Fig. 53-4). A negative intracapsular pressure completes the stabilization mechanism.9,10 The absence of bony stability permits a range of motion, however, that is greater than that of any other joint in the body. The proximal humerus articulates with the glenoid fossa and provides for the attachment of many important muscles. The supraspinatus, infraspinatus, and teres minor insert onto facets of the greater tuberosity, whereas the subscapularis inserts onto the lesser tuberosity. Together, this group of muscles forms the rotator cuff, which helps stabilize the humeral head within the glenohumeral joint (Fig. 53-5). The long head of the biceps tendon originates from the supraglenoid tubercle and ascends over the humeral head to enter the arm via the bicipital groove. The long head acts as an additional stabilizer for the superior and anterior aspects of the glenohumeral joint (see Fig. 53-5). Long muscles that cross the articulation are involved primarily in movements of the glenohumeral joint. The pectoralis major, latissimus dorsi, and teres major muscles all insert into the humeral intertubercular groove. Displacements encountered with fractures of the humerus usually reflect the pull of these attached muscle groups. The proximal humerus is composed primarily of trabecular bone with a thin cortical shell. Changes in bone density with age (osteoporosis) greatly increase the risk of fractures in this area.6 Figure 53-5 The rotator cuff: anterior view, posterior view, and the four muscles—subscapularis, supraspinatus, infraspinatus, teres minor. (Netter illustration from www.netterimages.com. Copyright Elsevier Inc. All rights reserved.) The examination is completed with an assessment of the neurovascular function. A complete sensory (light touch and pinprick) and full motor examination of the brachial plexus should be performed. This examination is best performed by assessing the myotomes and dermatomes (Table 53-1) pertinent to each nerve root within the brachial plexus. The radial pulse should also be checked, although collateral circulation may preserve this in the presence of a vascular injury. The presence of pallor, paresthesias, or an expanding hematoma should raise suspicion for a vascular injury. The neurovascular examination should be repeated after any manipulation in the ED, and the findings recorded. Table 53-1 Sensory and Motor Components of the Brachial Plexus The initial assessment of traumatic injuries includes a three-view series of radiographs consisting of true anteroposterior (AP) (45-degree lateral), transscapular lateral (“Y” view), and axillary lateral views (Figs. 53-6 and 53-7). The true AP view (see Fig. 53-7B) is preferred over standard AP views because it shows the glenohumeral joint without any bony overlap. Standard AP views taken with the joint in internal and external rotation profile the lesser and greater tuberosity and are more useful in the evaluation of soft tissue conditions. Acceptable orthogonal views include the axillary lateral, transscapular lateral, and apical oblique.11 The preferred view is the axillary lateral (see Fig. 53-7A), which projects the glenohumeral joint in a cephalocaudal plane. This view is particularly useful for defining the relationship of the humeral head with the glenoid fossa and in identifying lesions of the coracoid process, humeral head, and glenoid rim. Some degree of abduction is required for the axillary view, and patient cooperation with this position may be limited by pain. The difficulty in obtaining this view has led to the popularity of the transscapular view (see Fig. 53-7B). Advantages of this projection include its simplicity and reproducibility and a clear delineation of anatomic structures. In this view the scapula is projected as a Y, with the body forming the lower limb and the coracoid and acromion processes forming the upper limbs. The humeral head normally is superimposed over the glenoid, which is located at the junction of the three limbs. This view is particularly useful in identifying anterior and posterior glenohumeral dislocations. The apical oblique view (obtained by having the patient stand bending forward, and angling the central ray 45 degrees caudally) shows the glenohumeral joint in a unique coronal projection. This view can be obtained easily and painlessly and has been found to be useful in evaluating for Hill-Sachs lesions in shoulder dislocations, and displacement and angulation of proximal humerus fractures.11 Plain radiographs are the mainstay of the radiologic examination in the ED, but in selected circumstances, additional bone and soft tissue details may be obtained via computed tomography (CT) or magnetic resonance imaging (MRI). Bedside ultrasonography is emerging as a reliable screening and diagnostic imaging modality