CHAPTER 16 Regional Anesthesia
Regional anesthesia in infants and children has witnessed an increasing popularity over the years that has taken it from a practice of spinal and caudal procedures, to peripheral and truncal nerve blocks taking advantage of sonographic technology (Rochette et al., 2007). The advances that increased its popularity have presumably also improved the safety of blocks in children, which will ultimately encourage further use of this important practice in intraoperative and postoperative pain management. Despite the advances, it is still important to understand the basics of the practice: the pharmacokinetics and toxicities of local anesthetics and their additives, the anatomy of children at different ages, and the indications and complications of specific regional blocks.
Local anesthesia in children
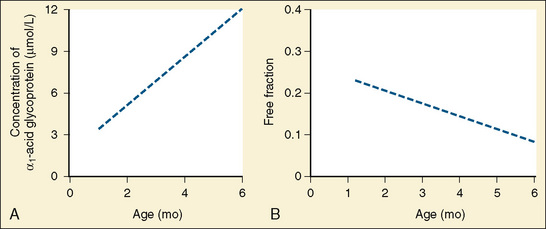
Amide anesthetics are primarily protein bound in the plasma. Bupivacaine, ropivacaine, and levobupivacaine are more than 90% bound to two plasma proteins: α1-acid glycoprotein (high affinity for local anesthetics) and albumin (high volume and relatively low affinity for local anesthetics). It is the free or unbound fraction of the local anesthetic that is physiologically active and is responsible for its effect on the cardiovascular system and the central nervous system (CNS). Infants less than 6 months of age have decreased levels of plasma proteins, resulting in a larger free fraction of local anesthetic, which consequently places this age group at a greater risk for toxicity from these agents (Lerman et al., 1989; Berde, 1992). As an infant matures, the level of plasma proteins increases, and the plasma free-fraction of the drug decreases. Adult levels of protein binding are reached near 1 year of age (Fig. 16-1). Of interest is that α1-acid glycoprotein levels increase in response to surgical stress, and the increased α1-acid glycoprotein ultimately decreases the free fraction of local anesthetic agent. This phenomenon occurs even when total plasma concentration appears to be near toxic levels (Tucker, 1994, 1996; Booker et al., 1996). The liver’s cytochrome P450 system is responsible for the metabolism of amide local anesthetics. These enzymes reach adult activity by the first year of life. The immaturity of liver enzymes in neonates and infants contributes to the decreased clearance of amide local anesthetics seen in this time period.
Ester anesthetics such as chloroprocaine and tetracaine depend on plasma esterases for their elimination. The decreased levels of plasma proteins in neonates and infants are reflected in decreased levels of plasma esterases (Zsigmond and Downs, 1971). However, this has not been shown to be of clinical significance, and tetracaine is commonly used for spinal anesthetics in premature infants for inguinal hernia repairs. Chloroprocaine, although not a commonly used pediatric local anesthetic, has been used for caudal anesthesia. It is thought to afford a greater level of safety than amide anesthetics because of its rapid metabolism (Henderson et al., 1993; Tobias et al., 1996).
Safety Issues
Local Anesthetic Toxicity
Children may be at increased risk for toxicity of local anesthetics because of their relatively increased cardiac output and increased systemic uptake of the agent. This increased systemic uptake may result either in direct CNS toxicity by increasing the amount of local anesthetic available to cross the blood-brain barrier, or in direct cardiac toxicity. Lidocaine at plasma levels of 2 to 4 mcg/mL acts as an anticonvulsant, but at 10 mcg/mL it produces convulsions (Dalens, 1995). Neonates, for example, will manifest symptoms of neurotoxicity such as depressed Apgar scores from lidocaine at umbilical venous blood concentrations of 2.5 mcg/mL, significantly lower than the 5 mcg/mL that is associated with neurotoxicity in adults (Foldes et al., 1960; Shnider and Way, 1968; Ralston and Shnider, 1978; Tucker, 1986).
In unmedicated patients, initial symptoms of neurotoxicity include headache, somnolence, vertigo, and perioral or lingual paresthesia. These symptoms and any objective signs of neurotoxicity such as tremors, twitching, shivering, or even convulsions may not be detected in infants and children under general anesthesia. Diagnosis of local anesthetic toxicity in the child under general anesthesia can be made with indirect signs such as muscular rigidity, hypoxemia without other causes, unexplained tachycardia, dysrhythmias, or cardiovascular collapse. General anesthetics are protective from the CNS effects, but general anesthetics are not protective against cardiac toxicity and may even further contribute to the toxicity (Badgwell et al., 1990). In fact, one study found that in anesthetized ewes, blood concentrations of local anesthetics were doubled because of decreased whole-body distribution and clearance (Copeland et al., 2008a). Net uptake of the local anesthetics in both the heart and brain were greater, with slower efflux, under general anesthesia. Although general anesthesia contributed to local anesthetic–induced cardiovascular depression and changed the overall pharmacokinetics, cardiovascular fatalities occurred only in conscious ewes—there were no fatalities in anesthetized ewes that received intravenous local anesthetics (Copeland et al., 2008b).
The original model that existed was that cardiac toxicity occurs because the local anesthetic prevents the fast inward sodium channels in the myocardium from opening. However, the action leading to toxicity is not at only one specific site, and there is evidence that potassium channels are involved with neuronal excitability and nerve conduction (Kindler and Yost, 2005). Manifestations of toxicity from bupivacaine consist of dysrhythmias with evidence of a high degree of conduction block, widening of the QRS, torsades de pointes, ventricular tachycardia related to reentry phenomena, and major cardiovascular collapse with decreased myocardial contractility (deLaCoussaye et al., 1992). Bupivacaine may produce cardiac and CNS toxicity at serum concentrations of 2 mcg/mL (Tucker, 1986; Dalens and Mazoit, 1998). Although 4 mcg/mL is considered the toxic threshold for bupivacaine in adults, the true toxic concentration of unbound bupivacaine is unknown in humans, particularly children (Knudsen et al., 1997; Luz et al., 1998; Meunier et al., 2001).
