Fig. 18.1
Injection of contrast medium

Fig. 18.2
Spread of contrast medium at C7 level
Pain relief is assessed 10, 20, and 30 min after the procedure. A diagnostic block is considered positive if it results in a minimum of 50 % pain reduction, measured on the VAS within 30 min. The level that responds with the largest pain reduction is selected for intervention.
Radiofrequency Treatment
A technique similar to the one for performing diagnostic nerve blocks is used for the interventions [24, 30]. The C-arm of the fluoroscopy unit (Philips BV 25, Eindhoven, the Netherlands) is positioned with the beam parallel to the axis of the intervertebral foramen (25–35° anteriorly and 10° caudally). The entry point is located by projecting a metal ruler over the caudal and posterior part of the foramen (Fig. 18.3). The 22-G cannula (SMK Pole needle 54 mm with 4 mm active tip, Cotop International BV, Amsterdam, the Netherlands) is introduced parallel to the beam, and, if necessary, the position is corrected in the superficial subcutaneous layers until the cannula was projected on the screen as a single dot (Fig. 18.4). In practice, this dot should lie directly over the dorsal portion of the intervertebral foramen at the transition between the middle and most caudal third. This position is chosen to avoid possible injection into the vertebral artery, which runs anterior to the ventral part of the foramen. The fluoroscope is then adjusted to the anterior–posterior view, and the cannula is inserted further until the tip projects over the middle of the facetal column (Fig. 18.5).


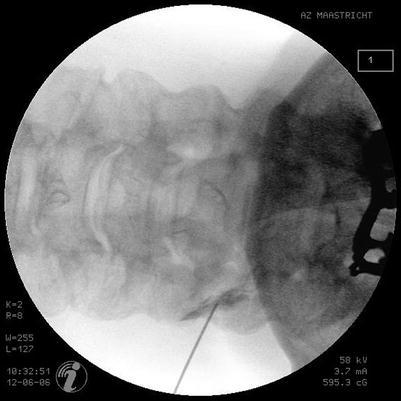

Fig. 18.3
Identification of the needle insertion point

Fig. 18.4
Radiofrequency lesion adjacent to the dorsal root ganglion (RF-DRG) 20° oblique, 10° caudocranial projection. The needle is positioned in the posterior aspect of the foramen, at the junction of the middle and caudal third part. It is projected as a dot in tunnel vision
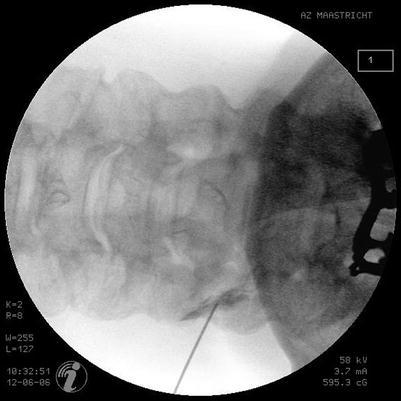
Fig. 18.5
RF-DRG AP view. The tip of the needle is projected over the facetal column
The stylet of the cannula is then replaced by the RF probe (SMK-TC 5, Radionics, Burlington, MA). After checking the impedance, indicating a normal, closed electrical circuit, stimulation is started at a frequency of 50 Hz to obtain a sensory stimulation threshold.
A paresthesia is elicited along the tested cervical nerve root at less than 0.5 V and is considered to indicate adequate proximity of the DRG [31].
The treatment can be performed using either conventional radiofrequency or pulsed radiofrequency current.
Radiofrequency current is applied in order to increase the temperature at the tip slowly to 67 °C. This temperature is maintained for 60 s.
The PRF current is applied during 120 s from the lesion generator (Radionics RFG 3 C Plus, Burlington, MA) as described by Sluijter et al. [27]. With the use of PRF the output is set at 45 V so that the temperature at the electrode tip does not exceed 40 °C.
Side Effects and Complications
The most frequently reported side effect with conventional radiofrequency treatment is a vague burning sensation in the treated dermatome. This pain usually subsided spontaneously 6 weeks after treatment. Also hyposensibility may be observed in the treated dermatome. Though rarely occurring, the most troublesome complication of conventional radiofrequency treatment is the deafferentation pain.
In the current experience with pulsed radiofrequency treatment adjacent to the cervical DRG, no side effects and complications have been reported.
Conclusions
Cervical radicular pain may be refractory to pharmacological treatment and rehabilitation. Before offering symptomatic treatment, infection and cancer (e.g., pancoast) should be excluded. After careful neurological examination, to rule out shoulder pathology, the causative level should be confirmed by means of diagnostic blocks. Epidural corticosteroid administration, by intralaminar or transforaminal route, may be a treatment option. There is however no comparison between both techniques, though the transforaminal administration route has gained in interest because it is supposed to deliver the drug as close as possible to the inflammatory nerve root [1, 32, 33] Recently published case reports on serious adverse events after transforaminal steroid administration at the cervical level urge for a cautious use of this treatment. Surgical techniques for decompression with or without anterior interbody fusion are often performed to reduce the pain and disability, but are associated with a small but definite risk [34]. A randomized controlled trial indicates that a multidisciplinary treatment with cognitive behavioral therapy and psychological interventions are preferred over surgery [35]. Systematic reviews showed that there is little evidence for better efficacy of surgery compared to cognitive behavioral treatment, justifying the higher risk for complications [34, 36].
The available evidence on radiofrequency treatment adjacent to the cervical DRG suggests pain relief and improved patient satisfaction. The evidence on PRF adjacent to the cervical DRG indicates potentially similar clinical results. The perceived better safety of the latter technique justifies trying this minimal invasive procedure prior to other interventional treatment options.
References
1.
2.
Bogduk N. Medical management of acute cervical radicular pain: and evidence-based approach. 1st ed. Newcastle: The Newcastle Bone and Joint Institute; 1999.
3.
Merskey H, Bogduk N. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of pain terms. 2nd ed. Seattle: IASP Press; 1994.
4.
Saal JS, Saal JA, Yurth EF. Nonoperative management of herniated cervical intervertebral disc with radiculopathy. Spine. 1996;21(16):1877–83.PubMedCrossRef

Full access? Get Clinical Tree








