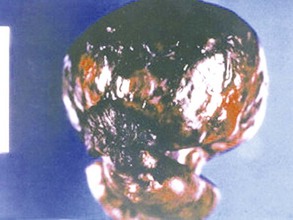
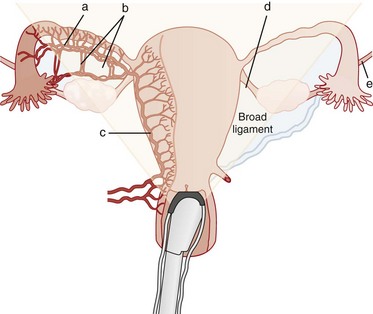
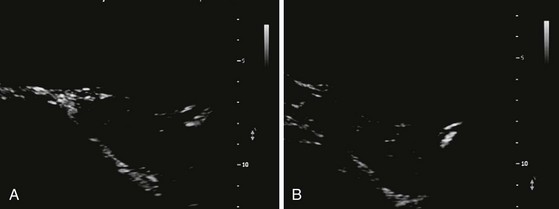
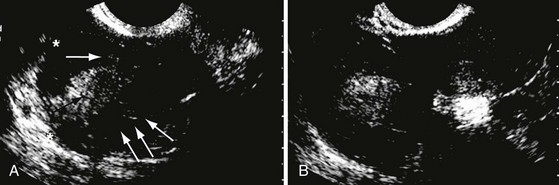
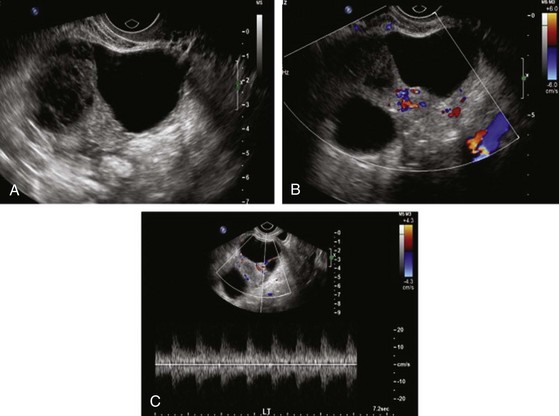
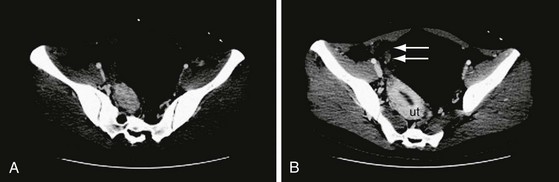
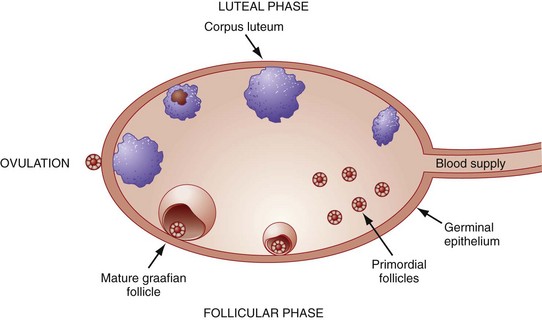
Chapter 100 Ovarian torsion accounts for approximately 3% of gynecologic emergencies.1 While ovarian torsion can occur in young girls2 and is increasingly recognized in postmenopausal women, it is still most common in the reproductive years because of the regular development of a corpus luteal cyst during the menstrual cycle.3 Ovarian torsion is typically caused by a twisting of both the ovary and the fallopian tube on the vascular pedicle.4 Most cases of torsion (50-80%) are associated with an ovarian tumor, typically a benign neoplasm; with large, heavy cysts, as seen in ovarian hyperstimulation syndrome after in vitro fertilization; or with polycystic ovaries.1 Torsion may be a complication of pregnancy.5,6 Torsion of a normal ovary only rarely occurs.7 A slight predominance of ovarian torsion on the right side has been noted. The reason for this predilection is unclear but may relate to the stabilizing effect of the sigmoid colon on the left side.4 In ovarian torsion, venous and lymphatic obstruction occurs initially, with subsequent congestion and edema of the ovary, progressing to ischemia and necrosis and eventual infarction of the ovary1 (Fig. 100-1). Thrombosis of the ovarian vein and artery can occur as well. The ovary is often salvageable if the diagnosis is made before thrombosis occurs.4 Because of the dual blood supply of the ovary from both the uterine and ovarian arteries, complete arterial obstruction is rare7 (Fig. 100-2). Ovarian torsion can often be challenging to diagnose, because the classic symptoms of severe, sharp unilateral abdominal pain and nausea may not be present.5,6,8,9 The presence of known risk factors for ovarian torsion such as an ovarian mass or infertility treatments may suggest the diagnosis.1 Because the presentation can be variable and often subtle, the diagnosis can be difficult to make. In 87 patients with surgically confirmed torsion, the diagnosis was missed on the first visit in almost half of the patients. Patients reported pain from several hours to weeks in duration, most likely from intermittent ischemia, and almost all had some pain on abdominal palpation. Nausea was a symptom in many of the patients. Other series report similar findings.2–4,6,8 No specific laboratory tests are helpful in the evaluation of a patient for suspected ovarian torsion, except for a pregnancy test to exclude ectopic pregnancy. A small percentage of patients may have an elevated white blood cell count above 15,000/µL,5 but this is not a reliable indicator of ovarian torsion.5,8 Ultrasonography.: Ultrasound examination is the initial imaging test in the evaluation of patients with pelvic pain suggestive of ovarian torsion.7 Enlargement of the ovary is the most common ultrasound finding,4 but the ovary also may have an abnormal position relative to the uterus. Enlargement of an ovary with a heterogeneous stroma and small, peripherally displaced follicles is the classic ultrasound appearance of torsion but is often absent, particularly early in the presentation4 (Fig. 100-3). The ultrasound study may reveal a mass in the ovary or evidence of hemorrhage10 (Fig. 100-4). The ultrasound appearance of ischemia can vary depending on the duration of the symptoms.11 Free pelvic fluid also may be seen.7 Hemorrhagic cysts and non-neoplastic masses frequently are associated with torsion. These may have a fluid-filled cystic component, exhibit a complex pattern with debris and septations, or be visualized as a solid mass.10 The characteristic appearance of torsion may be difficult to appreciate if the ovary is obscured by an associated mass.7 Doppler Ultrasound Examination.: Doppler ultrasound findings are inconsistent in ovarian torsion.7,12,13 Many cases of surgically proven torsion will have documented blood flow on Doppler examination because the ovary has a dual blood supply from both the ovarian and uterine arteries. Because the torsion may be intermittent, the findings may also vary depending on the time of the examination.7 If a large mass is present, the examination may be technically difficult to perform.9 Despite these