Asthma*
Pneumonia
Bronchitis
Croup*
Bronchiolitis
Hyperventilation*
Pleuritis
Chronic obstructive pulmonary disease*
Congestive heart failure*
Myocardial ischemia or infarction
Spontaneous pneumothorax
Primary pulmonary hypertension
Pulmonary embolism*
Cardiac tamponade
Laryngeal or tracheal obstruction
Superior vena cava syndrome
Pneumocystis carinii pneumonia
Pleural effusion
Interstitial lung diseases
Endobronchial foreign bodies
Anxiety
Fever associated with dyspnea usually implies an infectious cause such as pneumonia, tracheobronchitis, or croup and bronchiolitis in children.
Cough productive of yellow-green sputum suggests an infectious bacterial cause, whereas clear sputum is more often seen in viral infection; pink, frothy sputum may be noted in patients with congestive heart failure (CHF).
A history of pedal edema, paroxysmal nocturnal dyspnea, or orthopnea suggests CHF. An associated history of hypertension, coronary artery disease, or both lends support to this diagnosis.
Anginal discomfort accompanying dyspnea implies that either acute left ventricular dysfunction has developed in the context of ongoing myocardial ischemia or hypoxemia produced by acute CHF (pulmonary edema) has led to myocardial ischemia.
Sudden onset of breathlessness in a patient with a history of smoking, calf swelling or tenderness, hypercoaguable state, immobilization for a prolonged period, pregnancy, or oral contraceptive use suggests pulmonary embolism (PE).
Pleuritis of any cause may be accompanied by the sudden onset of dyspnea and pleuritic chest pain.
Tall, thin, young men who report the sudden onset of breathlessness and pleuritic chest or back pain should be suspected to have had a spontaneous pneumothorax.
Shortness of breath remains a common presenting symptom in patients with anxiety-related hyperventilation, although this is a diagnosis of exclusion.
Patients with severe respiratory distress from any cause use their accessory muscles of respiration and often assume a tripod position on the stretcher. Children often display nasal flaring and suprasternal and intercostal retractions. A decrease in vigilance or development of somnolence is a sign of impending respiratory failure.
Fever may be noted in patients with breathlessness caused by an infectious cause.
A prolonged expiratory phase and wheezing are noted in patients with bronchospasm; however, in persons with severe airway obstruction, airflow may be so limited that wheezing is absent until therapy results in increased airflow.
Signs of lobar consolidation, including egophony, whisper pectoriloquy, and enhanced or absent breath sounds may be noted in patients with pneumonia or neoplastic disorders of the lung resulting in bronchial obstruction.
An increased jugular venous pulse, rales, an S gallop, hepatosplenomegaly, ascites, and pedal edema are all signs of CHF.
A loud P with a palpable pulmonary artery segment and a pronounced subxiphoid impulse are noted in patients with pulmonary hypertension, as are often other signs of right-sided heart failure.
Cardiac tamponade may result in distant heart sounds, tachycardia, hypotension, and dyspnea in the setting of a relatively normal lung examination.
Dry, “Velcro-like” rales are often noted in patients with interstitial lung disease.
Pleural effusions produce dullness to percussion at the lung bases and may be found in the setting of CHF, pneumonia, or neoplastic disease.
Stridor is noted in patients with obstructing lesions of the upper airway, with endotracheal or endobronchial foreign bodies, or, especially in young children, as a consequence of epiglottitis or croup.
All patients with a complaint of shortness of breath must have a complete set of vital signs including temperature and pulse oximetry.
The chest roentgenogram may reveal an infiltrate, pulmonary vascular congestion or pneumothorax.
In patients suspected of pneumothorax, an upright, end-expiratory, posterioranterior film is most sensitive and should specifically be requested when this diagnosis is suspected.
Radiologically, patients with CHF typically manifest cardiomegaly, often in association with bilateral alveolar infiltrates, pulmonary vascular redistribution, perihilar prominence, and peribronchial cuffing.
A complete blood count (CBC) with differential may be helpful in assessing the presence of infection and may suggest a bacterial or viral etiology in some patients.
Brain natriuretic peptide (BNP) is useful in identifying patients with elevated left ventricular filling pressures due to CHF. BNP is elevated early in patients with cardiac dysfunction and in symptomatic patients; a normal level should cause one to reconsider a cardiac etiology for breathlessness (Table 21-1).
A lateral neck radiograph is also helpful in the differential diagnosis of stridor or upper airway obstruction. An edematous, enlarged epiglottis is noted on the lateral projection in patients with epiglottitis, while a narrowed tracheal air column is seen on the anterior-posterior (AP) projection in patients with croup. A foreign body may also be noted.