for selected injuries, in particular fractures of the clavicle.5,12 Pathophysiology.: The clavicle accounts for 5% of all fractures and is the most commonly fractured bone in children. Epidemiologic studies in adults have documented an annual incidence rate of 29 to 64 per 100,000 population, with a 2 : 1 male-to-female ratio.13 Clavicular fractures are classified anatomically and mechanistically into three groups. Fractures of the medial third are uncommon (5%) and occur as a result of a direct blow to the anterior chest. Fractures of the middle third are the most frequent (Fig. 53-8), accounting for 80% of all injuries. The usual mechanism of injury involves a direct force applied to the lateral aspect of the shoulder as a result of a fall, sporting injury, or motor vehicle collision (MVC). Fractures of the lateral third (15%) result from a direct blow to the top of the shoulder and are classified further into three subtypes.13 Type I fractures are stable and minimally displaced because the coracoclavicular ligament remains intact. Type II fractures are associated with a torn coracoclavicular ligament and have a tendency to displace because the proximal fragment lacks any stabilizing forces. Type III injuries involve the articular surface (Fig. 53-9). Clinical Features.: The patient has pain over the fracture site, and the affected extremity is held close to the body. With fractures of the middle third, the shoulder typically is slumped downward, forward, and inward. This positioning is a result of the effect of gravity and the pull of the pectoralis major and latissimus dorsi on the distal fragment. The proximal fragment often is displaced upward by the action of the sternocleidomastoid. The head is often tilted toward the injured side in an attempt to relax the effects of these displacing muscular forces. Ecchymosis, crepitus, and a palpable or visible deformity may be noted over the fracture site. Examine thoroughly for any tenting of the skin, as this can cause pressure necrosis and progression to an open fracture. Although associated neurovascular injury is rare, the close proximity of the subclavian vessels and brachial plexus demands a thorough assessment. Associated pneumothorax and pulmonary injuries are also rare unless an open or medial third fracture is present.14 Clavicle-specific plain radiographs should be obtained to confirm the presence of a fracture.12 The newborn clavicle fracture sustained during birth classically manifests as an uneventful “lump,” representing the area of subsequent callus formation, in a child brought in by a concerned parent. Fractures in children, especially neonates, can also be reliably diagnosed or ruled out by bedside ultrasound, sparing the infant exposure to radiation (Fig. 53-10). Management.: Principles of initial management include pain control, immobilization, and proper follow-up care. Fractures of the clavicle can be immobilized with supportive devices, such as a simple sling or sling and swathe (Fig. 53-11). Another immobilization technique for midclavicular fractures still recommended in the orthopedic literature, although its efficacy is not supported by evidence, is the clavicular (figure-of-eight) splint (Fig. 53-12). This splint is applied after closed reduction of the fracture, which is accomplished by pulling the shoulders up and back. Such reductions are difficult to maintain and may be associated with increased discomfort at the fracture site. Use of clavicular splints also can lead to skin irritation and compression of the neurovascular bundle in the axilla. Because some degrees of malunion and shortening are associated with an acceptable functional and cosmetic outcome, treatment with a simple sling is a valid and appropriate alternative to the clavicular splint in the ED. Disposition.: Immediate orthopedic consultation should be sought for open fractures or fractures associated with neurovascular injuries, skin tenting, or interposition of soft tissues. More urgent orthopedic consultation (before 72 hours) is recommended for type II lateral clavicle fractures because these fractures have up to a 30% incidence of nonunion and may require surgical repair.13 Severely comminuted or displaced fractures of the middle third (defined as over 20 mm of initial shortening) may also benefit from early orthopedic referral for consideration of operative reduction, because these have been associated with a higher incidence of nonunion and long-term functional deficits.14,15 Additional risk factors that have been associated with nonunion in midclavicular fractures include female gender and advancing age.16 Greenstick fractures of the midclavicle are common in children (Fig. 53-13). Most of these fractures are nondisplaced and heal uneventfully. Initial radiographs may appear