limitations, the Doppler examination is still useful because detection of abnormal venous flow is particularly important in early cases of torsion10 (Fig. 100-5). Visualization of the twisting of the pedicle and the coiled vessels is referred to as a “whirlpool sign.”14,15 Lee and colleagues report an 88% accuracy for torsion when the twisted pedicle or whirlpool sign is visualized.16 In summary, the combination of ultrasound with Doppler studies is the initial study of choice in considering the diagnosis of ovarian torsion; however, it is important for the clinician to appreciate that many of the findings can be subtle and may be negative, particularly in early presentations. Computed Tomography.: When renal colic and appendicitis also are strong considerations in the differential diagnosis for acute pelvic pain, abdominopelvic computed tomography (CT) may be the best initial study, particularly in patients who have a presentation atypical for torsion.17 In ovarian torsion, CT findings include fallopian tube thickening, smooth wall thickening of the associated adnexal mass, ascites, and uterine deviation to the twisted side18,19 (Fig. 100-6). Associated hemorrhage in patients with hemorrhagic infarction can be seen. A retrospective review of CT scans of patients with confirmed torsion found that every CT scan had evidence of an abnormality, including ovarian enlargement or the presence of a mass or cyst, suggesting that torsion is unlikely if the CT visualized a normal ovary.20 In contrast, another study of surgically confirmed ovarian torsion cases found that CT correctly diagnosed 5 of 13 cases (38%), as opposed to ultrasonography, which correctly identified 15 of 21 cases (71%).3 Therefore, negative imaging findings should be interpreted with caution when clinical suspicion is high, but with lower suspicion a normal-appearing ovary on CT scan can be reassuring. Magnetic Resonance Imaging.: Magnetic resonance imaging (MRI) is not typically ordered in the ED but may also demonstrate findings consistent with torsion. It is particularly helpful if the diagnosis is not clear, such as with intermittent pain over days, or when the history is highly suggestive but the ultrasound is not conclusive.21 Findings on MRI suggestive of torsion are similar to those on CT.18 Box 100-1 lists the common imaging findings in ovarian torsion. Laparoscopy.: A diagnostic laparoscopy is the gold standard investigative modality in patients in whom clinical suspicion is high despite negative imaging results. In 100 nonpregnant patients with an acute abdomen, only 29 of the 66 laparoscopically proven cases of ovarian torsion were diagnosed preoperatively. Laparoscopy also allowed diagnosis of other unsuspected conditions, including ovarian cysts, appendicitis, and pelvic inflammatory disease.22 Once the diagnosis of ovarian torsion has been made, the patient should be taken to the operating room as soon as possible. Pediatric patients taken to surgery more than 24 hours later have been found to have a zero salvage rate, compared with patients who had the best chance for salvage—those who were taken to the operating room within 8 hours.23 The ovary often will recover even if black in appearance at the time of surgery because of its dual blood supply, so attempts at ovarian salvage are warranted even if the diagnosis is made late.24 This is particularly true in adolescent patients. Ovarian function returns in a majority of patients with surgery that saves the ovary.23 Additional imaging studies, such as MRI, are an option if the diagnosis is not clear. Because torsion of a normal-appearing ovary is very rare, patients with a normal-appearing ovary on CT or ultrasound scan may be discharged from the ED. Ovarian cysts are the most common cause of gynecologic masses. They occur at any stage of life but are most frequent in the reproductive years because of the cyclic changes of the ovary associated with menstruation (Fig. 100-7). Most ovarian cysts are benign and resolve with no interventions, but on occasion they may be malignant or associated with significant complications such as hemorrhage or torsion.
Selected Gynecologic Disorders
Ovarian Torsion
Clinical Features
Diagnostic Strategies
Imaging
Management
Ovarian Cysts and Masses

Full access? Get Clinical Tree


Anesthesia Key
Fastest Anesthesia & Intensive Care & Emergency Medicine Insight Engine