Bupivacaine
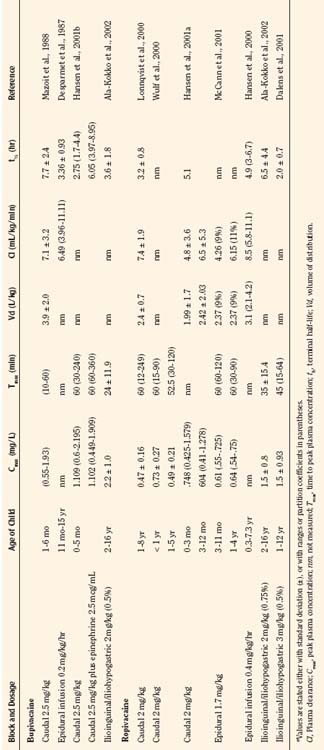
Bupivacaine is a racemic mixture of equimolar amounts of the enantiomers R(+) bupivacaine and S(−) bupivacaine. For many years, racemic bupivacaine was the only amide local anesthetic with long duration and therefore the most commonly used amide local anesthetic in children. Pharmacokinetic studies of a single dose of racemic bupivacaine (2.5 mg/kg) injected in the caudal space have demonstrated differences between infants and children (Ecoffey et al., 1985; Desparmet et al., 1987; Mazoit et al., 1988). Infants have a greater volume of distribution (3.9 L/kg versus 2.7 L/kg), an increased elimination half-life (7.7 versus 4.6 hours), and decreased clearance (7.1 versus 10.0 mL/kg per minute) compared with older children (Table 16-1). Although side effects from bupivacaine are rare, they can be serious, ranging from CNS excitation to cardiovascular collapse from direct cardiotoxicity. A series of case reports of possible toxicity of racemic bupivacaine secondary to continuous infusions of bupivacaine were reported in the early 1990s (Agarwal et al., 1992; McCloskey et al., 1992). In the report of McCloskey and coworkers, children had continuous caudal infusions of 0.25% bupivacaine at dosages between 1.67 and 2.5 mg/kg per hour. One neonate sustained bradycardia and hypotension, and two older children developed seizures. Bupivacaine serum concentrations at the time of the event ranged between 5.6 and 20.3 mcg/mL. In the cases reported by Agarwal and associates (1992), one child who developed a seizure had an intrapleural catheter with a bupivacaine infusion rate of 0.5 mg/kg per hour. The seizure occurred with a plasma bupivacaine level of 5.6 mcg/mL. The other child in this report had a continuous bupivacaine epidural infusion at 1.25 mg/kg per hour, and seizures occurred with a plasma bupivacaine level of 5.4 mcg/mL. Thus, all children in the reports from the McCloskey and Agarwal groups had plasma bupivacaine levels that exceeded bupivacaine’s toxic threshold of 4 mcg/mL.
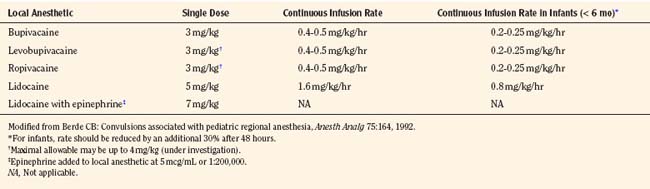
These early cases of toxicity prompted an editorial by Berde (1992), who addressed the false generalization that children were more resistant to local anesthetic toxicity than adults. Although earlier studies involving children noted no evidence of toxicity in patients with plasma concentrations of bupivacaine from 1 to 7 mcg/mL, the use of benzodiazepines in those children may have been protective (McIlvaine et al., 1988). Badgwell and coworkers (1990) reported greater resistance to toxicity in 2-day-old piglets compared with older piglets. However, the direct application of this study to neonates is difficult, because neonates have lower plasma protein concentrations and lower bupivacaine clearance. Berde (1992) recommended that maximal allowable dosages of local anesthetics should not be exceeded (Table 16-2), that infusion rates should be reduced in children with risk factors for seizures, and that the maximal allowable dosages should be reduced by at least 30% for infants less than 6 months of age.
Ropivacaine
Ropivacaine has become a commonly used local anesthetic in pediatric patients, with onset times similar to bupivacaine, and durations of actions that are similar or perhaps slightly longer than bupivacaine (Ivani et al., 1998; DaConceicao et al., 1998, 1999; Lonnqvist et al., 2000; Hansen et al., 2001a; Ivani, 2002). Controversy remains as to the potency of ropivacaine when compared with bupivacaine, and adult studies do not correlate with pediatric studies (Ivani, 2002). Although not confirmed, ropivacaine at 0.2% exhibits the same analgesic effect as 0.25% in children, perhaps because of the intrinsic vasoconstrictive activity that is evident at the lower concentrations used in children (Kopacz et al., 1989; Ivani, 2002). Ropivacaine has a lower risk for CNS and cardiac toxicity than bupivacaine. In fact, inadvertent intravenous ropivacaine in a 1-year-old child failed to produce neurotoxic or cardiotoxic signs or symptoms (Thong et al., 2000). In a pharmacokinetic study of ropivacaine in children ages 1 to 8 who were administered 1 mL/kg of 0.2% ropivacaine for caudal block, the free plasma concentrations were well below toxic levels (Lonnqvist et al., 2000). Clearance of the drug was 7.5 mL/kg per minute, and the terminal half-life was 3.2 hours. Hansen and associates (2001a) studied the pharmacokinetics of caudal ropivacaine in infants less than 1 year of age (see Table 16-1). In this study, infants less than 3 months of age were compared with infants 3 months to 1 year. Although the maximum free concentration of ropivacaine was significantly higher in the younger age group (99 mcg/L versus 38 mcg/L), the total and free plasma concentrations in all of the children less than 1 year were within the range of concentrations previously reported for adults and older children (Lonnqvist et al., 2000; Wulf et al., 2000).
Epidural ropivacaine in children aged 1 to 9 years was studied to determine pharmacokinetics and safety of 24- to 72-hour infusions (Berde et al., 2008). After a 2-mg/kg bolus, an infusion of 2 mg/mL at 0.4 mg/kg per hour was delivered and resulted in plasma concentrations that remained stable throughout the infusion and were well below toxic levels.
Levobupivacaine
Levobupivacaine is the S(−) enantiomer of bupivacaine and is less toxic to the CNS or heart than the racemic bupivacaine (Mazoit et al., 1993; Graf et al., 1997; Huang et al., 1998). The decreased risk for cardiotoxicity from levobupivacaine has been shown in healthy adult volunteers after intravenous administration of either levobupivacaine or racemic bupivacaine (Bardsley et al., 1998). Although similar intravenous studies have not been done in children, animal and human studies suggest less toxicity and equipotency of levobupivacaine compared with bupivacaine (Mather and Chang, 2001; McLeod and Burke, 2001; Gristwood, 2002). In pediatric studies, levobupivacaine has resulted in wide ranges of plasma concentrations when given in the caudal space (Chalkiadis et al., 2004, 2005). When levobupivacaine 0.25% was given in a single-shot caudal dose of 2 mg/mL in children less than 2 years of age, Chalkiadis and coworkers (2004) found that the time to peak plasma concentration ranged between 5 and 60 minutes and was reached later in children less than 3 months of age, and the plasma concentration ranged between 0.41 and 2.12 mcg/mL. In a similar study, but at a dosage of 2.5 mg/kg, the range was 0.62 to 2.4 mcg/mL, with the highest maximum concentration found in a 1-month-old infant (Cortinez et al., 2008). The authors suggested using caution when administering levobupivacaine at 2.5 mg/kg in the caudal space in this age group.
Toxicity Comparison among Commonly Used Local Anesthetics
Multiple studies have compared the risk for toxicity of various local anesthetics. Single high-dosage intravenous injection of the local anesthetics in the ewe model revealed that bupivacaine had the most pronounced changes in electrocardiographic and hemodynamic variables compared with ropivacaine, levobupivacaine, and lidocaine (Guinet et al., 2009). In addition, only the bupivacaine ewes experienced ventricular tachycardia. A recent review suggested that overall, ropivacaine has the greatest margin of safety of the long-acting local anesthetics that are currently available, partially because lipophilicity is a major determinant in local anesthetic toxicity (Zink and Graf, 2008).