normal despite suggestive clinical findings. In these instances, the arm should be immobilized in a simple sling and the radiographic evaluation repeated in 7 to 10 days if pain persists, to evaluate for early callus formation. Most fractures of the clavicle heal uneventfully, and follow-up can be provided by a primary care physician. A sling should be worn until repeat radiographs show callus formation and healing across the fracture site. Early passive shoulder range-of-motion exercises (Fig. 53-14) are encouraged to reduce the risk of adhesive capsulitis (so-called “frozen shoulder”). Younger children generally require shorter periods of immobilization (2 to 4 weeks) than adolescents and adults (4 to 8 weeks). Vigorous competitive play should be avoided until the bone healing is solid. Full range of motion of the shoulder and an absence of pain are two good clinical signs that the fracture has healed. Complications.: The most common complications are delayed union, nonunion, and symptomatic malunion.13,17 Displaced fractures of the middle third have a 15 to 20% rate of nonunion and up to 25% rate of symptomatic malunion.15 Vascular complications after fractures of the medial third can resemble those associated with posterior sternoclavicular dislocations. Articular surface injuries (type III lateral clavicle fractures) can lead to subsequent osteoarthritis of the ACJ. An uncommon but important association is that between clavicle fractures and atlantoaxial rotatory displacement (AARD). Most cases occur in girls younger than 10 years. The pathophysiology may involve a lax or disrupted alar ligament along with sternocleidomastoid spasm. Early diagnosis is important because delayed diagnosis can lead to a chronic deformity requiring surgical correction. AARD should be suspected if the child has a clavicle fracture and demonstrates a “cocked-robin” position with the head bent toward the fractured side but rotated in the opposite direction. The injury is best demonstrated by CT and, if recognized early, can be treated with a soft cervical collar or halo traction.18 Pathophysiology.: Fractures of the scapula are rare, with an annual incidence of 10 to 12 per 100,000 population.19 They account for 1% of all fractures and occur primarily in men 30 to 40 years old.8 In general, considerable force and energy are required to fracture the body and neck of the scapula. Common mechanisms of injury include high-speed MVCs and falls from height.20 Coracoid process fractures are usually avulsive, and glenoid rim fractures are commonly associated with anterior glenohumeral dislocations. Acromial or spinous process fractures result from blunt trauma to the top of the shoulder.21 The most important aspect of scapular fractures is the high incidence (75-98%) of associated injuries to the ipsilateral lung, chest wall, and shoulder girdle complex.8,20 The most common associated orthopedic injuries are fractures of the ribs, proximal humerus, and clavicle. Associated lung injuries, including pneumothorax, hemothorax, and pulmonary contusion, usually occur acutely but may manifest in delayed fashion, 2 to 3 days after the initial injury. Associated injuries of the head, spinal cord, brachial plexus, and subclavian or axillary vessels are more significant but less common.8,20 Of note, in a large series of blunt trauma admissions, the prevalence of aortic injury was similar in patients with or without a fractured scapula.20 Fractures of the scapula have traditionally been classified according to their anatomic location. Fractures can involve the acromion process, scapular spine, or coracoid process. Fractures can also involve the scapular neck (Fig. 53-15), glenoid fossa (intra-articular), and scapula body. Recently the Orthopaedic Trauma Association proposed a more comprehensive classification system that allows for a better understanding of severity and prognosis associated with these fractures. Fractures are divided into two main types: extra-articular and intra-articular (with partial or total glenoid involvement).22 Clinical Features.: In a conscious patient, the shoulder is adducted and the arm is held close to the body. Any attempts at movement result in significant pain. Associated tenderness, crepitus, or hematoma may be noted over the fracture site. The clinical findings occasionally mimic those with a rotator cuff tear. Hemorrhage into the rotator cuff associated with the scapula fracture can result in spasm and a temporary reflex inhibition of function (pseudorupture).21 The presence of a scapula fracture should prompt a thorough search for associated thoracic, intracranial, orthopedic, and neurovascular injuries. Diagnostic Strategies: Radiology.: The three-view trauma shoulder series will reveal most scapular fractures, as will careful