Chapter 45 Regional Anesthesia and the Difficult Airway
I Introduction
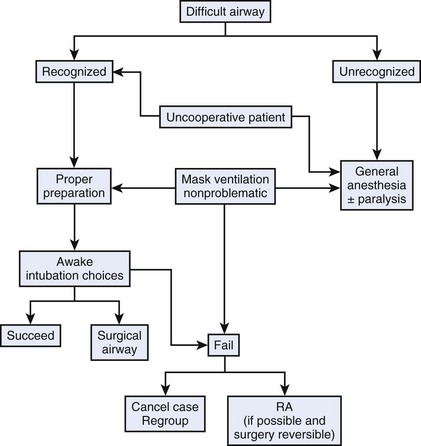
Regional anesthesia is recognized as an effective alternative to general anesthesia and is included in the American Society of Anesthesiologists (ASA) difficult airway algorithm as an alternative to failed intubation (Fig. 45-1).1 The anesthesiologist should carefully balance the risks and benefits of using regional anesthesia compared with those of securing the airway before the administration of anesthesia in a patient with an established difficult airway. The anesthesiologist has a responsibility to provide safe anesthetic care, including maintaining appropriate conditions to manage the airway effectively during the perioperative period. Morbidity and mortality as a consequence of mismanagement or lack of proper management of the airway represent major concerns for anesthesiologists worldwide.
II Practice Guidelines for Management of the Difficult Airway
Irrespective of the final decision, an appropriate assessment of the patient’s airway represents the first step. Although the ability to predict accurately a difficult airway preoperatively would be of great value, it is evident from the literature that no single airway assessment can reliably predict a difficult airway.2 Nevertheless, a preoperative airway history and physical examination should be performed in order to facilitate the choice and management of the difficult airway, as well as reduce the likelihood of adverse outcomes (see Chapter 9).3
Langeron and colleagues have established five factors that are frequently associated with difficult airway management.4 They separated difficult airway into difficult mask ventilation and difficult intubation; the former is the more deleterious of the two. It is well established that airway management may be more difficult in trauma cases and in patients with comorbidities, such as severe rheumatoid arthritis, morbid obesity, metabolic diseases, deformities, or pregnancy. Rocke and colleagues demonstrated that the incidence of difficult airway is 10 times higher during pregnancy than in the general population. They documented the potential risk factors for difficult airway in the obstetric patient.5 The risk factors included short neck, missing protruding incisors, receding mandible, facial edema, and high Mallampati scores. The relative risk of experiencing a difficult intubation compared with an uncomplicated class I airway assessment has been established as follows: class II, 3.23; class III, 7.58; class IV, 11.3; short neck, 5.01; receding mandible, 9.71; and protruding maxillary incisors, 8.0. Using the probability index or a combination of risk factors, or both, showed that for a combination of class III or IV plus protruding incisors, short neck, or receding mandible, the probability of difficult laryngoscopy was more than 90%.
The concept of a difficult airway has different meanings for different physicians. Although most anesthesiologists agree that a patient with very limited mouth opening, Mallampati IV classification, and a very short neck has a difficult airway, there is more controversy about the relative difficulty of managing the airway in a patient with cervical trauma or obesity. This in part reflects the increased expertise in airway management of anesthesiologists and the increased number of airway devices designed to facilitate airway management. For example, Hagberg and colleagues demonstrated that Cormack-Lehane grade 3 airways assessed by laryngoscopy were reduced to grade 2 and even grade 1 when using the video laryngoscope.6,7 The experience of the anesthesiologist with difficult airway management and access to certain airway management devices represent important factors in establishing the relative difficulty of managing the airway of a given patient.
Kheterpal and colleagues followed Langeron’s work by determining the incidence and predictors of difficult mask ventilation and impossible bag-mask ventilation in relation to a difficult intubation.8 Kheterpal later observed in more than 50,000 patients9 that 25% of impossible bag-mask ventilations (n = 19) also had difficult intubations and that 10% (n = 2) required surgical airways. The incidence of impossible bag-mask ventilations was 0.15%. Radiation-induced changes in the neck, male sex, obstructive sleep apnea, Mallampati class III or IV, and presence of a beard were identified as independent predictors. Despite the low incidence, the anesthesiologist must anticipate and recognize differences for difficult mask ventilation and difficult intubation while also exercising sound judgment in conducting regional anesthesia in this patient population.
III Use of Regional Anesthesia Versus Preoperative Management of the Airway
In the past few years, interest has increased in using regional anesthesia as the primary anesthesia technique, especially in patients undergoing gynecologic or obstetric; plastic; ear, nose, and throat; trauma; and orthopedic surgery. The literature supports using various techniques for performing regional anesthesia as the primary anesthetic on patients with difficult airways.10–12 We do not recommend performing these cases unless the anesthesiologist has a level of certainty about performing the block. Because of the more expanded use of regional anesthesia, anesthesiologists have become better accomplished at these techniques (e.g., higher success rate, lower frequency of complications). However, no regional technique provides a 100% success rate or is completely free of complications. Regional anesthesia complications include hematoma, nerve injury, and local anesthetic–associated complications, such as cardiac arrest, seizures, and death. When deciding whether to perform a regional technique in lieu of securing the airway preoperatively, these complications should be considered because they may trigger the need for immediate and urgent control of the airway because of a sudden loss of respiratory function (total spinal) or the development of local anesthesia–related complications (e.g., cardiac arrest, seizures).
Occurrence of these complications may be delayed, even if in most cases they occur within minutes after performance of a block. Anesthesiologists must be prepared to control the airway during the entire perioperative period. Although any regional technique intrinsically carries the risk of complications, the relative risk is different for each regional technique. For example, the use of an ulnar block at the wrist for an open reduction and internal fixation of the fifth finger performed using 5 to 6 mL of 0.5% ropivacaine is associated with a much lower risk of local anesthetic toxicity than the use of a transarterial axillary block performed with 40 mL of 0.5% bupivacaine. The specific type of approach, technique (e.g., transarterial, neurostimulator, paresthesia), volume of local anesthetic, and relative proximity of the injection site to a vessel or the central nervous system are some of the factors associated with the risks of toxicity associated with the use of regional anesthesia. Several considerations are important in making the decision to use regional anesthesia in a patient with an established difficult airway (Box 45-1). Knapik and colleagues demonstrated the ability to perform regional anesthesia for valvular heart surgery using a thoracic epidural on a patient with severe pulmonary disease, precluding the use of general endotracheal anesthesia.13 However, during cardiopulmonary bypass, the patient required ventilatory support with a mask technique, a feat that would have been ill advised if difficult mask ventilation was anticipated.
Box 45-1 Regional Anesthesia Versus Control of the Airway in Patients with Established Difficult Airways

Full access? Get Clinical Tree