Reducing Risks of Toxicity
Several safety measures can reduce the risks of toxicity from local anesthetics in children. One primary safety measure is to avoid overdosing by adhering to recommendations for maximal allowable dosages. For a bolus injection, the maximal recommended dosage of lidocaine is 5 mg/kg. Because epinephrine decreases uptake and absorption of local anesthetic, the dosage of lidocaine can be increased to 7 mg/kg when epinephrine (5 mcg/mL) is added to the local anesthetic. The maximal allowable bolus dosage for bupivacaine, ropivacaine, and levobupivacaine is 3 mg/kg, and the addition of epinephrine does not change the maximum (Agarwal et al., 1992; McCloskey et al., 1992). Recommendations for maximal dosing of continuous infusions (see Table 16-2) are the same for bupivacaine, levobupivacaine, and ropivacaine (Berde, 1992). For epidural infusions, the infusion rates should not exceed 0.4 to 0.5 mg/kg per hour for patients older than 6 months, and the recommendation for neonates is not to exceed 0.2 to 0.25 mg/kg per hour. Based on the clearance of bupivacaine and using the guidelines in Table 16-2, the plasma concentrations should remain below 2.5 mcg/mL and therefore below the toxic level of 4 mcg/mL (Tucker, 1986; Desparmet et al., 1987; Mazoit et al., 1988). These infusions assume a loading dosage of 2 to 2.5 mg/kg of bupivacaine and should be reduced by 25% in patients with risk factors for seizures (i.e., past history of febrile seizures, hypomagnesemia, and hyponatremia) (Agarwal et al., 1992; Berde, 1992).
Although there is extensive literature on maximal allowable dosing of local anesthetics, recommendations in children are mostly extrapolated from adults. Additionally, the recommendations for adults are not evidence based and are in turn extrapolated from animal experiences, blood concentration studies, local anesthetic toxicity case reports, and pharmacokinetics (Rosenberg et al., 2004). In the adult literature, it has even been suggested that the idea of maximal blanket dosing be abandoned, as it is not scientifically valid or clinically relevant (Heavner, 2004). This criticism suggests that the maximum dosages that are quoted to be valid in all patients are not truly valid, and one blanket recommendation does not actually cover all types of patients or all types of blocks. Instead, block- and site-specific guidelines are needed so that dosing is tailored to the patient’s situation. In addition, dosing must be based on children’s per-kilogram weight; this is the only way to safeguard the risk of overdosing local anesthetics in different age groups.
In addition to dosing guidelines, the risk for toxicity is also affected by hypothermia, hypoxia, hypercarbia, acidosis, or hyperkalemia (Broadman, 1996). These factors enhance the toxicity of local anesthetics by different mechanisms. Another factor that leads to increased toxicity is the speed of injection of the local anesthetic agent. Rapid injections can cause toxicity by resulting in a rapid high peak that may not allow the sodium channels to adapt for the local anesthetic action.
When local anesthetics are combined, their toxicities are additive. Therefore, if the maximal allowable dosage of one local anesthetic has been reached, another local anesthetic agent should not be delivered (Giaufre et al., 1996). Although combining local anesthetics may be common at some centers, maximal allowable dosing should be calculated for each of the anesthetics used and decreased based on the relative percentage of each.
The choice of local anesthetic is a clinical decision. The risks for potential cardiotoxicity have been discussed and should help guide practitioners in choosing a local anesthetic that they feel has the greatest safety margin. After the local anesthetic is chosen, the concentration must be considered. In general, lower concentrations of local anesthetics such as 0.25% bupivacaine or levobupivacaine and 0.2% ropivacaine may be used in infants and small children, and higher concentrations such as 0.5% bupivacaine, levobupivacaine, or ropivacaine should be reserved for older children. Higher concentrations result in longer duration of action and increased motor block, but the total milligram dosage must be calculated carefully. Additionally, in young children there is a risk for direct local anesthetic toxicity on developing nerves (Selander, 1993; Lambert et al., 1994; Radwan et al., 2002). The age at which this is no longer a concern is unknown.
Test dosing
Before injecting local anesthetics, it is essential to determine that the agent will not be injected into the intravascular space. The absence of blood aspiration when administering a pediatric block is not a reliable indicator that the needle is not in a vessel. Infants, in particular, may be at greatest risk of intravascular injection (Freid et al., 1993; Ved et al., 1993; Flandin-Blety and Barrier, 1995). Although clinical practice has relied on a test dose to elicit a tachycardia when the test drug is inadvertently injected systemically, the test dose was often considered unreliable in the anesthetized patient and its usefulness continues to be questioned (Desparmet et al., 1990; Sethna and McGowan, 2005). In Desparmet’s study of children anesthetized with halothane, only 16 of 21 children who received a test dose of 0.1% lidocaine with epinephrine 1:200,000 had an increase in heart rate that was greater than 10 beats per minute (bpm). Therefore, under halothane anesthesia, an increase of 20 bpm with prior administration of atropine improves the efficacy of the test dose. Sethna and associates (2000) determined that, with the patient under isoflurane anesthesia and after pretreatment of atropine, 0.75 mcg/kg epinephrine was more reliable than 0.5 mcg/kg. All patients in the 0.75-mcg/kg group had heart rate increases of 10 bpm or greater. Isoproterenol has also been used as a test drug, but although it is a more reliable indicator of an intravascular injection in patients anesthetized with halothane (Perillo et al., 1993; Kozek-Langenecker et al., 1996), its safety with neuraxial administration has not been determined, so it is not recommended for this use presently. The validity of test dosing has been studied and reviewed (Tanaka and Nishikawa, 1998, 1999; Tobias, 2001b). With the patient under sevoflurane anesthesia, Tanaka and Nishikawa (1998, 1999) were able to demonstrate that an increase in heart rate of 10 bpm, an increase in T-wave amplitude of 25%, or an increase in blood pressure of 15 mm Hg or more defines the criteria for a positive test dose. Prior administration of atropine did not affect these criteria. Varghese and coworkers (2009) had similar results when 0.1 mL/kg of intravenous 1% lidocaine with 5 mcg/mL epinephrine was injected in children under sevoflurane anesthesia to determine if T-wave amplitude would be visibly detectable on the monitor. An increase in T-wave amplitude in lead II was detected on the electrocardiographic (ECG) monitor in 91% of children and noted on the ECG strip in 94% of children. The amplitude change was considered more reliable for detecting intravascular injection than the increase in heart rate of 10 bpm, which occurred in 64% of children, or the increase of 15 mm Hg or greater in systolic blood pressure, which occurred in 76%. The increase in T-wave amplitude occurred within 30 seconds, as was found in other studies (Tanaka and Nishikawa, 1998; Kozek-Langenecker et al., 2000). Langenecker and associates (2000) delivered an epinephrine solution at 0.5 mcg/kg without being mixed in a local anesthetic and also concluded that the T-wave criterion was more reliable than hemodynamic criteria for a positive test dose.