examination of the scapula on the trauma chest radiograph. The true AP view best evaluates the glenohumeral joint, glenoid neck, and scapular body. The transscapular lateral view may demonstrate displacement of the glenoid and scapular body. The axillary lateral view is especially useful in evaluating fractures of the glenoid fossa and the acromion or coracoid process.8,21 An os acromiale (unfused acromial process epiphysis) is present in 3% of the population and should not be confused with a fracture of the acromion.6 A comparison film can be useful because the abnormality is present bilaterally in 60% of cases. In many patients, fractures of the scapula initially are overlooked despite being readily apparent on the initial supine trauma chest radiograph because of the life-threatening nature of the associated injuries.8 Although additional dedicated scapula views can be obtained in the ED, the presence as well as the extent of scapular injury is best determined by CT. In the event that a trauma chest CT scan has been obtained to search for associated injuries, a three-dimensional reconstruction of the scapula should be requested to further define the nature and extent of the injury.21,23 Management.: Most fractures, including fractures with severe comminution and displacement, heal rapidly with conservative therapy.8,22 Initial therapy consists of analgesia and immobilization in a sling to support the ipsilateral upper extremity. Passive (see Fig. 53-14) followed by active range-of-motion shoulder exercises should be initiated as soon as discomfort subsides, to reduce the risk of adhesive capsulitis. Most patients require a sling for 2 to 4 weeks and close radiographic follow-up for assessment for delayed displacement.21 Fractures of the body and spine usually require no further therapy. Nondisplaced fractures of the acromion process also respond well to conservative therapy. Displaced acromial fractures that impinge on the glenohumeral joint require surgical management. Rarely, the acromion is fractured as part of a superior dislocation of the humeral head. In these instances, an accompanying tear of the rotator cuff is invariably present and requires surgical repair. If the coracoclavicular ligaments remain intact, fractures of the coracoid process respond well to conservative therapy. Severely displaced coracoid fractures with ruptured coracoclavicular ligaments usually require open reduction and internal fixation. Scapular neck and glenoid fossa fractures present the most difficult management issues. Although most of these injuries also do well with conservative therapy, open reduction and internal fixation may be recommended for severely displaced or angulated fractures.21 In a review of 520 scapula fractures from 22 case series, Zlowodzki and co-workers reported that 80% of all fractures with glenoid involvement were treated operatively, whereas 83% of all neck injuries and 99% of all isolated scapula body fractures were treated nonoperatively.19 Complications.: Associated injuries of the ipsilateral lung, chest wall, and shoulder girdle account for most complications after fractures of the scapula. A shear-type brachial plexus injury has been associated with fractures of the acromion process. Neurovascular (brachial plexus, axillary artery) injuries also have been reported with fractures of the coracoid process, scapular neck, body, or spine fractures that extend into the suprascapular notch to injure the suprascapular nerve. The most common presenting symptom of a suprascapular nerve injury is dull posterior shoulder pain that is worsened by activity. The characteristic examination finding is atrophy of the scapular muscles along with weakness in abduction and external rotation Delayed complications include adhesive capsulitis and rotator cuff dysfunction. Pathophysiology.: Fractures of the proximal humerus are common and account for 4 to 5% of all fractures.24 An epidemiologic Swedish study reported an incidence of 14 to 60 per 100,000 per year, with a mean age at occurrence of 63 years and a female-to-male ratio of 1.5 : 1.25 These fractures occur primarily in the older population, in whom structural changes associated with aging (osteoporosis) weaken the proximal humerus, predisposing it to injury. Although most of these injuries involve minimal displacement and are adequately managed with conservative therapy, significantly displaced fractures may require operative intervention. Displacements encountered with fractures of the humerus usually reflect the pull of the attached muscle group. Fractures of the proximal humerus separate along old epiphyseal lines, producing four distinct segments consisting of the articular surface (anatomic neck), greater tuberosity, lesser tuberosity, and humeral shaft (surgical neck). Neer’s