Direct fiberoptic larygoscopy may reveal an enlarged, erythematous epiglottis that is diagnostic for epiglottitis or may demonstrate an obstructing foreign body.
Spiral chest CT or ventilation/perfusion scanning can be used to confirm the diagnosis of PE.
Table 21-1 Median BNP Levels Among Patients in Each of the Four Heart Failure Classesa
Class
Patient Symptoms
BNP Level (pg/mL)
Class I (mild)
No limitation of physical activity. Ordinary physical activity does not cause undue fatigue, palpitation, or dyspnea.
244 (±286)
Class II (mild)
Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in fatigue, palpitation, or dyspnea.
389 (±374)
Class III (moderate)
Marked limitation of physical activity. Comfortable at rest, but less than ordinary activity causes fatigue, palpitation, or dyspnea.
640 (±447)
Class IV (severe)
Unable to perform any physical activity without discomfort. Symptoms of cardiac insufficiency at rest. If any physical activity is undertaken, discomfort is increased.
817 (±435)
aData from in Maisel AS, Krishnaswamy P, Nowak RM, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 2002;347(3):161-167.
Arterial and venous blood gases have limited utility. Pulse oximetry and clinical respiratory status should guide most management decisions. Blood gases may reveal hypoventilation and CO2 retention. A normal or rising pCO2 may indicate impending respiratory failure.
All patients with a complaint of shortness of breath must have a complete set of vital signs including temperature and pulse oximetry.
A normal oxygenation level on pulse oximetry or ABG does not exclude pulmonary embolus.
A chest roentgenogram is indicated in most patients with a complaint of shortness of breath. Asthmatics with a nonfocal lung exam may not require a chest roentgenogram.
Patients with an acute asthmatic attack complain of shortness of breath, cough, and, occasionally, audible wheezing. Symptoms may progress over a period of minutes to hours.
Those patients with a long history of asthma often attempt to medicate themselves with bronchodilators at home and appear in the ED when these measures fail.
Patients may have a history of upper respiratory tract infection or may report a cough, occasionally productive, that appears to exacerbate the sensation of dyspnea and wheezing.
In some patients with asthma, cold air or exercise often induces either cough alone as an early manifestation of bronchospasm or frank wheezing.
Patients experiencing an acute asthmatic attack appear quite anxious and dyspneic. Respiratory rate is increased and tachycardia with an elevated blood pressure is often noted.
In patients with severe bronchospasm, the accessory muscles of respiration are utilized, producing tracheal “tugging” and suprasternal and intercostal retractions.
Auscultation of the chest reveals a prolonged expiratory phase with associated inspiratory and expiratory wheezes; fine basilar rales may be heard in some patients, and in others, simple prolongation of the expiratory phase in the absence of wheezing is noted.
The heart sounds are distant as a result of air trapping and an increased thoracic diameter.
If severe hypoxemia evolves, nail bed and perioral cyanosis may develop.
Arterial blood gases should be deferred unless hypercarbia or serious hypoxemia is suspected and patients are unable to perform pulmonary function testing, particularly if symptoms are worsening despite treatment, and intubation and mechanical ventilation are being contemplated.
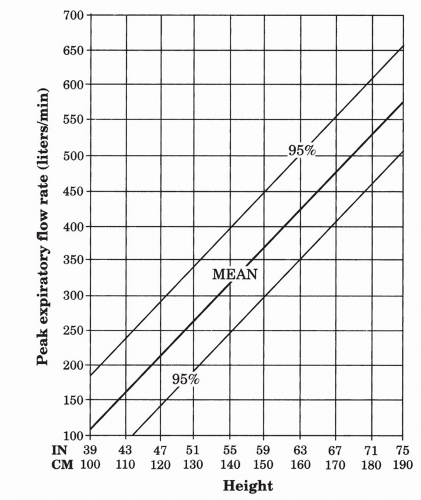
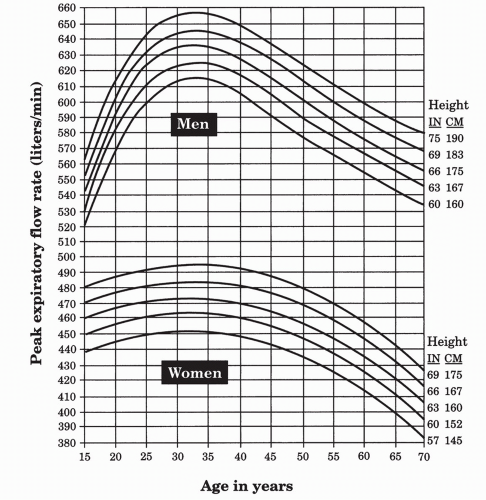
If possible, all patients should have a forced expiratory volume in 1 second (FEV1) or peak expiratory flow rate (PEFR) determined; these indices are helpful to determine attack severity and treatment strategy, the patient’s response to therapy, and admission/discharge decisions (Figs. 21-1 and 21-2).