A test dose can be a useful tool for identifying intravascular injection when the appropriate criteria are used. The test dose should not, however, be a replacement for slow incremental dosing of the total volume of the local anesthetic, with attention to vital sign and ECG monitoring throughout the drug administration. A recommended test dose under sevoflurane anesthesia is 0.1 mL/kg of the chosen local anesthetic with epinephrine 5 mcg/mL added, not to exceed 3 mL. A heart rate increase of 10 bpm, a systolic blood pressure increase of 15 mm Hg, a T-wave amplitude increase of 25% or greater from baseline, or bradycardia should alert the practitioner to possible intravascular injection (Freid et al., 1993; Fisher et al., 1997; Tanaka and Nishikawa, 1998, 1999; Tobias, 2001b).
Although it has not been extensively tested under total intravenous anesthesia (TIVA), there is evidence that the test dose criteria used for determining intravascular injection differ between TIVA and inhaled anesthesia (Polaner et al., 2010). Arterial blood pressure was the most consistent finding, with an increase in all patients of at least 30% within 2 minutes of injection. Heart rate increased by 10 bpm in only 73% of children, and t-wave amplitude was not reliable. Of note in this study, the injectate was 0.1 mL/kg bupivacaine 0.25%, with epinephrine 1:200,000.
Another advantage of epinephrine administration in regional anesthesia is that, in addition to its being a reliable marker for intravascular injection, its use decreases systemic absorption of the local anesthetic (Eyres et al., 1983, 1986). Children may be at increased risk for local anesthetic toxicity from increased systemic absorption because of their relatively higher cardiac output and regional blood flow. In a study comparing bupivacaine with epinephrine 5 mcg/mL to bupivacaine alone in children for fascia iliaca block, Doyle and coworkers (1997) demonstrated that the peak plasma concentration was lower in the bupivacaine-with-epinephrine group (0.35 mcg/mL versus 1.1 mcg/mL), and that the time to peak concentration was more gradual (20 minutes versus 40 minutes from injection). Similarly, the addition of epinephrine to caudal ropivacaine significantly lowers the maximal concentration of ropivacaine and delays the time to maximum concentration, thus improving the safety profile in children (Van Obbergh et al., 2003). In adults, this same delay in systemic absorption and a reduced peak plasma concentration have been shown when epinephrine was added to ropivacaine for paravertebral block (Karmaker et al., 2005). These findings do not suggest that the addition of epinephrine extends the duration of analgesia, but they do demonstrate the effects of epinephrine on the pharmacokinetics of local anesthetics, including those with intrinsic vasoconstrictive properties. Epinephrine (2.5 to 5 mcg/mL) should be added to local anesthetic doses, particularly when large volumes are used, to reduce the risks of local anesthetic toxicity (Rosenberg et al., 2004).
Management of Local Anesthetic Toxicity
Despite all efforts to safely deliver a local anesthetic to a child, it is still possible for local anesthetic toxicity to occur, either by undetected intravascular injection or from inadvertent overdose. When it is apparent that there is local anesthetic toxicity, the practitioner must act quickly to prevent the serious cardiac complications that may ensue. The first steps should focus on the basics, with attention to oxygenation, ventilation, and cardiovascular resuscitation. In particular, hypercarbia must be avoided when resuscitating a patient with local anesthetic toxicity, as an increased Paco2 displaces local anesthetics from their plasma protein binding sites (Burney et al., 1978).
A significant change in the overall management of local anesthetic toxicity has been the introduction of the delivery of a lipid emulsion (Weinberg, 2006). In the clinical arena, lipid emulsion has been used to treat the neurotoxicity and cardiotoxicity that occur from bupivacaine, levobupivacaine, ropivacaine, and mepivacaine (Foxall et al., 2007; Litz et al., 2008; Warren et al., 2008; Marwick et al., 2009). These long-acting local anesthetics are highly soluble in lipid emulsion, and this high binding capacity explains the clinical efficacy of action, although several mechanisms of action have been proposed (Weinberg et al., 2006).
When comparing lipid emulsion (Intralipid) with epinephrine for bupivacaine-induced cardiotoxicity in a rat model, the lipid infusion resulted in better overall resuscitation hemodynamics than epinephrine (Weinberg et al., 2008). In addition, epinephrine resulted in higher lactate levels, hypoxemia, a mixed acidosis, and persistent ventricular ectopy. When compared with saline, epinephrine had similar hemodynamic and metabolic metrics during resuscitation.
Many questions remain regarding the use of Intralipid, and no clear consensus has been reached as to when Intralipid should be delivered (Weinberg, 2009). One school of thought is that the potential risks of administering the high dosages of Intralipid are yet uncertain, and therefore it should be used only after advanced cardiac life support has failed (Corman and Skledar, 2007). Potential risks include infection, intravenous thrombophlebitis, altered inflammatory responses, anaphylaxis, and fat emboli (Brull, 2008). Serum amylase increases and the risk for acute pancreatitis are concerns (Marwick et al., 2009). Certainly for the neonate, who is less likely to be able to handle a large Intralipid load, caution should be used and the risk-benefit ratio weighed prior to dosing. These risks certainly exist, but withholding Intralipid in the event of a local anesthetic–induced arrest would not be advised. The question remains whether it should be the first step in the resuscitation. Intralipid impairs return of cardiac function in the presence of profound hypoxia (Harvey et al., 2009). Likewise, Mazoit and associates (2009) found that a drop in pH, as might occur during resuscitative efforts, decreases the affinity of lipid emulsion for the local anesthetics ropivacaine and bupivacaine. Particularly after the use of epinephrine at dosages of 10 mcg/kg or higher, there is a decrease in successful resuscitation efforts in the presence of bupivacaine toxicity (Hiller et al., 2009). Although epinephrine results in a faster onset of spontaneous circulation than lipid rescue, the effect is not prolonged, and the overall inefficiency in resuscitation in the presence of this dosage of epinephrine probably results from high levels of lactate. These studies would support the early use of Intralipid for improved result.
To effectively use Intralipid, it should be immediately available with clear instructions attached for the practitioner. Dosing guidelines are presented in Box 16-1. As discussed, no specific guidelines have yet been established, and dosing relies only on a series of case reports and animal studies. Nevertheless, having some starting point is essential. A sufficient quantity of Intralipid must be immediately available, as it is possible for a patient to have recurrence of cardiotoxicity after lipid rescue that may require additional support (Marwick et al., 2009). It is important to distinguish that a 20% lipid emulsion has been effective for resuscitation, not propofol, which is 10% Intralipid and 1% propofol and would contribute further to cardiovascular depression in the arrest situation (Weinberg et al., 2004).
Box 16-1 Dosing Guidelines of Intralipid Infusion for Local Anesthetic Toxicity
Repeat dose
Every 3 to 5 minutes during resuscitation
1 to 1.5 mL/kg of 20% Intralipid over 1 minute, up to a total of 3 mL/kg
A website (http://lipidrescue.org) was developed to disseminate information about lipid rescue therapy and to allow practitioners to share their experiences.