classification system (Fig. 53-16) is based on the relationship of these fracture fragments.24 In this system, a segment is considered displaced if it is angled more than 45 degrees or separated more than 1 cm from the neighboring segment. Because this classification system considers only displacement, the number of fracture lines is irrelevant. There are four major categories of fracture: minimal displacement (Fig. 53-17), two-part displacement (Fig. 53-18), three-part displacement, and four-part displacement. When present, anterior and posterior dislocations are included as part of the classification. Impaction and head-splitting fractures are classified separately. Figure 53-17 Three-part minimally displaced fracture of the proximal humerus involving the greater and lesser tuberosities. Clinical Features.: The affected arm is held close to the body, and movement is restricted by pain. Tenderness, hematoma, ecchymosis, deformity, or crepitus may be noted over the fracture site. A thorough neurovascular examination is essential to identify associated injuries of the axillary nerve, brachial plexus, or axillary artery (see Table 53-1). The three-view trauma series of shoulder radiographs will allow for assessment of the number of fracture fragments and degree of displacement or angulation. Management.: Minimally displaced fractures (see Fig. 53-17) constitute 80 to 85% of all cases. In these instances, limited displacement or angulation is present, and the fracture segments are held together by the capsule, periosteum, and surrounding muscles. Initial treatment consists of adequate analgesia and immobilization with a sling or sling and swathe device. The former is more comfortable, and a Cochrane review of 16 randomized trials found only limited evidence that use of special bandage immobilization affected time to fracture union or functional outcome.26 Traditionally, it has been recommended that immobilization be continued until clinical union is achieved (head and shaft are seen to move together). The Cochrane review also noted that immediate or earlier commencement of physiotherapy (within 1 week) resulted in less pain and did not compromise long-term outcome. Initial passive exercises (see Fig. 53-14) are gradually replaced by more active and resistive exercises. Most nondisplaced fractures heal over 4 to 6 weeks. The treatment of two-part, three-part, and four-part displaced fractures is beyond the scope of this discussion. An orthopedic surgeon should be consulted, because many of these injuries require operative repair.24 Prospective and retrospective observational studies, however, have failed to show a significant functional difference between operative and nonoperative treatment of displaced two-part and three-part fractures in elderly patients. Current literature continues to support operative treatment of four-part fractures in the elderly; the procedure of choice is hemiarthroplasty.26 Fracture-dislocation injuries (Fig. 53-19) are best managed in consultation with an orthopedic surgeon before attempts at reduction (except in cases of neurovascular compromise or unavailability of an orthopedic surgeon). Of note, reductions of these injuries in the ED often are unsuccessful, and these manipulations can cause separation of previously undisplaced segments. Closed reduction under radiologic control and general anesthesia may be preferable. Complications.: The most common complication of proximal humeral fractures is adhesive capsulitis. This complication can be prevented by the early initiation of pendular shoulder exercise, along with a thorough rehabilitation program. One of the most devastating complications is avascular necrosis (AVN) of the humeral head. The highest rate of AVN (up to 90%) has been documented for four-part fractures.27 Repeated forceful attempts at reduction of fracture-dislocations may be associated with subsequent heterotopic bone formation (myositis ossificans). Neurovascular injuries (axillary nerve, brachial plexus, and axillary artery) may be encountered with displaced surgical neck fractures and fracture-dislocations. Pathophysiology.: Fractures of the proximal humeral epiphysis are uncommon and account for less than 1% of all pediatric fractures.28 The injury can occur at any age while the epiphysis remains open but is most common in adolescent boys. The most common mechanism of injury involves a fall onto the outstretched hand, and the fracture typically occurs through the zone of hypertrophy in the epiphyseal plate. Injuries can be classified according to their location (Salter system), stability, and degree of displacement. Clinical Features.: The patient holds the injured arm tightly against the body by the opposite hand. The area over the proximal humerus is swollen and extremely tender