If arterial blood gases are obtained, a low PCO2 due to hyperventilation is expected. A normal PCO2, suggesting significant obstruction, is worrisome. Elevation of the PCO2 occurs only with severe attacks and may indicate impending respiratory failure.
Patients using an oral theophylline preparation should have a baseline level obtained.
A CBC can be obtained (preferably before systemic steroids or epinephrine administration) if pneumonia is suspected.
A chest x-ray is necessary only to exclude pneumothorax or confirm a high clinical suspicion of pneumonia, or when patients fail to respond to therapy. An admission chest x-ray in the absence of the aforementioned indications is not indicated.
In patients who appear ill, supplemental oxygen should be immediately administered and continuous pulse oximetry initiated. Oxygen saturation measured by pulse oximetry correlates well with hypoxemia; saturations less than 90% indicate relatively serious hypoxemia (PaO2 < 60 mm Hg).
Inhalation of β-agonists is the primary treatment for the patient with acute asthma. Although delivery by metered-dose inhaler (MDI) is more efficient, most patients are treated via wet nebulization. Albuterol, 2.5 mg, via wet nebulization repeated three times, at 20-minute intervals, is a reasonable first-line intervention.
In patients with severe disease, administration of albuterol via continuous wet nebulization in increased doses (15 mg/h × 2 hours) with a large reservoir may be beneficial.
After stabilization, the frequency of inhalations is reduced to hourly, or every other hour, or ever 4 hours, depending on the particular patient.
An inhaled anticholinergic agent, such as ipratropium, 2.5 to 5.0 mg, is recommended. Ipratropium can be administered concurrently with albuterol and can be given at 20-minute intervals with each of the three initial inhalation treatments.
There is evidence that albuterol and ipratropium when administered in this manner produce more bronchodilation than treatment with albuterol alone.
Subcutaneous terbutaline (0.25 mg; may repeat in 20-30 minutes if needed), for those unable to comply with nebulization, produces a therapeutic response comparable to inhalation therapy with albuterol. Tachycardia often limits its use.
The early and aggressive use of corticosteroids in acute asthma is recommended; commonly used initial doses are methylprednisolone, 60 to 125 mg intravenous, or prednisone, 60 mg orally. A therapeutic response can be documented within 3 hours of administration with peak effects at approximately 6 to 10 hours.
The early use of steroids in the ED has been shown to reduce the number of patients requiring hospital admission.
There is no evidence that parenteral administration is superior to the oral route.
It is generally recommended that the following patients receive an initial dose of steroids in the ED: those who experience an acute attack while on, or tapering off, a steroid course; those with moderate (FEV1/PEFR 40% to 60% of predicted) or severe (FEV1/PEFR < 40% of predicted) attacks; and those with increasing frequent or accelerating attacks.
Patients who appear to be dehydrated should receive intravenous fluids in the ED; routine rehydration of patients with asthma is not indicated.
Acute episodes of asthma may be triggered by bacterial infection. When a reasonable degree of clinical suspicion exists in favor of bacterial infection, a course of antibacterial therapy is warranted.
Aminophylline is not particularly helpful in the initial management of asthma in the ED, but patients who are maintained on an oral aminophylline preparation should have a baseline blood level obtained and optimized.
Although the bronchodilatory properties of magnesium sulfate are well known, the role of magnesium in the treatment of acute asthma is not well defined. The use of magnesium is best reserved for severely ill patients who have not responded to other modalities and in whom intubation and mechanical ventilation appear increasingly likely. In these patients, 2 g of magnesium sulfate can be given intravenously. Side effects include nausea and vomiting, flushing, diaphoresis, weakness, hypotension, and respiratory depression; these are dose related and fortunately relatively uncommon.
The treatment of acute asthma in children is similar to the treatment of adults.
The treatment of the pregnant patient presenting with an acute asthmatic attack is essentially as outlined. Terbutaline, because of its inhibitory effect on uterine muscle contraction, is best avoided.