Regional Anesthesia in the Anesthetized Child
A significant difference between adult and pediatric regional anesthesia is that children typically receive their regional anesthetic while they are under general anesthesia. This practice remains controversial outside of the pediatric arena (Bromage, 1996; Bromage and Benumof, 1998; Rosenquist and Birnback, 2003). Because of issues regarding patient cooperation, the practice of performing a regional anesthetic in children differs greatly from placing a block in an adult. Performing regional anesthetic blocks during general anesthesia in children, including thoracic epidural blocks, is an accepted practice as long as the individual has the proper training and expertise. Over 50 international pediatric anesthesiologists signed an editorial by Krane and coworkers (1998) to support the placement of blocks in anesthetized children. In fact, “It would be considered malpractice to perform such techniques in patients who were not fully anesthetized” (Dalens, 1999), and “Any performance of a block in an agitated and moving child is not only unethical, but could be dangerous when the needle approaches the delicate nervous structures” (De Negri et al., 2002). A large retrospective study of 4298 adult thoracic surgical patients who underwent epidural catheter placement while under general anesthesia revealed no neurologic complications including radicular symptoms or persistent paresthesias (Horlocker et al., 2003a).
In children who are under general anesthesia or who are heavily sedated, it may be difficult to recognize intravascular injection of a local anesthetic. Even in the awake child, recognizing the signs or symptoms of local anesthetic toxicity is challenging, and it would be optimistic to think that the child would be able to relay this information early in the injection phase. For this reason, the practice of test dosing with a local anesthetic with the addition of epinephrine has been readdressed, and this should be a common practice as it is more reliable than patient report for detecting or preventing intravascular injection (Tobias, 2001b; Bernards et al., 2008). It is also argued that an anesthetized child cannot warn the practitioner of a significant paresthesia and the potential risk for neurologic injury from intraneural placement of a needle or anesthetic. This is a hypothetical risk that has not been supported by reports of large series of pediatric regional anesthetics (Pietrapaoli et al., 1993; Goldman, 1995; Giaufre et al., 1996).
The American Society of Regional Anesthesia and Pain Medicine issued a practice advisory that was based on evidence and expert opinion as it pertains to performing procedures on anesthetized or heavily sedated patients (Bernards et al., 2008). These recommendations (see Box 16-2) differ somewhat from the recommendations set forth for adults.
Box 16-2 Recommendations* for Performing Regional Anesthesia in Anesthetized or Heavily Sedated Children
Modified from Bernards CM, Hadzic A, Suresh S, et al: Regional anesthesia in anesthetized or heavily sedated patients, Reg Anesth Pain Med 33:449, 2008.
An additional concern with regional anesthesia in an anesthetized child is that of “wrong-side block” for a unilateral extremity procedure. Universal protocols must be followed in the conscious child: the operative extremity must be appropriately marked by the surgical team with concurrence of a witness as well as the parent, and the consent must be checked for accuracy regarding the appropriate site. A time-out should occur before blocking the anesthetized child, to again check the consent and marked site. See related video online at www.expertconsult.com. 
Direct Nerve Toxicity
The use of local anesthetics and neurotoxicity on the developing nerve is an area that continues to be addressed. Animal data have demonstrated that all local anesthetics are potentially neurotoxic, and this neurotoxicity parallels their anesthetic potency (Selander, 1993). The factors that contribute to the mechanism of the neurotoxicity include the concentration of the local anesthetic and the time of exposure of the nerve to the local anesthetic. This is important in children, particularly in neonates, who may be at greatest risk for direct neurotoxicity during nerve development and therefore should not receive the higher concentrations of local anesthetics. Studies on rabbit nerve fibers have demonstrated an increased sensitivity to the blocking effects of local anesthetics in young nerves (Benzon et al., 1988). Additional in vitro biological investigation has demonstrated that lidocaine, bupivacaine, mepivacaine, and ropivacaine are all capable of producing growth cone collapse and neurite degeneration (Radwan et al., 2002). However, the incidence of growth cone collapse with bupivacaine and ropivacaine is insignificant when compared with lidocaine and mepivacaine. This finding has not been consistent. When looking at cytotoxicity of local anesthetics on peripheral nerves by measuring viability and apoptotic activity, although all local anesthetics decreased cell viability in a concentration-dependent fashion, bupivacaine had the greatest effect (Castro-Perez et al., 2009). The order of the killing potency (based the concentration at which 50% of cells are killed, or the median lethal dose [LD50]), from high to low, was bupivacaine, then ropivacaine, then chloroprocaine, then lidocaine, then mepivacaine, and finally, with much lower effect, procaine. Only bupivacaine and lidocaine killed all cells with increasing concentration and could cause apoptosis with either the increased concentration or time of exposure. The authors of the study concluded that cytotoxicity-induced nerve injury may have different mechanisms for the various local anesthetics, and that the targets may not be neurons, because they found that bupivacaine was the most toxic local anesthetic that they tested, but it has a history of having a low incidence of producing transient neurologic symptoms in the postoperative period.
Risk of Infection
Another safety consideration concerns the risk for infection. An initial way to avoid infection is by preparing the skin prior to a regional block. Before placing any block, sterile preparation of the skin should be performed, but this is particularly important for central blocks, to reduce the risk for meningitis or epidural abscess. Chlorhexidine, despite its labeling, is the agent of choice for preparing the skin prior to regional anesthetic block (Hebl, 2006). It is recommended over the use of povidone iodine (Povidine), as it has been shown to decrease colonization when used in young children for epidural catheter placement (Kinirons et al., 2001; Wagner and Prielipp, 2003). In addition, povidone iodine may be harmful to the very sensitive skin of an infant. If used, the povidone iodine should be allowed to dry and not be carried centrally with the needle into the epidural or subdural spaces. After the block has been placed, the iodine should be washed from the skin to avoid iodine burns.
The actual risk for infection from regional techniques, however, is extremely low. For indwelling caudal catheters, the incidence of catheter tip colonization is 20%, as opposed to 4% for indwelling epidural catheters (McNeely et al., 1997b). No patients with bacterial colonization of the catheters exhibited systemic signs of infection. Strafford and associates (1995) studied 1620 children who received epidural catheters. There were no infections in the children who had the catheters placed for postoperative analgesia, and only one significant infection in an immunosuppressed child who received a long-term catheter for pain secondary to her malignancy (Strafford et al., 1995). Adult review has confirmed that infections are typically limited to long-term indwelling catheters in cancer patients (Ruppen et al., 2007). Giaufre and coworkers (1996), in a prospective study of over 24,000 regional techniques performed in children by members of the French-Language Society of Pediatric Anesthesiologists, reported no infections.