to palpation. Radiographs obtained at 90 degrees to each other confirm the diagnosis. Comparison views may be helpful with minimally displaced fractures. Bedside ultrasound has also been shown to detect these injuries. In one series of 100 shoulder injury subjects, all three cases of proximal humerus fractures were detected by ultrasound imaging (sensitivity 83-93%) before shoulder radiographs had been obtained.12 Management.: Fractures of the proximal humeral epiphysis should not be taken lightly, because the physis accounts for 80% of the growth of the bone. The active healing process at the site of an epiphyseal injury makes delayed reduction extremely difficult. Early orthopedic consultation should be obtained for all such injuries. Children younger than 6 years usually have Salter I epiphyseal injuries (Fig. 53-20), which can be treated conservatively with sling and swathe immobilization and analgesic agents. Children older than 6 years usually have a Salter II epiphyseal injury. Salter II injuries with more than 20 degrees of angulation may benefit from reduction, which is accomplished by reversing the mechanism of injury.28 Imperfect reductions often are acceptable because growth and remodeling correct the deformity with time. After reduction, unstable injuries should be immobilized in a shoulder spica cast, whereas stable lesions can be immobilized with a sling and swathe. Fractures of the proximal humeral epiphyses generally heal in 3 to 5 weeks.28 Pathophysiology.: SCJ dislocations are infrequent and account for less than 1% of all dislocations.29 Significant forces are required to disrupt the strong ligamentous stabilizers of this joint. The most common causes are MVCs and injuries sustained in contact sports. The SCJ can dislocate in an anterior or a posterior direction. Anterior dislocations, which result from indirect forces, are more common (9 : 1 ratio).5 The usual mechanism of injury (Fig. 53-21) involves an anterolateral force to the shoulder, followed by backward rolling, which levers the medial clavicle out of its articulation. Posterior dislocations (Fig. 53-22) can result from a direct blow to the medial clavicle (30%) or from delivery of a posterolateral force to the shoulder, followed by inward rolling (70%). Posterior dislocations can be associated with life-threatening injuries within the superior mediastinum, including acute airway compression. Injuries to the SCJ can be graded into three types.5 A grade I injury is a mild sprain secondary to stretching of the sternoclavicular and costoclavicular ligaments. A grade II injury is associated with subluxation of the joint (anterior or posterior) secondary to rupture of the sternoclavicular ligament. The costoclavicular ligament remains intact. Complete rupture of the sternoclavicular and costoclavicular ligaments results in a grade III injury (dislocation). In patients younger than 25 years, these actually represent Salter type I injuries, because the medial epiphysis of the clavicle has not yet fused.30 Clinical Features.: Clinical suspicion is the most important factor in diagnosing these injuries, and prompt diagnosis is vital because it is associated with a better prognosis. The injured extremity is flexed at the elbow and supported across the trunk by the opposite arm. Pain results from any movement of the upper extremity or lateral compression of the shoulders. The SCJ may be mildly swollen and tender to palpation. With an anterior dislocation, the displaced medial end of the clavicle may be palpable. Posterior dislocations are associated with more severe pain, and the neck is often flexed toward the injured side.30 The clavicular notch of the sternum may be palpable, and complaints of hoarseness, dysphagia, dyspnea, and weakness or paresthesias in the upper extremities have been documented. Rarely, airway complications caused by tracheal injury may be present. If present, airway compromise should be attended to promptly. These patients should also be examined thoroughly to identify any injuries to superior mediastinal or intrathoracic structures. The presence of cyanosis and venous congestion of the neck and arm is typical of an innominate vein injury.30 When necessary, appropriate consultation should be obtained.
Shoulder
Perspective
Principles of Disease
Clinical Features
Physical Examination
SPINAL LEVEL
SENSORY AREA
MUSCLE
C2-4
—
Trapezius
C5
Lateral arm
Deltoid
C6
Lateral forearm and thumb
Biceps
C7
Tip of long finger
Thumb extensors
C8
Tip of little finger and medial forearm
Finger flexors
T1
Medial arm
Hand interossei
Diagnostic Strategies
Specific Injuries
Clavicle
Scapula
Proximal Humerus

Proximal Humeral Epiphysis
Dislocations

Full access? Get Clinical Tree


Shoulder
Only gold members can continue reading. Log In or Register to continue