Compartment Syndrome
A concern often cited for failure to perform a regional anesthetic in pediatric patients for orthopedic procedures is the risk of an unrecognized compartment syndrome. Compartment syndrome puts the child at risk for muscle ischemia or loss of limb and must be recognized early so that decompressive fasciotomy may occur if necessary prior to these serious complications. The concern focuses on the possibility that the use of a local anesthetic in a regional block may mask the initial symptoms of the sensation of pressure in the limb that occurs with compartment syndrome (Dunwoody et al., 1997). Case reports in children have demonstrated that a successful epidural block with a low concentration of local anesthetic does not mask the symptoms of compartment syndrome. A literature review to assess the risk for compartment syndrome in children who have received epidurals revealed 12 cases (Johnson and Chalkiadis, 2009). In all cases, pain was the primary finding and was considered more severe than the clinical situation would explain. Five of the patients had compartment syndrome as a result of lithotomy position rather than operative site edema. The authors concluded that warning signs of compartment syndrome are the presence of increasing pain or pain that is remote to the site of surgery, an increase in analgesic requirements, paresthesia not due to analgesia, reduced perfusion, swelling, and pain on passive movement. They suggested that the presence of the epidural catheter did not result in delayed diagnosis but instead contributed to deficiencies in the system. Recommendations made included the following: educate staff as to the signs and symptoms of compartment syndrome, identify which patients are particularly at risk through discussion with the surgeon, use dilute local anesthetic solutions, site epidural catheters as close as possible to involved dermatomes, and assess distribution and density of block frequently. Serial examinations should be performed on children to assess the operated extremity in the presence of good analgesia. For the high-risk child, or if any question exists, measure compartmental pressures postoperatively, particularly in children who would clearly benefit from infusions of local anesthetic, such as those who have undergone microvascular surgery or amputation.
Consent Issues
Performance of a regional block must follow the same guidelines as performance of a surgical procedure with consideration of the risk-benefit ratio, a discussion of complications, and appropriate documentation to support its use. Not only should the more common complications be discussed, but the rare, serious complications should also be part of the preoperative consent process with regard to block placement in a child (Domino, 2007). The manner by which this occurs varies with the country in which the procedure is performed, but some effort must be made to make the parents aware of the purpose, benefits, and risks of regional anesthesia for their child (Lonnqvist et al., 2009).
Reviews of Safety of Regional Anesthesia in Children
Despite the issues of the safety of regional anesthesia in children, studies have shown that the risks and complications of regional anesthesia in children are quite low and often preventable (Dalens and Hasnouai, 1989; Pietropaoli et al., 1993; Giaufre et al., 1996; Dalens and Mazoit, 1998). The largest of these studies was published by the French-Language Society of Pediatric Anesthesiologists (ADARPEF) (Giaufre et al., 1996). This prospective report included 24,409 regional blocks performed over 1 year in children. Central blocks accounted for greater than 60% of the blocks, whereas peripheral nerve blocks and local anesthetic techniques made up the remaining 38%. Only 25 complications occurred in the study, and all the complications occurred in children who received central blocks. Thus, the overall complication rate of regional anesthesia was 0.9 per 1000. The most common complications from regional blockade were inadvertent dural puncture (n = 8), inadvertent intravascular injection of local anesthetic (n = 6), technical problem (n = 3), and overdosing of local anesthesia leading to dysrhythmias (n = 2). In addition, two children had transient paresthesias, one child had apnea after central morphine, and one child had a skin lesion after a caudal anesthetic administration. There were no deaths secondary to any of the complications. The conclusion from this study of regional anesthesia in children was that complications were rare and minor, and that they occurred most often in the operating room where they were readily managed. In addition, when appropriate, a peripheral nerve block may be preferable to a central block.
In a retrospective review of 24,005 regional anesthetics administered over a 10-year period, Flandin-Blety and Barrier (1995) reported 108 events without sequelae (0.45%). However, in this review, five events resulted in severe neurologic injury, including tetraplegia in three children, paraplegia in one child, and one child with cerebral lesions. All five of the children were healthy and less than 3 months of age. Four of the five children had loss of resistance to air used in their technique to identify the epidural space. The true pathophysiologic causes for the neurologic injuries in these children are unknown, but the authors recommended that air not be used to identify the epidural space, and a lower concentration of epinephrine (e.g., 2.5 mcg/mL) be used to avoid possible ischemic injury. In addition, the authors recommended that the indications for regional anesthesia be reconsidered in children less than 18 months of age because of their incomplete myelination of neuronal fibers.
Recent studies have also looked at new technology and whether these advances have improved the practice of regional anesthesia. Rubin and associates (2009) reviewed the literature on ultrasound-guided blocks and suggested that improved safety features included the need for a lower volume of local anesthetic, and better visibility. How these findings extrapolate to whether ultrasound improves overall safety of regional blocks in children is unclear and not adequately demonstrated except for ilioinguinal blocks.
Introduction to ultrasound
Before discussing specific blocks in pediatric anesthesia, the place of ultrasound in the practice of pediatric regional anesthesia should be appreciated. The use of ultrasound for regional anesthesia has experienced immense growth in recent years. The premise of image guidance for nerve localization could not have a better suitor than a developing pediatric anatomy that defies predictable landmarks and has a narrow margin of safety. Despite the demonstrated reduction in the volume of local anesthetic required, the faster onset and longer duration of sensory and motor blocks, and improved quality of sensory block, randomized, controlled studies examining the safety and efficacy of ultrasound-guided nerve blocks in children have been lacking (Marhofer et al.,1997, 1998, 2004; Willschke et al., 2005, 2006a). Therefore, this subject should be approached with the understanding of its evolving nature.
The development of ultrasound technology stems from the principles of piezoelectricity, the ability of crystals and certain other materials to generate an electric potential in response to applied mechanical stress. This effect was first described by brothers Pierre and Jacques Curie in 1880, shortly followed by the demonstration of the converse piezoelectric effect (strain to crystals when an electric field is applied) by Gabriel Lippmann in 1881. However, it took the military innovations of World War I, where ultrasound (sonar) was used to detect submarines, to fuel its use in the medical arena. The first Doppler-assisted nerve block was described in 1978 to locate the subclavian artery for placement of supraclavicular brachial plexus block, but it was not until 1994 that the two-dimensional imaging improved to allow for real-time visualization of the supraclavicular brachial plexus with observation of local anesthetic spread (la Grange et al., 1978; Kapral et al., 1994). Ultrasound guidance has since been used to visualize most remote peripheral and central nerves in both adults and children. This field continues to expand as portable machines with high-resolution capabilities are perfected and three-dimensional ultrasound delineates additional sonoanatomy (Clendenen et al., 2009).
Physics of Sonography
Doppler
When performing regional blocks, it is important to visualize and avoid vascular structures. Color Doppler ultrasonography uses the Doppler effect (a frequency shift that occurs when either a wave source or receiver moves) to assess blood flow and overlays the color velocity mapping on the two-dimensional gray image. The moving red blood cells act as a reflecting medium in the vessels and amplify the perceived signal frequency (red) when moving toward the transducer or diminish it when moving away (blue). The red and blue reflect the direction of the flow to the transducer, not whether the flow is arterial or venous. The image appears black when the wave hits red blood cells perpendicular to the flow. Power color Doppler is a recent alternative that enhances flow detection regardless of the angle of incidence, but it lacks directional information (Rubin et al., 1994).
Artifacts
The complex physics behind ultrasound image derivation frequently creates image distortions with no anatomic basis. Accurate interpretation not only avoids erroneous needle adjustment but also guides corrective action (Sites et al., 2007a, 2007b). Suspect structures can be confirmed by examining them in a second plane.
Types of Ultrasound Transducers
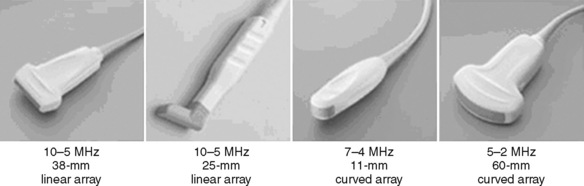
Selection of transducer type, footprint size, and frequency are critical to successful nerve block performance (Fig. 16-2). Linear transducers produce rectangular images and offer superior sonographic views for superficial structures (<4 cm). This ability makes this type of transducer ideally suited for the majority of pediatric examinations. Hockey-stick probe configuration offers the additional advantage of smaller footprint (25 mm), ergonomic shape capable of navigating the pediatric landscape, and a broadband frequency (6 to 13 MHz) adequate to examine even deep pediatric blocks such as the psoas compartment block. Curvilinear probes create a wedge-shaped image capable of reaching deep structures, but they sacrifice lateral resolution as the beam disperses in the far field of the curved array. This type of transducer is useful for working with teenagers and obese children to perform deeper blocks or for epidural guidance. Phased-array transducers have the smallest footprint and electronically guide their beam to diverge distally. They produce deep panoramic views most suited for transthoracic echocardiography and hold little use for regional practice.
Training and Safety
Inexperience is highly correlated with an increased complication rate, and in this age of heightened patient safety, awareness may preclude talented physicians from realizing the benefits of ultrasound-guided regional anesthesia. Recent publications have increasingly focused on optimizing the learning environment and on designing a learner-centered curriculum (Sites et al., 2007c; Smith et al., 2009). The most common novice behavior patterns that were associated with poor block outcomes are as follows: (1) advancement of the needle when the tip was not well visualized, (2) unintentional probe movements, (3) failure to recognize an intramuscular location of the needle tip before injection, (4) poor ergonomics, (5) failure to identify maldistribution of local anesthesia, (6) operator fatigue, (7) failure to correctly correlate ultrasound sidedness to patient’s anatomy, and (8) inappropriate choice of needle insertion site and angle.
Role of the Nerve Stimulator in the Age of Ultrasound
Regional anesthesia took a giant step forward when it abandoned paresthesia and field infiltration for nerve localization and developed a scientifically based, quantitative technique of nerve stimulation (NS). In its 30-year reign, NS has demonstrated a high degree of safety and success rates (Neal et al., 2002). Today, ultrasound guidance offers a qualitative anatomic endpoint, provides the ability to observe local anesthetic spread during injection, and can be used to identify abnormal anatomy. However, it is difficult to be a staunch proponent of solo methodology when both modalities offer complementary evidence of needle-to-nerve proximity and may reduce the time necessary for trainees to successfully reach the desired peripheral nerve block (Orebaugh et al., 2007). Pediatric regional anesthesia presents the additional challenges of working with anesthetized patients unable to report pain on injection, and smaller nerve size that is difficult to locate by NS alone, especially in patients less than 10 years of age (Gurnaney et al., 2007). In addition, NS may yield functional information on proximity to other nerves (phrenic stimulation in parascalene/supraclavicular nerve blocks) and alert to intrafascicular injection when evoked motor response is present with less than 0.2 mA, although this is not a uniform finding (Tsai et al., 2008). Thus, it is reasonable to advocate dual guidance in performing nerve blockade on nerves capable of NS (Gebhard et al., 2008).
Central neuraxial blockade
Central blockade is performed in children for many of the same reasons that it is performed in adults, such as for bilateral lower extremity, abdominal, and thoracic procedures. The risks and benefits to performing central blocks are inherent to the type of block chosen. Central blocks performed in children include spinal blocks and epidural blocks, with the caudal technique being the most commonly used approach to the epidural space. Contraindications to central blockade include a child on anticoagulation therapy, a patient with a preexisting coagulopathy, and a patient or parent who refuses consent for the procedure. The guidelines for regional anesthesia and anticoagulation therapy in adults should be reviewed, as they may be useful for guiding the management of the child (Horlocker et al., 2003b).
Spinal Anesthesia
Spinal anesthesia was a very early form of regional anesthesia that was considered useful for children (Bainbridge, 1901; Tyrell-Gray, 1909). Since that time, spinal anesthetics have become an important anesthetic technique for reducing the incidence of postoperative apnea in premature and expremature infants (Harnik et al., 1986; Welborn et al., 1990; Krane et al., 1995; Somri et al., 1998). Infants who have continuing apnea at home, or a hematocrit of less than 30% are at particular risk for postoperative apnea (Cote et al., 1995; Welborn et al., 1991). Spinal anesthesia may also reduce the need for postoperative mechanical ventilation in infants who are less than 60 weeks of postconceptual age and after hernia repair (Huang and Hirshberg, 2001). The ability of a spinal anesthetic to densely block the dermatomes involved in inguinal hernia repair has kept this regional technique a popular choice in pediatric anesthesia for inguinal surgery. Often, a spinal anesthetic combined with liberal clear liquids until 2 hours before the procedure, and a pacifier intraoperatively, are enough to keep an expremature infant comfortable while he or she undergoes inguinal hernia repair. However, any expremature infant up to 44 weeks of postconceptual age, and up to 60 weeks of postconceptual age if the infant has risk factors such as anemia or ongoing apnea, should be a candidate for overnight monitoring after the surgery, whether or not a pure regional technique was used.
Although spinal anesthesia may be used in any age group, there are relatively few true indications for a spinal anesthetic in older children, who may be at increased risk for post–dural puncture headaches (PDPHs) from the technique (Wee et al., 1996).
Anatomy
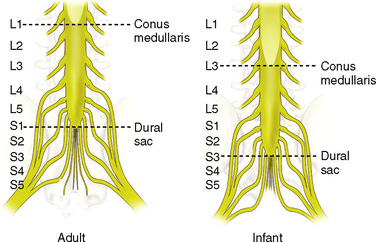
The anatomic differences between an infant and a young child or adult are clinically significant and must be taken into consideration when performing a spinal technique. Common teaching has always suggested that the dural sac in a newborn ends at S3, and the conus medullaris may be located at L3 (Fig. 16-3). Willschke and coworkers (2007), however, in a study of 145 neonates using ultrasound for epidural catheter placement, determined that the termination of the spinal cord in neonates actually ended at a median of L2. Likewise, Shin and associates (2009) found that the end of the dural sac was at a median level of the upper S2 in children less than 36 months of age. Even in children up to approximately 6 years of age, the dural sac ascended only slightly on sonographic examination, to remain near the level of S1 or S2 (Shin et al., 2009). This differs significantly from the final position in adults.
Technique
A sterile preparation and a clear plastic drape are used so that the anatomy may be seen (Fig. 16-4). For neonates and infants, a 1½-inch 22-gauge spinal needle is inserted at the L4-5 interspace. The stylet of the needle should be in place when it is passed through the skin. This avoids the remote risk for an epidermoid tumor (Shaywitz, 1972; Barnitzky et al., 1977). Using this size needle in this age group, a pop will be felt as the needle enters the ligamentum flavum, and another pop as the needle enters the dura. The stylet is removed to check for the flow of CSF. In a baby positioned in the lateral position, if no CSF is evident after what seemed to be appropriate needle placement, then the procedure may be repeated with the infant in the sitting position to improve CSF flow.
After confirmation of position into the subarachnoid space as evidenced by free flow of CSF through the needle, the local anesthetic solution is slowly injected. After the injection, the needle is removed and the child is placed in the supine position. It is extremely important that the child remain supine and that the legs not be raised for any reason, including placement of electrocautery pad. Lifting the legs will cause the local anesthetic to migrate and result in an undesirable high spinal blockade (Wright et al., 1990).
Dosing
The total volume of CSF in a neonate is 4 mL/kg, compared with 2 mL/kg in an adult, and the hydrostatic pressure is 30 to 40 mm H2O, lower than that of an adult. In addition, almost half of the total CSF volume is in the spinal subarachnoid space, whereas only one fourth of the total volume in adults is found in the spinal region. These factors play an important part of dosing spinal blocks, as the local anesthetics are quickly diluted by the CSF in a neonate on injection. Infants require higher volumes based on weight, but the duration of action of spinal blocks are shorter than in adults (Rice et al., 1994).
Although many different dosing regimens have been used, tetracaine either with or without epinephrine is a commonly employed local anesthetic for spinal anesthesia. Rice and associates (1994) studied 100 infants to determine the duration of spinal block, and the authors compared three groups: lidocaine 3 mg/kg with epinephrine, tetracaine 0.4 mg/kg plain, and tetracaine 0.4 mg/kg with epinephrine. The duration in the lidocaine with epinephrine group was 56 ± 2.5 minutes, the tetracaine plain group was 86 ± 4 minutes, and the tetracaine with epinephrine group was 128 ± 3 minutes.
When using 1% tetracaine for a spinal block in an infant, a dosage of 0.5 mg/kg mixed in an equivalent amount of 10% dextrose to make the solution hyperbaric should provide at least 90 minutes of surgical analgesia. Yaster and Maxwell (1989) suggested that regardless of the infant’s weight, 1.5 to 2 mg of tetracaine is the minimal effective dosage. To achieve 5 mg/mL of tetracaine, mix 1 mL of 1% tetracaine with 1 mL of 10% dextrose in water (D10W). The delivered volume is then 0.3 to 0.4 mL for infants less than 10 kg in weight. If 0.01 mL/kg of epinephrine is added to 0.75 to 1 mg/kg of hyperbaric tetracaine, surgical analgesia can be extended up to 120 minutes. Similarly, the use of clonidine will extend a spinal block in a former preterm infant, but the risk for apnea may be increased (Rochette et al., 2005). When using bupivacaine for spinal block, 0.5 to 0.6 mg/kg of either isobaric or hyperbaric bupivacaine will provide an average of 80 minutes of surgical analgesia (Dalens, 2000). Dosing of bupivacaine should be reduced for infants and young children who are greater than 5 kg in weight, because of changes in CSF volume. For infants or toddlers 5 to 15 kg, the dosage of hyperbaric bupivacaine or tetracaine is 0.4 mg/kg or 0.08 mL/kg, and for children weighing more than 15 kg, the dosage of bupivacaine or tetracaine is 0.3 mg/kg or 0.06 mL/kg (Dalens, 1995).
Isobaric ropivacaine has been studied in children for spinal anesthesia at a dosage of 0.5 mg/kg up to 20 mg (Kokki et al., 2005). The mean highest sensory level of block was T6 and duration was 96 minutes with a range of 34 to 210 minutes. Additional study on intrathecal ropivacaine is warranted.
Complications
Complications during spinal anesthesia in children are uncommon. In the ADARPEF study, an intravascular injection during spinal anesthesia was the only reported complication in 506 cases (Giaufre et al., 1996). Although considered to be a rare occurrence in children, the incidence of PDPH is actually between 10% and 50% in children aged 10 to 18 years (Oliver, 2002; Wee, 1996). The onset of symptoms from a PDPH typically occurs within 48 hours, with the hallmark symptom being a frontal or occipital headache that is postural. The cause of PDPH is most likely a persistent leakage of spinal fluid that causes a net decrease in CSF volume and intracranial pressure. The supine position helps to alleviate the symptoms of PDPH by decreasing the effect of gravity on the CSF leak. The size of the dural perforation is the primary predictor of the development of PDPH. To reduce the risk for PDPH, smaller-gauge needles are used, and the needle is inserted with the bevel parallel to the dura’s longitudinal fibers (Kokki and Hendolin, 1996). Electron microscopy has revealed that the collagen fibers of the dura are arranged in several layers, and that the thickness of the dura is more predictive of whether a leak will occur than the orientation of the needle’s bevel (Turnbull and Shepherd, 2003). This explains the unpredictability of PDPH.
If a diagnosis of PDPH is made, simple measures such as bed rest and hydration can decrease the volume of CSF loss. In addition, analgesics to reduce the headache and intravenous caffeine may be administered. Caffeine is effective because of its ability to cause cerebrovascular vasoconstriction, resulting in decreased cerebral blood flow. In one study, when caffeine was used prophylactically in adults, visual analog pain scores and analgesic demand after PDPH were lower (Yucel et al., 1999). There is no current pediatric dosage recommendation for caffeine. The oral dosage for adult patients is 300 to 500 mg once or twice a day (Turnbull and Shepherd, 2003). The intravenous formulation of caffeine is administered with sodium benzoate. The adult intravenous dosage is 500 mg. This may be repeated within 2 to 4 hours if the headache is unchanged after the first dose (Janssen et al., 2003).
If conservative measures to treat PDPH are ineffective after 48 hours, an epidural blood patch should be considered. This requires that blood be drawn sterilely from a peripheral vein. The blood is then injected into the epidural space under aseptic technique. An epidural blood patch is most effective 48 to 72 hours after the dural puncture, and it may be ineffective if performed immediately after dural tap because high leakage of CSF may interfere with blood clotting (Oliver, 2002). If a child is awake during the placement of an epidural blood patch, the practitioner should stop the injection once the child feels either discomfort or pressure in the back. If a child is anesthetized during the performance of an epidural blood patch, no more than 0.3 mL/kg of blood should be injected into the epidural space (Ylonen and Kokki, 2002).
Total spinal block with respiratory arrest and bradycardia is another complication of spinal anesthesia (Desparmet, 1990). The preganglionic sympathetic blockade that is commonly seen in adults secondary to a high spinal is not typically seen in children, particularly in infants (Oberlander et al., 1995; Finkel et al., 2003; Somri et al., 2003). Dohi and coworkers (1979)

Full access? Get Clinical Tree